Antiparkinsonism agents are drugs used for the management of signs and symptoms of Parkinson’s disease, a progressive, chronic neurological disorder primarily characterized by lack of coordination. Over time, individuals with Parkinson’s develop rigidity and weakness.
There is no known treatment for Parkinson’s as of present and drug therapy remains to be the primary treatment.
The goal of the therapy is to restore the balance between decreasing dopamine levels (has inhibitory effect on the neurons of the basal ganglia) and increasing cholinergic neurons (excitatory).
Table of Contents
- Antiparkinsonism Agents: Generic and Brand Names
- Disease Spotlight: Parkinson’s Disease and Parkinsonism
- Dopaminergic Agents
- Anticholinergic Agents
- Practice Quiz: Antiparkinsonism Agents
- Recommended Resources
- See Also
- References and Sources
Antiparkinsonism Agents: Generic and Brand Names
Here is a table of commonly encountered antiparkinsonism agents, their generic names, and brand names:
- Dopaminergic Agents
- amantadine (Symmetrel)
- apomorphine (Apokyn)
- bromocriptine (Parlodel)
- carbidopa-levodopa (Sinemet)
- levodopa (Dopar)
- ropinirole (Requip)
- Anticholinergic Agents
- benztropine (Cogentin)
- diphenhydramine (Benadryl)
- trihexyphenidyl (Artane)
- Others:
- entacapone (Comtan)
- tolcapone (Tasmar)
- selegiline (Carbex)
Disease Spotlight: Parkinson’s Disease and Parkinsonism
Parkinson’s Disease
- Parkinson’s Disease is a chronic, progressive neurological disorder with rhythmic tremors as its initial manifestation. These tremors lead to rigidity and weakness which interfere with the ability to maintain posture.
- Other manifestations include bradykinesia (extremely slowed movements), shuffling gait, drooling, and slow and slurred speech. Cranial nerve affectations lead to a mask-like expression.
- It is important to note that Parkinson’s does not affect the higher levels of cerebral cortex so intelligence and other brain functions at the same level are intact.
- The actual cause of Parkinson’s is not known but the manifestations are directly related to the damaged neurons in the basal ganglia of the brain. Neuronal damage is thought to be caused by viral infections, head trauma, brain infections, atherosclerosis, and drug and environmental exposures.
Parkinsonism
- Parkinsonism is referred to as the Parkinson’s disease-like extrapyramidal symptoms which are associated to particular drugs or brain injuries’ adverse effects.
Dopaminergic Agents
- Drugs that increase the effects of dopamine at receptor sites.
Therapeutic Action
The desired and beneficial actions of dopaminergics are as follows:
- Dopamine does not cross the blood-brain barrier so other drugs with actions similar to dopamine and those that increase its concentration in the substantia nigra (area responsible for muscle tone) must be used. This is one way of restoring the balance between stimulatory and inhibitory neurotransmitters.
- Levodopa, the precursor of dopamine is the mainstay of treatment for Parkinson’s. It crosses the blood-brain barrier and is converted into dopamine. When combined with carbidopa, the enzyme dopa decarboxylase is inhibited from metabolizing levodopa, leading to higher levels that can cross the barrier.
Indications
Dopaminergics are indicated for the following medical conditions:
- Dopaminergics are indicated for the relief of the signs and symptopms of idiopathic Parkinson’s disease.
- Levodopa is the drug of choice and acts as a replacement therapy.
- Amantadine is an antiviral drug that increases release of dopamine.
- Apomorphine directly binds with postsynaptic dopamine receptors.
Here are some important aspects to remember for indication of dopaminergics in different age groups:
Children
Safety and effectiveness of dopaminergics in children has not been established. Parkinson’s in children is very rare but they do experience parkinsonian symptoms because of other drugs. In this case, diphenhydramine is the drug of choice.
Adults
They must receive education about how to cope with the disease and the effects of the drugs. Herbal and alternative therapies should be mentioned to health care team because of drug interactions that may minimize effectiveness of therapy. Vitamin B6 can cause serious problems when taken with dopaminergics. Women of childbearing age should use contraception because of potential adverse effects to fetus. Lactating women should also use other method of feeding because of potential adverse effects to the baby.
Older adults
They are more susceptible to drug effects so dose for older adults need to be frequently adjusted. It can worsen other existing medical conditions like glaucoma and benign prostatic hypertrophy. An extensive written drug-teaching protocol is essential.
Pharmacokinetics
Here are the characteristic interactions of dopaminergics and the body in terms of absorption, distribution, metabolism, and excretion:
| Route | Onset | Peak | Duration |
| Oral | Varies | 0.5-2 h | 5 h |
| T1/2: 1-3 h Metabolism: liver Excretion: kidney (urine) |
Contraindications and Cautions
The following are contraindications and cautions for the use of dopaminergics:
- Allergy to dopaminergics. Prevent hypersensitivity reactions
- Angle-closure glaucoma. Can be exacerbated by drug effects
- Lactation. Can enter breast milk and cause adverse effects to the baby
- Pregnancy. Can enter
- Suspicious skin lesions. Levodopa is associated with development of melanoma
- CV disease, bronchial asthma, psychiatric disorders. Can be exacerbated by dopamine receptor stimulation
- Hepatorenal diseases. Can interfere with metabolism and excretion of drug
- Apomorphine can increase risk of hypotension and prolonged QT interval.
Adverse Effects
Use of dopaminergics may result to these adverse effects:
- CNS: anxiety, nervousness, headache, malaise, fatigue, confusion, mental changes, blurred vision, muscle twitching, and ataxia
- CV: arrhythmias, hypotension, palpitation
- Respiratory: bizarre breathing patterns
- GI: anorexia, nausea, vomiting, dysphagia, constipation or diarrhea
- GU: urinary retention
- Others: flushing, increased sweating, hot flashes
Interactions
The following are drug-drug interactions involved in the use of dopaminergics:
- MAOI: Increased therapeutic effects and risk of hypertensive crisis. MAOI should be stopped 14 days before beginning dopaminergic therapy.
- Vitamin B6, phenytoin: decreased levodopa efficacy
- Over-the-counter vitamins: decreased dopaminergic effectiveness
Nursing Considerations
Here are important nursing considerations when administering this drug:
Nursing Assessment
These are the important things the nurse should include in conducting assessment, history taking, and examination:
- Assess for mentioned contraindications and cautions (e.g. drug allergy, GI depression or obstruction, BPH, glaucoma) to prevent untoward complications.
- Perform a thorough physical assessment (e.g. CNS, respiratory status, vital signs, CV status, bowel sounds, urine output ) to obtain baseline data, determine drug therapy effectiveness, and monitor adverse effects.
- Assess skin for suspicious lesions if levodopa is to be given because it can cause or exacerbate melanoma.
- Assess for history of prolonged QT interval and obtain electrocardiogram if apomorphine is to be given to prevent further prolonged QT interval and serious arrhythmias.
- Monitor laboratory test results (liver and renal function, CBC) to determine need for possible dose adjustment and for evaluation of possible bone marrow suppression.
Nursing Diagnoses
Here are some of the nursing diagnoses that can be formulated in the use of this drug for therapy:
- Disturbed thought processes related to CNS effects
- Constipation related to dopaminergic effects
- Risk for urinary retention related to dopaminergic effects
- Risk for injury related to CNS effects and orthostatic hypotension
Implementation with Rationale
These are vital nursing interventions done in patients who are taking dopaminergics:
- Decrease dose of drug as ordered if therapy has been interrupted to prevent systemic dopaminergic effects.
- Evaluate disease progress and signs and symptoms periodically for reference of disease progress and drug response.
- Give drug with meals to alleviate GI irritation if present.
- Monitor bowel function and institute bowel program if constipation is severe.
- Have patient void before taking the drugs to decrease risk of urinary retention.
- Monitor laboratory test results (renal and liver function, CBC) to detect early signs of dysfunction.
- Provide comfort measures to help patient tolerate drug effects.
- Provide safety measures (e.g. adequate lighting, raised side rails, etc.) to prevent injuries.
- Educate client on drug therapy to promote understanding and compliance.
Evaluation
Here are aspects of care that should be evaluated to determine effectiveness of drug therapy:
- Monitor patient response to therapy (improvement in signs and symptoms of Parkinson’s disease).
- Monitor for adverse effects (e.g.CNS changes, urinary retention, GI depression, increased sweating and flushing, etc).
- Evaluate patient understanding on drug therapy by asking patient to name the drug, its indication, and adverse effects to watch for.
- Monitor patient compliance to drug therapy.
Anticholinergic Agents
- Anticholinergic agents are synthetic drugs which have been developed to achieve a greater affinity for cholinergic receptor sites in the CNS.
- Drugs that inhibit the effects of acetylcholine at receptor sites of substantia nigra and corpus striatum.
Therapeutic Action
The desired and beneficial actions of anticholinergic agents are as follows:
- Returns the balance to the basal ganglia and reduces the severity of rigidity, akinesia, and tremors.
- Peripheral anticholinergics reduce drooling and other secondary effects of parkinsonism.
Indications
Anticholinergic agents are indicated for the following medical conditions:
- Adjunctive therapy for Parkinson’s disease (idiopathic, atherosclerotic, and postencephalitic)
- Indicated for patients who no longer respond to levodopa.
Here are some important aspects to remember for indication of anticholinergic agents in different age groups:
Children
Safety and effectiveness of dopaminergics in children has not been established. Parkinson’s in children is very rare but they do experience parkinsonian symptoms because of other drugs. In this case, diphenhydramine is the drug of choice.
Adults
They must receive education about how to cope with the disease and the effects of the drugs. Herbal and alternative therapies should be mentioned to health care team because of drug interactions that may minimize effectiveness of therapy. Vitamin B6 can cause serious problems when taken with anticholinergics. Women of childbearing age should use contraception because of potential adverse effects to fetus. Lactating women should also use other method of feeding because of potential adverse effects to the baby.
Older adults
They are more susceptible to drug effects so dose for older adults need to be frequently adjusted. It can worsen other existing medical conditions like glaucoma and benign prostatic hypertrophy. An extensive written drug-teaching protocol is essential.
Pharmacokinetics
Here are the characteristic interactions of anticholinergic agents and the body in terms of absorption, distribution, metabolism, and excretion:
| Route | Onset | Peak | Duration |
| Oral | 1 h | Unknown | 6-10 h |
| IM, IV | 15 min | Unknown | 6-10 h |
| T1/2: Unknown Metabolism: liver Excretion: N/A |
Contraindications and Cautions
The following are contraindications and cautions for the use of anticholinergic agents:
- Allergy to dopaminergics. Prevent hypersensitivity reactions
- Angle-closure glaucoma, GI and GU obstruction, prostatic hypertrophy. Can be exacerbated by drug effects
- Myasthenia gravis. Exacerbated by acetylcholine receptor sites blocking effect of the drug
- Tachycardia, dysrhythmia, hyper or hypotension. Blocking the parasympathetic system may cause a dominance of sympathetic stimulatory activity
- Hepatic dysfunction. Interfere with the metabolism of drugs increasing risk of toxicity
- Lactation. Can enter breast milk and cause adverse effects to the baby
- Pregnancy. Can enter
Adverse Effects
Use of anticholinergic agents may result to these adverse effects:
- CNS: disorientation, confusion, memory loss, agitation, nervousness, delirium, dizziness, light-headedness, weakness
- CV: tachycardia, palpitations, hypotension
- EENT: blurred vision, photophobia, pupil dilation, blocking of lens accommodation
- GI: dry mouth, nausea, vomiting, paralytic ileus, constipation
- GU: urinary retention and hesitancy
- Others: flushing, reduced sweating
Interactions
The following are drug-drug interactions involved in the use of anticholinergic agents:
- TCAs, phenothiazines: increased risk of potentially fatal paralytic ileus and toxic psychoses
- Antipsychotics: decreased antipsychotic therapeutic effectiveness because of central antagonism of two agents
Nursing Considerations
Here are important nursing considerations when administering this drug:
Nursing Assessment
These are the important things the nurse should include in conducting assessment, history taking, and examination:
- Assess for mentioned contraindications and cautions (e.g. drug allergy, GI depression or obstruction, glaucoma, myasthenia gravis) to prevent untoward complications.
- Perform a thorough physical assessment (e.g. CNS, respiratory status, vital signs, CV status, bowel sounds, urine output) to obtain baseline data, determine drug therapy effectiveness, and monitor adverse effects.
- Monitor laboratory test results (liver and renal function) to determine need for possible dose adjustment.
Nursing Diagnoses
Here are some of the nursing diagnoses that can be formulated in the use of this drug for therapy:
- Disturbed thought processes related to CNS effects
- Impaired urinary elimination related to genitourinary effects
- Constipation related to GI effects
- Risk for impaired thermoregulation related to anticholinergic effects
- Risk for injury related to CNS effects
Implementation with Rationale
These are vital nursing interventions done in patients who are taking anticholinergics:
- Administer drug with caution for patients exposed in hot weather or environments because patients are at increased risk for heat prostration due to decreased ability to sweat.
- Give drug with meals to alleviate GI irritation if present.
- Monitor bowel function and institute bowel program if constipation is severe.
- Have patient void before taking the drugs to decrease risk of urinary retention.
- Monitor laboratory test results (renal and liver function) to detect early signs of dysfunction.
- Provide comfort measures to help patient tolerate drug effects.
- Provide safety measures (e.g. adequate lighting, raised side rails, etc.) to prevent injuries.
- Educate client on drug therapy to promote understanding and compliance.
- Evaluate disease progress and signs and symptoms periodically for reference of disease progress and drug response.
Evaluation
Here are aspects of care that should be evaluated to determine effectiveness of drug therapy:
- Monitor patient response to therapy (improvement in signs and symptoms of Parkinson’s disease).
- Monitor for adverse effects (e.g.CNS changes, urinary retention, GI depression, decreased sweating, etc).
- Evaluate patient understanding on drug therapy by asking patient to name the drug, its indication, and adverse effects to watch for.
- Monitor patient compliance to drug therapy.
Practice Quiz: Antiparkinsonism Agents
Let’s evaluate what you’ve learned in this nursing pharmacology study guide for antiparkinsonian agents.
1. What is the goal of therapy for Parkinson’s disease?
A. To decrease dopamine and to increase cholinergic neurons
B. To balance dopamine and cholinergic neurons
C. To excite neurons more
D. To inhibit neurons more
2. What is the mainstay of treatment for Parkinson’s?
A. Symmetrel
B. levodopa
C. Cogentin
D. Parlodel
3. The drug of choice in children with parkinsonian symptom.
A. levodopa
B. Artane
C. Benadryl
D. benztropine
4. Which can decrease efficacy of levodopa?
A. Phenytoin
B. Pyridoxine
C. Niacin
D. Both A and B
5. A construction worker for 10 years is about to receive anticholinergics. What should the nurse consider in handling this patient?
A. Do not give the drug to the patient.
B. Administer it with caution.
C. Discuss it with the doctor and have the order changed.
D. Arrange for a possible increase in the dose.
6. Which of the following is a contraindication for the use of anticholinergic agents?
A. Heart rate of 120 beats per minute
B. Myasthenia gravis
C. Active hepatitis B
D. All of the above.
Answers and Rationale
1. Answer: B. To balance dopamine (excitatory) and cholinergic neurons (inhibitory).
2. Answer: B. levodopa.
Levodopa, the precursor of dopamine is the gold standard of treatment for Parkinson’s. It crosses the blood-brain barrier and is converted into dopamine. When combined with carbidopa, the enzyme dopa decarboxylase is inhibited from metabolizing levodopa, leading to higher levels that can cross the barrier.
3. Answer: C. Benadryl.
Antiparkinsonism agents are generally not indicated for children. However, they experience parkinsonian symptoms due to other drugs. In this case, diphenhydramine (Benadryl) is the drug of choice.
4. Answer: D. Both A and B.
Both phenytoin and pyridoxine or Vitamin B6 can decrease the effectiveness of levodopa.
5. Answer: B. Administer it with caution.
Administer drug with caution for patients exposed in hot weather or environments because patients are at increased risk for heat prostration due to decreased ability to sweat.
6. Answer: D. All of the above.
Tachycardia, hepatic dysfunction, and myasthenia gravis are all contraindications for use of anticholinergics. Tachycardia will be stimulated more because parasympathetic system is blocked in the use of this drugs. Hepatic dysfunction can interfere with drug metabolism and may predispose patient to toxicity. Lastly, myasthenia gravis can be exacerbated because anticholinergics block acetylcholine receptor sites.
Recommended Resources
Our recommended nursing pharmacology resources and books:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase which will help support us. Thank you! For more information, check out our privacy policy.
Pharm Phlash! Pharmacology Flash Cards #1 BEST SELLER!
Test-yourself review cards put critical clinical information for nearly 400 of the top generic medications at your fingertips. And, you can count on them for accuracy, because each card is based on content from Davis’s Drug Guide for Nurses. Increase your test scores in pharmacology class.
Focus on Pharmacology (8th Edition)
Focus on Nursing Pharmacology makes challenging concepts more approachable. Engaging learning features cultivate your clinical application, critical thinking and patient education capabilities. This updated 8th edition builds on your knowledge of physiology, chemistry and nursing fundamentals to help you conceptualize need-to-know information about each group of drugs.
Pharmacology Made Incredibly Easy (Incredibly Easy! Series®)
Nursing pharmacology guide offers step-by-step guidance so you can grasp the fundamentals in enjoyable Incredibly Easy style. This is the perfect supplement to class materials, offering solid preparation for NCLEX® as well as a handy refresher for experienced nurses. Colorfully illustrated chapters offer clear, concise descriptions of crucial nursing pharmacology concepts and procedures.
Lehne’s Pharmacology for Nursing Care (11th Edition)
The Eleventh Edition of Lehne’s Pharmacology for Nursing Care provides a thorough understanding of key drugs and their implications for nursing care. This text, written by renowned nursing educators, helps you comprehend and apply pharmacology principles. A clear and engaging writing style simplifies complex concepts, making even the most challenging pharmacology content enjoyable. We recommend this book if you want a comprehensive nursing pharmacology guide.
Nursing Drug Handbook
Nursing2023 Drug Handbook delivers evidence-based, nursing-focused drug monographs for nearly 3700 generic, brand-name, and combination drugs. With a tabbed, alphabetical organization and a “New Drugs” section, NDH2023 makes it easy to check drug facts on the spot.

Pharmacology and the Nursing Process
The 10th edition of Pharmacology and the Nursing Process offers practical, user-friendly pharmacology information. The photo atlas contains over 100 unique illustrations and photographs depicting drug administration techniques. Updated drug content reflects the most recent FDA drug approvals, withdrawals, and therapeutic uses.

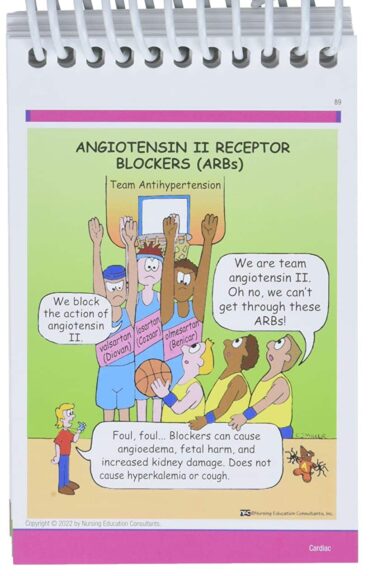
Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, and Memory Aids for Nurses
The 6th edition of Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, & Memory Aids for Nurses incorporates illustrations and humor to make studying easier and more enjoyable. This unique pharmacology review can be utilized as a spiral-bound notebook or as individual flashcards, making it ideal for mobile study.
See Also
Here are other nursing pharmacology study guides:
- Nursing Pharmacology – Study Guide for Nurses
Our collection of topics related to nursing pharmacology - Pharmacology Nursing Mnemonics & Tips
These nursing mnemonics aim to simplify the concepts of pharmacology through the use of a simple, concise guide. - Generic Drug Name Stems Cheat Sheet
Learn about these generic drug name stems to help you make sense of drugs easier! - Common Drugs and Their Antidotes
A guide to drug antidotes that nurses should be familiar about. - IV Fluids and Solutions Guide & Cheat Sheet
Get to know the different types of intravenous solutions or IV fluids in this guide and cheat sheet. - Drug Dosage Calculations NCLEX Practice Questions (100+ Items)
Care to take the challenge? This quiz aims to help students and registered nurses alike grasp and master the concepts of medication calculation.
Drug Guides NEW!
Individual drug guides and nursing considerations for the most common medications used in nursing pharmacology:
- Acetaminophen (Tylenol)
- Aspirin
- Atorvastatin (Lipitor)
- Enoxaparin (Lovenox)
- Furosemide (Lasix)
- Gabapentin
- Hydromorphone (Dilaudid)
- Lisinopril
- Metoprolol
- Morphine
Gastrointestinal System Drugs
Respiratory System Drugs
- Antihistamines
- Bronchodilators and Antiasthmatics
- Decongestants
- Expectorants and Mucolytics
- Inhaled Steroids
- Lung Surfactants
Endocrine System Drugs
- Adrenocortical Agents
- Antidiabetic Agents
- Glucose-Elevating Agents
- Hypothalamic Agents
- Insulin
- Parathyroid Agents: Bisphosphonates, Calcitonins
- Pituitary Drugs
- Sulfonylureas
- Thyroid Agents
Autonomic Nervous System Drugs
- Adrenergic Agonists (Sympathomimetics)
- Adrenergic Antagonists (Sympatholytics)
- Anticholinergics (Parasympatholytics)
- Cholinergic Agonists (Parasympathomimetics)
Immune System Drugs
Chemotherapeutic Agents
- Anthelmintics
- Anti-Infective Drugs
- Antibiotics
- Antifungals
- Antineoplastic Agents
- Antiprotozoal Drugs
- Antiviral Drugs
Reproductive System Drugs
Nervous System Drugs
- Antidepressants
- Antiparkinsonism Drugs
- Antiseizure Drugs
- Anxiolytics and Hypnotic Drugs
- General and Local Anesthetics
- Muscle Relaxants
- Narcotics, Narcotic Agonists, and Antimigraine Agents
- Neuromuscular Junction Blocking Agents
- Psychotherapeutic Drugs
Cardiovascular System Drugs
References and Sources
References and sources for this pharmacology guide for Antiparkinsonism Agents:
- Karch, A. M., & Karch. (2011). Focus on nursing pharmacology. Wolters Kluwer Health/Lippincott Williams & Wilkins. [Link]
- Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
- Lehne, R. A., Moore, L. A., Crosby, L. J., & Hamilton, D. B. (2004). Pharmacology for nursing care.
- Smeltzer, S. C., & Bare, B. G. (1992). Brunner & Suddarth’s textbook of medical-surgical nursing. Philadelphia: JB Lippincott.