Schizophrenia is a severe mental illness characterized by disruptions in thinking, perception, emotions, and social interactions. The disorder often emerges in late adolescence or early adulthood and can lead to significant impairments in a person’s ability to function in various aspects of life.
This nursing guide aims to provide a concise overview of schizophrenia, its symptoms, its different types, treatment, and nursing management.
Table of Contents
- What is Schizophrenia?
- Incidences
- Causes
- Signs and Symptoms
- Phases of Schizophrenia
- Types of Schizophrenia
- Diagnosis
- Medical Management
- Nursing Management
What is Schizophrenia?
Despite it being one of the most common psychiatric disorders, schizophrenia is usually misunderstood. Here is how it is described and defined:
- Schizophrenia refers to a group of severe, disabling psychiatric disorders marked by withdrawal from reality, illogical thinking, possible delusions and hallucinations, and emotional, behavioral, or intellectual disturbance.
- These disturbances last for at least six (6) months. The level of functioning in work, interpersonal relationships, and self-care is markedly below the level since the onset of symptoms.
- Have difficulty distinguishing reality from fantasy. Their speech and behavior may frighten or mystify those around them.
Incidences
Schizophrenia occurs in all societies without regard to class, color, and culture.
- It affects 1.1% of the population above age 18, which is estimated to be 51 million people worldwide.
- In the United States alone, 2 million Americans each year are affected, with 7.2 in 1000 persons developing it during their lifetime.
- Affects both men (late teens or early 20s) and women (mid-20s to early 30s) equally
- Prevalence is higher than diabetes mellitus, Alzheimer’s disease, and multiple sclerosis.
Causes
Like many diseases, schizophrenia is linked to various factors.
- The precise cause is unknown.
- There is currently no way to predict who will develop the disease.
- Genetic factors. It is believed that multiple genes (strongest evidence points to chromosomes 13 and 6) are involved in predisposition to schizophrenia. Other factors like prenatal infections, perinatal complications, and environmental stressors are also being studied. The manner of transmission of genetic predisposition is not clearly understood.
- Biochemical factors. Involves dopamine (the focus of most studies), serotonin, norepinephrine, and epinephrine. Excessive dopamine activity is linked to hallucinations, agitation, and delusion. High norepinephrine is linked to positive symptoms of schizophrenia.
- Other factors include structural brain abnormalities (e.g. enlarged ventricles), developmental (e.g. faulty neuronal connections), and other possible causes (e.g. maternal influenza during the second trimester of pregnancy, epilepsy of the temporal lobe, head injury, etc.)
Signs and Symptoms
Behaviors and functional deficiencies seen in schizophrenia vary widely among patients.
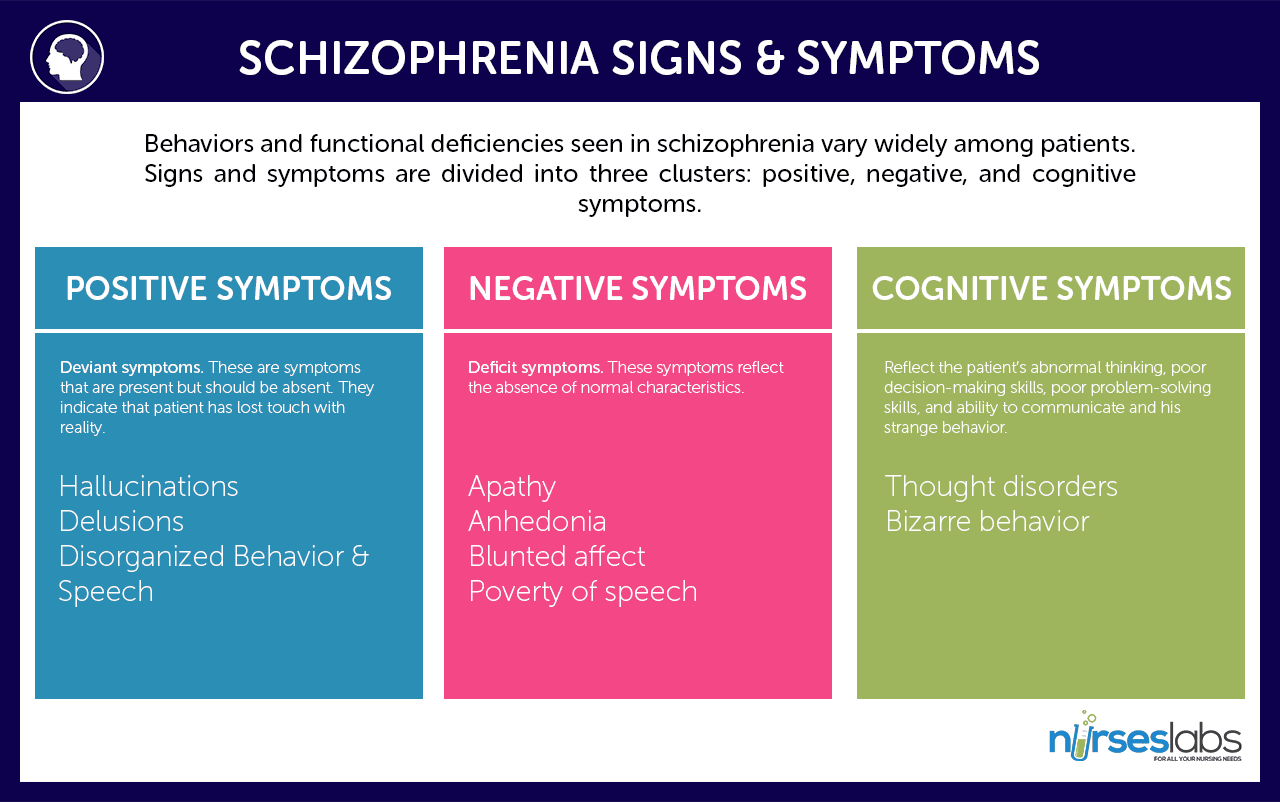
- Signs and symptoms are divided into three clusters: positive, negative, and cognitive symptoms.
- Positive symptoms are associated with temporal lobe abnormalities.
- Negative symptoms are associated with frontal cortex and ventricular abnormalities.
Positive Symptoms
- Deviant symptoms. These are symptoms that are present but should be absent. They indicate that the patient has lost touch with reality.
- Primarily include delusions and hallucinations.
- Hallucinations are the most common feature of schizophrenia. These involve hearing, seeing, smelling, tasting, and feeling touched by things in the absence of stimuli. An example is hearing voices that command the patient to do certain things, usually abusive and self-destructive.
- Delusions are fixed false beliefs. They cannot be changed by logic or persuasion. An example is a patient believing that people can read his mind. Several categories of delusions include:
- Persecutory delusions. Patient thinks he is being tormented, followed, tricked, or spied on.
- Reference delusions. Patient thinks that passages in books, music, TV shows, and other sources are directed at him.
- Delusions of thought withdrawal/thought insertion. Patient believes others can read his mind, his thoughts are being transmitted to others, or outside forces are imposing their thoughts or impulses on him.
Negative Symptoms
- Deficit symptoms. These symptoms reflect the absence of normal characteristics.
- Apathy is a lack of interest in people, things, and activities.
- Anhedonia is a diminished capacity to feel pleasure.
- Blunted affect is characterized by the patient’s face appearing immobile and inexpressive; this is the flattening of emotions and becomes more pronounced as the disease progresses.
- Poverty of speech is a speech that is brief and lacks content.
Cognitive Symptoms
- Reflect on the patient’s abnormal thinking, poor decision-making skills, poor problem-solving skills, ability to communicate, and strange behavior.
- Thought disorder is characterized by confused thinking and speech (e.g., incoherent ramblings, loose association, word salad, wandering).
- Bizarre behavior includes childlike silliness, laughing or giggling, agitation, inappropriate appearance, hygiene, and conduct.
Phases of Schizophrenia
Schizophrenia usually progresses through three distinct phases:
Prodromal Phase
- Occurs before hospitalization or within the year.
- Characterized by a clear decline from his previous level of functioning.
- May withdraw from friends and families and hobbies and interests, exhibit peculiar behavior, and deterioration in work and school performance.
Active Phase
- Commonly triggered by a stressful event
- Characterized by the presence of acute psychotic symptoms (e.g. hallucinations, delusions, incoherence, and catatonic behaviors).
- Prognosis worsens with each acute episode.
Residual Phase
- This is at this point in which the illness pattern is established, the disability level may be stabilized, and late improvements may occur.
Types of Schizophrenia
Schizophrenia is classified into five subtypes:
Paranoid
- Characterized by persecutory or grandiose delusional thought content and delusional jealousy.
- Stress may worsen patient symptoms.
- Experience frequent auditory hallucinations but lack symptoms of other subtypes like incoherence, loose associations, and affect problems.
- Tend to be less severely disabled than other schizophrenics and are more responsive to treatments.
Disorganized
- Marked by incoherent, disorganized speech and behaviors, and blunted or inappropriate affect.
- Usually includes extreme social impairment.
- Starts early and insidiously, with no significant remissions.
“Knowing that you’re crazy doesn’t make the crazy things stop happening.”
–Mark Vonnegut, The Eden Express: A Memoir of Insanity
Catatonic
- A rare disease form characterized by fixed stupor or positions for long periods and periodically yielding to brief spurts of extreme excitement.
- Increased potential for destructive, violent behaviors when agitated.
- They remain mute and have refusal to move about or tend to personal needs.
Undifferentiated
- Presence of schizophrenic symptoms such as delusions and hallucinations in patients who does not fall to the category of the other subtypes.
Residual
- Muted form of the disease that stops short of recovery.
- No prominent psychotic symptoms.
- Has history of acute schizophrenic episodes and persistence of negative symptoms.
Diagnosis
The basis for diagnosing schizophrenia is formed by mental status examination, psychiatry history, and careful clinical observation.
- Diagnostic test results. No definitive diagnostic tool for schizophrenia but certain tests like CT scans and MRIs may be ordered to rule out disorders that can cause psychosis (e.g. vitamin deficiencies and enlarged ventricles).
- Ventricular-brain ratio may find elevated VBR in schizophrenic patients. Brain scans reveal functional cerebral asymmetries in a reverse pattern.
Medical Management
Here’s how schizophrenia is medically managed:
- Drug Therapy. Schizophrenia is mainly treated by antipsychotic (neuroleptic) drugs.
- These prevent relapse of acute symptoms.
- Psychotic symptoms must be present 12 to 24 months before patients receive their first medical treatment.
- Examples of these drugs include the typical or conventional typical antipsychotic chlorpromazine (Thorazine) and the atypical
- Electroconvulsive Therapy. Rarely used but is for patients with acute schizophrenia and those who can’t tolerate or don’t respond to medication. It is effective in reducing depressive and catatonic symptoms of schizophrenia.
- Other treatments include compliance promotion programs, psychosocial treatment and rehabilitation, vocational counseling, supportive psychotherapy, and appropriate use of community resources.
Nursing Management
Here are the nursing responsibilities for taking care of patients with schizophrenia:
Nursing Assessment
- Recognize schizophrenia. Note characteristic signs and symptoms of schizophrenia (e.g., speech abnormalities, thought distortions, poor social interactions).
- Establish trust and rapport. Don’t tease or joke with patients. Expect that patient is going to put you through rigorous testing periods. Introduce yourself and explain your purpose.
- Maximize level of functioning. Assess the patient’s ability to carry out activities of daily living (ADLs).
- Assess positive symptoms. Assess for command hallucinations; explore answers. Assess if the client has a fragmented, poorly organized, well-organized, systematized, or extensive system of beliefs that are not supported by reality. Assess for pervasive suspiciousness about everyone and their actions (e.g., vigilant, blames others for consequences of own behavior, argumentative, threatening).
- Assess negative symptoms. Assess for the negative symptoms of schizophrenia (as mentioned above).
- Assess medical history. Assess if the client is on medications, what these are, and adherence to therapy.
- Assess support system. Determine whether the family is well informed about the disease. Does the family understand the need for medication adherence?
Nursing Diagnoses
- Impaired Physical Mobility related to depressive mood state and reluctance to initiate movement.
- Impaired Social Interaction related to problems in thought patterns and speech.
- Decreased Cardiac Output related to orthostatic hypotensive drug effects.
- Risk for Suicide related to impulsiveness and marked changes in behavior.
- Risk for Injury related to hallucinations and delusions.
- Risk for Imbalanced Nutrition: less than body requirements related to self-neglect and refusal for self-care.
Nursing Care Planning and Goals
Main Article: 6 Schizophrenia Nursing Care Plans
- Reduce severity of psychotic symptoms
- Prevent recurrence of acute episodes
- Meet patient’s’ physical and psychosocial needs
- Help patient gain optimum level of functioning
- Increase client’s compliance to treatment and nursing plan
Nursing Interventions
- Establish trust and rapport. Don’t touch client without telling him first what you are going to do. Use an accepting, consistent approach; short, repeated contacts are best until trust has been established. Language should be clear and unambiguous. Maintain a sense of hope for possible improvement, and convey this to the patient.
- Maximize level of functioning. Avoid promoting dependence by doing only what the patient can’t do for himself. Reward positive behavior and work with him to increase his personal sense of responsibility in improving functioning.
- Promote social skills. Provide support in assisting him to learn social skills.
- Ensure safety. Maintain a safe environment with minimal stimulation.
- Ensure adequate nutrition. Monitor patient’s nutritional status and if the patient thinks his food is poisoned, let him fix his own food if possible or offer him foods in closed containers that he can open. Institute suicide and/or homicide precautions as appropriate.
- Keep it real. Engage patient in reality-oriented activities that involve human contact (e.g., workshops, inpatient social skills training). Clarify private language, autistic inventions, or neologisms.
- Deal with hallucinations by presenting reality. Explore the content of hallucinations. Avoid arguing about the hallucinations. Tell them you do not see, hear, smell, or feel it but explain that you know that these hallucinations are real to him.
- Promote compliance and monitor drug therapy. Administer prescribed drugs and encourage the patient to comply. Ensure that patient is really taking the drug. Observe for manifestations that warrant hypersensitivity reactions and toxicity.
- Encourage family involvement. Involve family in patient treatment and teach members to recognize impending relapse (e.g. nervousness, insomnia, decreased ability to concentrate). Suggest ways how families can manage symptoms.
Evaluation
- Evaluate effectiveness of drug therapy (absence of acute episodes and psychotic symptoms).
- Evaluate compliance to health instructions (taking medications on time, showing independence in activities, involvement of family).
- Level of patient’s functioning (ability to engage in social interactions).
- Patient’s mental status (oriented to reality).
Documentation Guidelines
The following are to be documented in the patient’s chart:
- Document the assessed presenting signs and symptoms (e.g., positive and negative signs).
- In instituting suicide precaution, document behavior and your precautions.
- In instituting homicide precaution, document patient’s comment and who was notified. Be sure to notify the doctor and the potential victim.
- In using restraints, document time of application and release.
References
- Diagnostic and Statistical Manual of Mental Disorders (DSM-V-TR)
- Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales
- Straight A’s in Psychiatric & Mental Health Nursing: A Review Series
External Links & Further Reading
- Schizophrenia – National Institute of Mental Health – provides up to date information about Schizophrenia.
- Psychiatric Mental Health Nursing Success: A Q&A Review Applying Critical Thinking to Test Taking (Davis’s Success) – great if you’re reviewing for the NCLEX.
Its a great honour to have such information.. Thank you fr it all
Amazing! felt interested to study
This was very helpful, thank you
It very useful and amazing piece.Thanks
Need more info on Schizophrenia nursing care plan at workplace