Explore this comprehensive nursing care plan and management guide to effectively prevent falls among patients. Acquire essential knowledge about the nursing assessment, nursing diagnosis, and goals specifically tailored to patients who are at risk for falls.
Table of Contents
- What is fall risk?
- Factors that may cause falls
- Goals and outcomes
- Nursing assessment and rationales
- Nursing Interventions and Rationales
- Recommended Links
- Recommended Resources
- See also
- References and Sources
What is fall risk?
A fall is defined as an event that results in a person coming to rest inadvertently on the ground or floor or other lower level (WHO, 2021). Falls put a person at risk for serious injury and reduce their ability to remain independent.
According to the Centers for Disease Control and Prevention (CDC), falls are the leading cause of death among adults 65 and older, causing over 34,000 deaths for that age group. Falling is the second leading cause of death from unintentional injuries globally. Death from falls is a serious and endemic problem among older people. It is estimated that fall death rates in the U.S. have increased 30% from 2007 to 2016. If this rate continues, the CDC anticipates seven fall deaths every hour by 2030. Injuries from falls are costly and cause prolonged hospitalization for the older people. In 2015, the total medical costs for falls totaled more than $50 billion and over 3 million emergency room visits. Additionally, the quality of life after sustaining falls is significantly changed. Falls are the most common cause of traumatic brain injuries (TBI), and most hip fractures are caused by falling. Each year, over 800,000 patients are hospitalized because of falls.
Nurses play a major role in preventing falls for their patients through education, evaluating fall risk, creating safer environments, and providing interventions in preventing injuries from falls.
Factors that may cause falls
Several factors and conditions contribute to patient’s risk for falls, including the following:
Adults
- Aged 65 years and older; lower limb prosthesis; use of assistive devices such as walker, crane, and wheelchair; living alone
Children
- Less than 2 years of age; inadequate supervision of infants, toddlers, and preschoolers; insufficient safety guards on windows and heights
Lifestyle
- Unsafe workplaces such as buildings, bridges; insufficient safety equipment to protect workers from falls
Physiological
- Lower body weakness; vision problems; hearing impairment; foot condition; balance difficulty; postoperative patients, use of assistive devices for mobility
Emotional State
- Stressful situations can lessen a person’s ability to concentrate; depression
Environmental
- Environmental hazards such as clutter and throw rugs; insufficient lighting; broken or uneven steps that can cause tripping; unprotected creeks and landfills; unsecured swimming pools
Cognitive
- Impaired levels of alertness; alteration in cognitive abilities and functioning; lack of sleep; unconscious or semiconscious; disoriented and confused patients
Pharmaceutical Agents
- Polypharmacy; tranquilizers, narcotics, hypnotics, sedatives, or antidepressants, over-the-counter medicines that can affect balance and gait
Nursing Diagnosis Following a thorough assessment, a nursing diagnosis is formulated to specifically address the challenges associated with fall risk and fall prevention based on the nurse’s clinical judgement and understanding of the patient’s unique health condition. While nursing diagnoses serve as a framework for organizing care, their usefulness may vary in different clinical situations. In real-life clinical settings, it is important to note that the use of specific nursing diagnostic labels may not be as prominent or commonly utilized as other components of the care plan. It is ultimately the nurse’s clinical expertise and judgment that shape the care plan to meet the unique needs of each patient, prioritizing their health concerns and priorities. However, if you still find value in utilizing nursing diagnosis labels, here are some examples to consider:
- Risk for Falls related to advanced age (e.g., decreased muscle strength, slower reflexes, and visual or hearing impairments)
- Risk for Falls related to medication side effects (e.g., sedatives, antihypertensives)
- Risk for Falls related to environmental hazards (e.g., poor lighting, cluttered walkways)
- Risk for Falls related to cognitive impairment (e.g., dementia, delirium)
- Risk for Falls related to neurological disorders (e.g., Parkinson’s disease, stroke)
- Risk for Falls related to decreased sensory perception (e.g., neuropathy, vision loss)
Goals and outcomes
The individual will relate controlled falls or no falls, as evidenced by the following indicators:
- Patient will not sustain a fall.
- Patient will relate the intent to use safety measures to prevent falls.
- Patient will demonstrate selective prevention measures.
- Patient and caregivers will implement strategies to increase safety and prevent falls in the home.
Nursing assessment and rationales
Falls are due to several factors, and a holistic approach to the individual and environment is important. Suppose a person is considered at high risk for falls after the screening. In that case, a health professional should conduct a fall risk assessment to obtain a more detailed analysis of the individual’s risk of falling. A fall risk assessment requires using a validated tool that researchers have examined to be useful in naming the causes of falls in an individual. As a person’s health and circumstances change, reassessment is required.
Conducting fall risk assessment
1. Assess for circumstances associated with increasing the level of fall risk upon admission, following any alteration in the patient’s physical condition or cognitive status, whenever a fall happens, systematically during a hospital stay, or at defined times in long-term care settings:
The degree of fall risk can be determined using the assessment of intrinsic and extrinsic factors. Standard assessment tools can also be used (discussed below). The nurse should consider these factors when planning care for patients with fall risk.
1.1. Assess history of falls.
Individuals are more likely to fall again if they have sustained one or more falls in the past six months. The older population is at increased risk of fall-related readmissions based on a study identifying the factors predictive of repeat falls associated outcomes (Prabhakaran et al., 2020).
1.2. Assess mental status changes.
Persons with impaired awareness and disorientation may not understand where they are or what to do to help themselves. They may wander from one place to another that may jeopardize their safety. Additionally, confusion and impaired judgment increase the patient’s chance of falling.
1.3. Assess age-related physical changes.
The ability of people to protect themselves from falls is affected by such factors as age and development. Older people with weak muscles are more likely to fall than those who maintain muscle strength, flexibility, and endurance. These changes include reduced visual function, impaired color perception, change in center of gravity, unsteady gait, decreased muscle strength, decreased endurance, altered depth perception, and delayed response and reaction times.
In older adults with age-related macular degeneration, increased visual impairment was particularly associated with an increased incidence of falls and other injuries. Less contrast sensitivity was quite associated with both increased rates of falls and other injuries, while decreased visual acuity was only associated with increased fall rate (Wood et al., 2011).
1.4. Assess the patient for sensory deficits.
Sensory perception of environmental stimuli is paramount to safety. Vision and hearing impairment limit the patient’s ability to perceive hazards in the surroundings. Older people who lived in homes with dimly lit kitchens and clutters at entryways or backyards were found to be at a considerably greater risk for falls (Huang, 2004).
1.5. Assess the patient’s balance and gait.
Older adults who have poor balance or difficulty walking are more likely to fall. These problems may be associated with lack of exercise or a neurological cause, arthritis, or other medical conditions and treatments. An important risk factor highlighted in a study is that adults with rheumatoid arthritis are at high risk of falls, including swollen and tender lower extremity joints, fatigue, and use of psychotropic medications (Stanmore et al., 2013).
1.6. Assess the use of mobility assistive devices.
Inappropriate use, improper selection, and maintenance of mobility aids such as canes, walkers, and wheelchairs can increase energy expenditure, unsteady gait, overload, and joint damage and ultimately increase the patient’s risk for falls. Older adults who are frail and are not using ambulatory assistive devices fall more during their activities of daily living (Cruz et al., 2020). Education programs should be developed to encourage proper use of ambulatory-assistive devices by the frail elderly.
1.7. Assess for disease-related symptoms.
Increased incidence of falls has been demonstrated in people with symptoms such as orthostatic hypotension, reduced cerebral blood flow, impaired urinary elimination, edema, dizziness, weakness, fatigue, and confusion. Patients with certain diagnoses experienced more falls than others. For example, patients with stroke were more likely to fall than other patients, thereby lengthening their stay and increasing their medical costs during physical rehabilitation (Salamon et al., 2012). Patients with orthostatic hypotension whose blood pressure drops upon often standing experience light-headedness or dizziness that can cause falls.
1.8. Review the patient’s medications.
Risk factors for falls also include medication use such as antihypertensive agents, ACE-inhibitors, diuretics, tricyclic antidepressants, alcohol use, antianxiety agents, opiates, and hypnotics or tranquilizers. Older adults usually take various medications for multiple chronic conditions. Hospitalized older people taking medications are at increased risk for falls based on a study on the association between drug use and falls (Rhalimi & Jaecker, 2009). Drugs that affect BP and level of consciousness are associated with the highest fall risk.
Medications Causing High Risk for Falls
| Point Value (Risk Level) | Medication Class | Fall Risks |
|---|---|---|
| 3 (High) | Antipsychotics, anticonvulsants, and benzodiazepines | Sedation, dizziness, postural disturbances, altered gait and balance, and impaired cognition |
| 2 (Medium) | Antihypertensives, cardiac drugs, antiarrhythmics, and antidepressants | Induced orthostasis, impaired cerebral perfusion, and poor health status |
| 1 (Low) | Diuretics | Increased ambulation and induced orthostasis |
1.9. Assess for unsafe clothing.
Clothing and shoes that are poor fitting or overly tight can restrict the person’s movement and ambulation contributing to fall risk.
1.10. Evaluate the patient’s environment.
A fall is more likely to be experienced by an individual if the surroundings are unfamiliar, such as furniture and equipment placement in a certain area. Environmental hazards contribute to falls to a greater extent in older healthy people than in older frail people due to increased exposure to fall hazards with an increase in the proportion of such falls occurring outside the home (Lord et al., 2006).
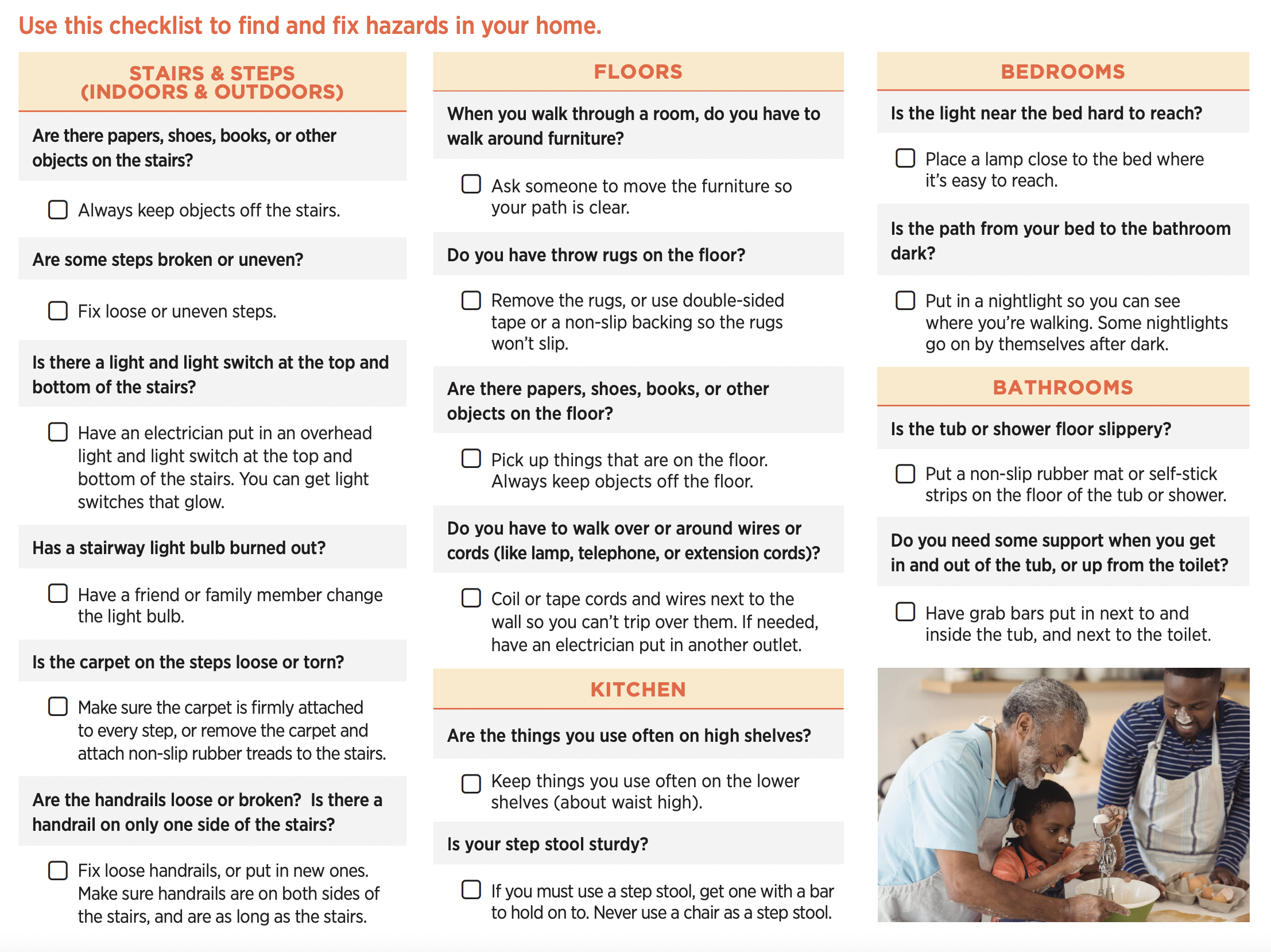
The nurse may need to assess the environment of the home, workplace, or community. In the home, clutter, throw rugs, light insufficiency, broken or uneven steps can cause tripping. Poor lighting, being in an unfamiliar environment, wet floors or surfaces, clutter, slippery floors, and obstacles on the floor all increase the patient’s fall risk. Workplaces that require stairs may also create occupational hazards in the workplace. In the community, inadequate street lighting or unprotected creeks and landfills may also cause accidents.
Fall risk assessment tools
2. Assess patient’s fall risk using Fall Risk Assessment Tool (FRAT).
Falls Risk Assessment Tool (FRAT) is a 4-item falls-risk screening tool for sub-acute and residential care. The FRAT has three sections: fall risk status, risk factor checklist, and action plan.
- Part 1: Fall Risk Status. A Fall Risk Status includes data about history of recent falls, medications, psychological and cognitive status of the patient.
- Part 2: Risk Factor Checklist. A Risk Factor Checklist includes vision, mobility, transfers, behaviors, activities of daily living (ADL’s), environment, nutrition, continence, and others.
- Part 3: Action Plan. An Action Plan involves clinical judgment and expertise when selecting core interventions to protect patients from falling, including individualized plans of care based on actual fall and injury risk factors.
3. Assess the patient’s fall risk using the Hendrich II Fall Risk Model (HIIFRM).
The Hendrich II Fall Risk Model determines risk for falling based on gender, mental and emotional status, symptoms of dizziness, and known categories of medications increasing risk. Each fall risk factor has assigned risk points set upon the study findings. If the patient scores on a risk factor, the corresponding number of points are counted to the patient’s fall risk score in the box to the far right. If a patient’s fall risk score totals five or higher, the person is at high risk for falls. If the patient scores only four points or lower, they are still at some risk of falling, and the nurse should use their best clinical assessment to manage all fall risk factors as part of a holistic care plan.
4. For pediatric clients assess sensory or motor deficits, recent illnesses, unsteady balance, running at speeds beyond capability, and inadequate supervision.
Assessment factors will assist in identifying appropriate interventions.
Nursing Interventions and Rationales
The following are the therapeutic and evidence-based nursing interventions and actions (including their rationales) for patients at risk for falls:
Fall risk interventions for adults in hospital or long-term care settings
1. Design an individualized plan of care for preventing falls. Provide a plan of care that is individualized to the patient’s unique needs.
Planning an individualized fall prevention program is essential for nursing care in any healthcare environment and needs a multifaceted approach. Avoid relying too much on universal fall precautions as different individuals have different needs. Universal fall precautions are established for all patients to reduce their risk of falling. These standard strategies, in general, help develop a safe environment that reduces accidental falls and delineates core preventive measures for all patients.
2. Provide signs or secure wristband identification for patients at risk for falls to remind healthcare providers to implement fall precaution behaviors.
Signs are vital for patients at risk for falls. Healthcare providers need to acknowledge who has the condition, for they are responsible for implementing actions to promote patient safety and prevent falls. When providing care, treatment, and services, use two patient identifiers. For example, wristbands should include the patient’s last and first name, date of birth, and NHS number in the UK. Details should be printed/written in black against a white background. Only red color should be used to signal special patient status. These recommendations are consistent with current developments in patient identification (Sevdalis et al., 2009).
3. Transfer the patient to a room near the nurses’ station.
Determining which patients are most likely to fall is essential to prepare and anticipate nearby location and provide more constant observation and quick response to call needs.
4. Place items the patient uses within easy reach, such as call light, urinal, water, and telephone.
Items that are too far may require the patient to reach out or ambulate unnecessarily and can potentially be a hazard or contribute to falls.
5. Respond to call light as soon as possible.
Helps prevent the patient from going out of bed without any assistance. Nurses respond to fallers’ call lights more quickly than they do to lights initiated by non-fallers. The nurses’ responsiveness to call lights could be a compensatory mechanism in responding to the fall prevalence on the unit (Tzeng & Yin, 2010). Additional effort is required to reach the ideal or even a reasonable level of patient safety-first practice in current hospital environments.
6. Avoid the use of physical restraints to reduce falls.
Studies demonstrate that regular use of restraints does not reduce the incidence of falls. The use of a trunk restraint is associated with a higher risk for falls and fractures among patients with either Alzheimer’s disease or dementia (Luo et al., 2011).
7. Inform the patient of the advantage of wearing eyeglasses and hearing aids. Encourage to have vision and hearing checked regularly.
Hazard can be reduced if the patient uses appropriate aids to promote visual and auditory orientation to the environment. Visual impairment can greatly cause falls.
8. Provide high-risk patients with a hip pad.
Hip pads, when worn properly, may reduce a hip fracture when fall happens.
9. Place beds are at the lowest possible position. Set the patient’s sleeping surface as near the floor as possible if needed.
Keeping the beds closer to the floor reduces the risk of falls and serious injury. Placing the mattress on the floor significantly reduces fall risk in some healthcare settings. Low beds are designed to lessen the distance a patient falls after moving out of bed. Although these beds don’t prevent a fall, they reduce the distance of a fall, reducing trauma and injury (Quigley et al., 2015).
10. For tall patients, avoid keeping the bed in a low position at all times.
Patients who are tall and with weak leg muscles who try to sit on the bed from a standing position are likely to fall onto the bed because it’s too low for them to lower themselves safely. Also, if a tall patient attempts to get up from a low bed without assistance, the patient is likely to fall back down onto the bed or miss the bed and fall onto the floor.
11. Secure bed and chair alarms when the patient gets up without support or assistance.
Bed alarms serve as early-warning systems to warn nursing staff that a patient is about to get up from bed without assistance. They’re designed to promote timely rescue, not to prevent falls from bed. Audible alarms can also remind the patient not to get up alone. The use of alarms can also be a substitute for physical restraints. Aside from bed alarms, increased supervision for high-risk patients also may help prevent falls.
12. Raise side rails on beds, as needed. For beds with split side rails, leave at least one of the rails at the foot of the bed down.
According to research, a disoriented or confused patient is less likely to fall when one of the four rails is left down.
13. Place a non-skid floor mat at the bedside.
Floor mats can serve as a cushion that helps reduce the impact of a possible fall.
14. Encourage the patient to don shoes or slippers with nonskid soles when walking.
As a person ages, gait becomes slower, and stride becomes shorter. Footwear influences balance and the subsequent risk of slips, trips, and falls by altering somatosensory feedback to the foot and ankle and modifying frictional conditions at the shoe/floor interface. Nonskid footwear provides sure footing for the patient with diminished foot and toe lift when walking. Shoes with low heels and a large contact area may aid older adults lessen the risk of a fall in everyday activities and settings (Tencer et al., 2004). A study likened slip resistance during mobilization, incline, and descent in patients with bare feet to patients wearing nonskid socks or compression stockings. Results showed bare feet provide better slip resistance than nonskid socks during mobilization and incline (Quigley et al., 2015; Chari et al., 2009).
15. For patients with shuffling gait or foot drop, avoid using nonskid socks.
Patients with a shuffling gait increase fall chances dramatically. To reduce fall risk, shoes should be with a little to no heel, thin soles with slip-resistant tread, and support the ankles.
16. Have the patient wear proper footwear.
Advise patient to use nonskid socks to prevent the feet from sliding upon standing. However, encourage patients to wear appropriate, well-fitting shoes—not nonskid socks for ambulation.
17. Improve home support.
Many community service organizations provide financial assistance to make older adults make safe environments in their homes.
18. Familiarize the patient with the layout of the room. Discourage rearranging the furniture in the room.
A fall is more likely to be experienced by an individual if the surrounding is not familiar, such as furniture and equipment placement in a certain area. The patient must get used to the room’s layout to avoid tripping over furniture or any large objects.
19. Teach patients how to safely ambulate at home, including using safety measures such as handrails in the bathroom.
Helps relieve anxiety at home and eventually decreases the risk of falls during ambulation in their home setting. Raised toilet seats can facilitate safe transfer on and off the toilet.
20. Use heavy furniture that will not tip over when used as support when ambulating. Make the primary path clear and as straight as possible. Avoid clutter on the floor surface.
Patients having difficulty balancing are not skilled at walking around certain objects that obstruct a straight path. Recognizing and fixing potential hazards and establishing assistive devices are effective fall prevention approaches that make the home environment safer for older adults. Safety experts and design engineers can collaborate with healthcare providers, homecare workers, and the older people to improve the home environment (Rogers et al., 2004).
21. Provide the patient with a chair with a firm seat and arms on both sides. Consider locked wheels as appropriate.
Chairs with firm seats and armrests are easier to get out of, especially for patients who experience weakness and impaired balance.
22. Provide appropriate room lighting, especially at night.
Patients, especially older adults, have reduced visual capacity. Lighting an unfamiliar environment helps increase visibility if the patient must get up at night. In a study, homes with adequate lighting report fewer falls (Ramulu et al., 2021). Improvement in lighting at home may reduce fall rates in older adults.
23. Provide the patient with assistive devices for transfer and ambulation.
The use of gait belts by all health care providers can promote safety when assisting patients with transfers from bed to chair. Assistive aids such as canes, walkers, and wheelchairs can improve patient stability and balance when ambulating.
24. Consider physical and occupational therapy sessions to assist with gait techniques.
Occupational therapy is defined as the therapeutic application of activities of daily living ADL (occupation) in an individual or group to develop and enhance participation in roles, habits, and routines at home, at school, in the workplace, in the community, and in other settings. These interventions enable individuals to integrate exercise into their day-to-day routine. Group exercises can be incredibly helpful for older people. Observing their peers when performing the exercises can attain progress in their reactions and behavior (Samardzic et al., 2020).
25. Acknowledge that when the patient attends to another task while walking, such as holding a cup of water, clothing, or supplies, they are more likely to fall.
Patients should avoid carrying different objects that could cause a higher risk for subsequent falls.
26. Limit use of wheelchairs as much as possible because they can serve as a restraint device.
Most people in wheelchairs do not move. Wheelchairs, unfortunately, serve as a restraint device
27. If the patient has a new onset of confusion (delirium), provide reality orientation when interacting. Have family bring in familiar items, clocks, and watches from home to maintain orientation.
Reality orientation can help prevent or decrease the confusion that increases the risk of falling for patients with delirium.
28. Ask the family to stay with the patient.
Helps prevent the patient from accidentally falling or pulling out tubes.
29. Consider using sitters for patients with impaired ability to follow directions.
Sitters are effective for guaranteeing a secure, protected, and safe environment. However, studies demonstrated very low-certainty evidence that sitters reduce fall risk in acute care hospitals and only moderate-certainty that alternatives like video monitoring can reduce sitter use without increasing fall risk, suggesting that sitters are not as useful as initially believed (Greely et al., 2020).
30. Refer the patient with musculoskeletal problems for diagnostic evaluation.
Patients with musculoskeletal problems such as osteoporosis are at increased risk for serious injury from falls. Musculoskeletal pain, explicitly general pain, is a fundamental risk factor for falls in older women with disabilities. The risk for recurrent falls and self-reported fractures due to falls was also heightened in women with musculoskeletal pain, almost invariably in women with general pain (Leveille et al., 2002). Bone mineral density testing will help identify the risk for fractures from falls. Physical therapy evaluation can identify problems with balance and gait that can increase a person’s fall risk.
31. Collaborate with other health care team members to assess and evaluate patients’ medications that contribute to falling. Examine peak effects for prescribed medications that affect the level of consciousness.
A review of the patient’s medications by the prescribing health care provider and the pharmacist can identify side effects and drug interactions that increase the patient’s fall risk. The more medications a patient takes, the greater the risk for side effects and interactions such as dizziness, orthostatic hypotension, drowsiness, and incontinence. Polypharmacy in older adults is a significant risk factor for falls. Fall Risk-Increasing Drugs (FRID) refers to the medications well-recorded to be associated with heightened fall risk. These comprise but are not limited to anti-hypertensives, anti-psychotics, narcotics, sedatives, and anticholinergics. For example, recent studies have revealed that long-term use of proton pump inhibitors (PPIs) increased the risk of falls (Lapumnuaypol et al., 2019).
32. Allow the patient to participate in a program of regular exercise and gait training.
Studies recommend exercises to strengthen the muscles, improve balance, and increase bone density. Increased physical conditioning reduces the risk for falls and limits injury that is sustained when fall transpires. Land and water-based exercise programs may be similarly beneficial on balance and gait and thereby reduce the risk for falls. Water exercise may contribute a positive benefit on balance and gait for women 65 years and older. Water-based exercise could be regarded as an alternate exercise activity for older people, significantly if land-based exercise is challenging due to chronic musculoskeletal conditions (Booth, 2004).
33. Encourage patient to do Chair Rise Exercise or Sit-to-Stand Exercise.
Chair Rise Exercise is a simple sit-to-stand exercise that helps strengthen the muscles in the thighs and buttocks and improves mobility and independence. The goal is to do Chair Rise exercises without using hands as the client becomes stronger. See resources section for a detailed instruction on how to perform Chair Rise exercise.
34. Explain the use of vitamin D supplements.
Vitamin D helps in maintaining postural balance, propulsion and improves executive functions and navigation abilities among older adults. Vitamin D supplementation determines gait performance and prevents the occurrence of falls and their complications among older adults (Annweiler et al., 2010). The prescription of at least 800 IU of vitamin D daily for older patients is a simple intervention that should be integrated into new methods for postural rehabilitation, primary and secondary fall prevention, strength training, integration of body schema, automation of gait, and adaptation to the environment
Interventions for children with fall risk
1. Promote necessary modifications in surroundings.
Keeping toys and other objects lying around on the floor can prevent children from possible falls and accidents.
2. Encourage parents or family members to improve window safety by installing window guards and raising awareness.
Incidences of children falling from balconies or windows are found to be high and usually result in severe injuries and death (Grivnan et al., 2017).
3. Teach parents or family members about safety and how to prevent accidents by using infant car seats, guard gates on stairs, and sunburn protection, life jackets, and helmets.
These measures are necessary to keep the child in a confined area and prevent falls and accidents.
4. Educate parents about the danger of using high chairs and walkers. Remind parents always to use the safety straps and keep a close eye on their children.
High chair and walker injuries can include pinches and falls. Walkers can cause severe accidents, such as a fall down a flight of stairs.
5. Encourage parents to train children in using staircases, elevated porches, and decks in the home.
With constant adult supervision, allow children to hold on to the rail and walk carefully down each step one at a time.
6. Inform parents to keep thinking ahead for new falling hazards that children may encounter.
Children will always be prone to falls and injuries despite carefully modifying the home with safety measures. Make sure to never leave children unattended at all times and use all the safety precautions provided.
Recommended Links
Here are some additional resources you can use to promote safety from falls.
- CDC’s STEADI: Older Adult Fall Prevention. Great resources from the CDC regarding fall prevention. Includes brochures for patients, families, and healthcare workers.
- World Health Organization’s Fact Sheet for Falls. A fact sheet that lists risk factors for falls.
- Fall Risk Assessment Tool (FRAT). Guide on how to use the FRAT tool in evaluating patient’s fall risk.
- Henrich II Fall Risk Model. More information on how to use the Henrich II Fall Risk Model – another tool used in evaluating a patient’s fall risk.
- Chair Rise Exercise. Step by step guide on how to perform Chair Rise Exercise.
Recommended Resources
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care
We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition)
Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales
Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care
Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health
Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

See also
Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ!
Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch. - Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing
Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
References and Sources
Recommended resources and references for this nursing care plan for Risk for Falls.
- Booth, C. E. (2004). Water exercise and its effect on balance and gait to reduce the risk of falling in older adults. Activities, adaptation & aging, 28(4), 45-57.
- Cedric Annweiler; Manuel Montero-Odasso; Anne M Schott; Gilles Berrut; Bruno Fantino; Olivier Beauchet (2010). Fall prevention and vitamin D in the elderly: an overview of the key role of the non-bone effects. , 7(1), 50–0.
- Chari, S., Haines, T., Varghese, P., & Economidis, A. (2009). Are non-slip socks really ‘non-slip’? An analysis of slip resistance. BMC geriatrics, 9(1), 1-6.
- Cruz, A. D. O., Santana, S. M. M., Costa, C. M., Gomes da Costa, L. V., & Ferraz, D. D. (2020). Prevalence of falls in frail elderly users of ambulatory assistive devices: a comparative study. Disability and Rehabilitation: Assistive Technology, 15(5), 510-514.
- Greeley, Adela M.; Tanner, Elizabeth P.; Mak, Selene; Begashaw, Meron M.; Miake-Lye, Isomi M.; Shekelle, Paul G. (2020). Sitters as a Patient Safety Strategy to Reduce Hospital Falls. Annals of Internal Medicine, 172(5), 317–. doi:10.7326/M19-2628
- Grivna, M., Al-Marzouqi, H. M., Al-Ali, M. R., Al-Saadi, N. N., & Abu-Zidan, F. M. (2017). Pediatric falls from windows and balconies: incidents and risk factors as reported by newspapers in the United Arab Emirates. World journal of emergency surgery, 12(1), 1-6.
- Haney, S. B., Starling, S. P., Heisler, K. W., & Okwara, L. (2010). Characteristics of falls and risk of injury in children younger than 2 years. Pediatric emergency care, 26(12), 914-918.
- Huang, H. C. (2004). A checklist for assessing the risk of falls among the elderly. The journal of nursing research: JNR, 12(2), 131-142.
- Lapumnuaypol, K., Thongprayoon, C., Wijarnpreecha, K., Tiu, A., & Cheungpasitporn, W. (2019). Risk of fall in patients taking proton pump inhibitors: a meta-analysis. QJM: An International Journal of Medicine, 112(2), 115-121.
- Leveille, S. G., Bean, J., Bandeen-Roche, K., Jones, R., Hochberg, M., & Guralnik, J. M. (2002). Musculoskeletal pain and risk for falls in older disabled women living in the community. Journal of the American Geriatrics Society, 50(4), 671-678.
- Lord, S. R., Menz, H. B., & Sherrington, C. (2006). Home environment risk factors for falls in older people and the efficacy of home modifications. Age and ageing, 35(suppl_2), ii55-ii59.
- Luo, H., Lin, M., & Castle, N. (2011). Physical restraint use and falls in nursing homes: a comparison between residents with and without dementia. American Journal of Alzheimer’s Disease & Other Dementias®, 26(1), 44-50.
- Prabhakaran, K., Gogna, S., Pee, S., Samson, D. J., Con, J., & Latifi, R. (2020). Falling again? Falls in geriatric adults—risk factors and outcomes associated with recidivism. Journal of surgical research, 247, 66-76.
- Quigley, P. (2015). Tailoring falls-prevention interventions to each patient. The American Nurse Today, 10(11), 8-10.
- Ramulu, P. Y., Mihailovic, A., Jian-Yu, E., Miller, R. B., West, S. K., Gitlin, L. N., & Friedman, D. S. (2021). Environmental features contributing to falls in persons with vision impairment: The role of home lighting and home hazards. American journal of ophthalmology.
- Rhalimi, M., Helou, R., & Jaecker, P. (2009). Medication use and increased risk of falls in hospitalized elderly patients. Drugs & aging, 26(10), 847-852.
- Rogers, M. E., Rogers, N. L., Takeshima, N., & Islam, M. M. (2004). Reducing the risk for falls in the homes of older adults. Journal of Housing for the Elderly, 18(2), 29-39.
- Salamon, L. A., Victory, M., & Bobay, K. (2012). Identification of patients at risk for falls in an inpatient rehabilitation program. Rehabilitation Nursing, 37(6), 292-297.
- Samardzic, V., Jaganjac, A., Kovacevic, K., & Kraljevic, B. (2020). Occupational therapy in fall prevention: case report. International journal of medical reviews and case reports.[Internet], 4(4), 103-7.
- Sevdalis, N., Norris, B., Ranger, C., Bothwell, S., & Wristband Project Team. (2009). Designing evidence-based patient safety interventions: the case of the UK’s National Health Service hospital wristbands. Journal of evaluation in clinical practice, 15(2), 316-322.
- Stanmore, E. K., Oldham, J., Skelton, D. A., O’Neill, T., Pilling, M., Campbell, A. J., & Todd, C. (2013). Risk factors for falls in adults with rheumatoid arthritis: a prospective study. Arthritis care & research, 65(8), 1251-1258.
- Tencer, A. F., Koepsell, T. D., Wolf, M. E., Frankenfeld, C. L., Buchner, D. M., Kukull, W. A., … & Tautvydas, M. (2004). Biomechanical properties of shoes and risk of falls in older adults. Journal of the American geriatrics society, 52(11), 1840-1846.
- Tzeng, H. M., & Yin, C. Y. (2010). Nurses’ response time to call lights and fall occurrences. Medsurg Nursing, 19(5), 266.
- Wood, J. M., Lacherez, P., Black, A. A., Cole, M. H., Boon, M. Y., & Kerr, G. K. (2011). Risk of falls, injurious falls, and other injuries resulting from visual impairment among older adults with age-related macular degeneration. Investigative ophthalmology & visual science, 52(8), 5088-5092.
- World Health Organization, World Health Organization. Ageing, & Life Course Unit. (2008). WHO global report on falls prevention in older age. World Health Organization.

Thank you for this! Definitely helps me in nursing school
Thanks for posting this! It helped me to understand nursing process a lot!
Thank you for this ! It really helped in refreshing my nursing process knowledge.
Thank you! I can always count on Nurseslabs to help me with my care plan!
Thank you for all your support :-)
This is brilliant, thank you so much.