Antihypertensive drugs affect different areas of blood pressure control so in most cases, these agents are combined for synergistic effect.
Ninety percent of cases of hypertension have no known cause. Therefore, the main action of antihypertensive agents is to alter the body’s regulating mechanisms (e.g. baroreceptors, renin-angiotensin-aldosterone system, etc.) responsible for maintaining normal blood pressure.
Different people have different responses towards hypertensive agents because hypertension is multifactorial. For an instance, the presence of comorbidities (e.g. diabetes, myocardial infarction, etc.) may make some antihypertensives not suitable for treatment.
Table of Contents
- Antihypertensive Agents: Generic and Brand Names
- Disease Spotlight: Hypertension
- ACE Inhibitors
- Angiotensin II-Receptor Blockers
- Calcium-Channel Blockers
- Vasodilators
- Practice Quiz: Antihypertensive Agents
- Recommended Resources
- See Also
- References and Sources
Antihypertensive Agents: Generic and Brand Names
Here is a table of commonly encountered antihypertensive drugs, their generic names, and brand names:
- Angiotensin-Converting Enzymes (ACE) Inhibitors
- benazepril (Lotensin)
- captopril (Capoten)
- enalapril (Vasotec IV)
- quinapril (Accupril)
- Angiotensin II-Receptor Blockers (ARBs)
- irbesartan (Avapro)
- losartan (Cozaar)
- telmisartan (Micardis)
- valsartan (Diovan)
- Calcium-Channel Blockers
- amlodipine (Norvasc)
- diltiazem (Diltiazem)
- nicardipine (Cardene)
- nifedipine (Adalat, Procardia)
- verapamil (Calan, Isoptin)
- Vasodilators
- hydralazine (Apresoline)
- minoxidil (Loniten)
- nitroprusside (Nitropress)
- Renin Inhibitors
- aliskiren (Tekturna)
Disease Spotlight: Hypertension
Hypertension affects 20% of the population of the United States alone.
Types
Ninety percent of these cases have no known cause and is termed as essential hypertension. Of this type, there is elevated total peripheral resistance. Also, the organs are perfused effectively and people with essential hypertension usually exhibit no symptoms. It is also the reason why hypertension is tagged as the “silent killer.”
Another type of hypertension called secondary hypertension is characterized by elevated blood pressure due to a known cause. For example, a tumor in the adrenal medulla called phaeochromocytoma can cause the organ to release a high amount of catecholamines, which greatly increase blood pressure.
Categories
In 2017, the American College of Cardiology and the American Heart Association revised their hypertension guidelines. The previous guidelines set the threshold at 140/90 mm Hg for younger people and 150/80 mm Hg for those ages 65 and older.
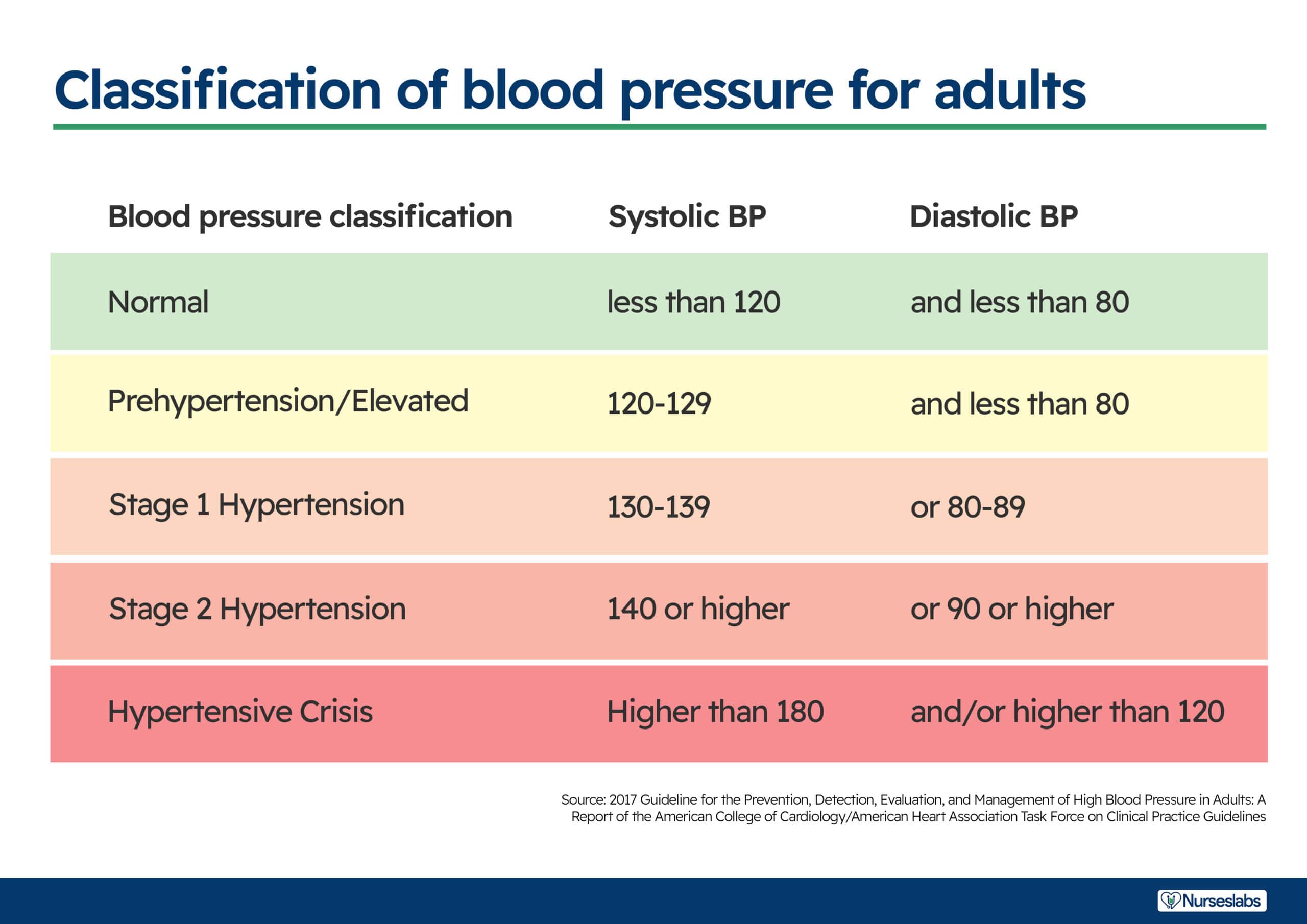
- Normal. The normal range for blood pressure is between, less than 120 mmHg and less than 80 mmHg.
- Elevated. Elevated stage starts from 120 mmHg to 129 mmHg for systolic blood pressure and less than 80 mmHg for diastolic pressure.
- Stage 1 hypertension. Stage 1 starts when the patient has a systolic pressure of 130 to 139 mmHg and a diastolic pressure of 80 to 89 mmHg.
- Stage 2 hypertension. Stage 2 starts when the systolic pressure is already more than or equal than 140 mmHg and the diastolic is more than or equal than 90 mmHg.
ACE Inhibitors
- Angiotensin-converting enzymes inhibitors (ACE Inhibitors) are antihypertensive agents that act in the lungs to prevent the conversion of angiotensin I into angiotensin II, which is a potent vasoconstrictor.
Therapeutic Action
- By preventing the production of angiotensin II which is a potent vasoconstrictor and a stimulator of aldosterone release, blood pressure is decreased with resultant loss of serum sodium and fluid but with a slight increase in serum potassium.
Indications
- Primarily indicated for hypertension and can be used alone or in combination with other drugs.
- Aside from its indication in treating hypertension, it is also combined with diuretics and digoxin in the treatment of heart failure and left ventricular dysfunction. The resultant effect is decreased in peripheral resistance and blood volume leading to decreased cardiac workload.
- It is also approved for treatment of diabetic nephropathy, in which the renal artery is being damaged by diabetes. It is thought that decreased in stimulation of angiotensin receptors in the kidney will slow down the damage in the renal artery.
- Children: safety and efficacy of ACE inhibitors has not been established in this age group.
- Adults: ACE inhibitors are not allowed during pregnancy.
- Older adults: are more susceptible to drug toxicity because of underlying conditions that would interfere with metabolism and excretion of drug. Renal and hepatic function should always be monitored.
Pharmacokinetics
| Route | Onset | Peak |
| Oral | 15 min | 30-90 min |
| T1/2: 2 h Metabolism: liver Excretion: urine |
Contraindications and Cautions
- Allergy to ACE inhibitors. Prevent severe hypersensitivity reactions.
- Renal impairment. Decreased renal blood flow effect of these drugs can exacerbate renal impairment.
- Heart failure. Changes in hemodynamics caused by these drugs can exacerbate heart failure.
- Hyponatremia and hypovolemia. Can be exacerbated by the therapeutic effects of the drug.
- Pregnancy and lactation. Can cause potential adverse effects to the fetus and can decrease milk production. Pregnant women are advised to use barrier type of contraceptives while taking this drug.
Adverse Effects
- GI: irritations, ulcer, constipation, liver injury
- GU: renal insufficiency, renal failure, proteinuria
- CV: reflex tachycardia, chest pain, heart failure, cardiac arrhythmias
- EENT: rash, alopecia, dermatitis, photosensitivity
- Captopril is associated with sometimes-fatal pancytopenia, cough, and GI distress.
Interactions
- Allopurinol: increased risk for hypersensitivity
- NSAIDs: increased risk for decreased antihypertensive effects
Nursing Considerations
Here are important nursing considerations when administering this drug:
Nursing Assessment
These are the important things the nurse should include in conducting assessment, history taking, and examination:
- Assess for the mentioned contraindications to this drug (e.g. renal impairment, hyponatremia, hypovolemia, etc.) to prevent potential adverse effects.
- Obtain baseline status for weight, vital signs, overall skin condition, and laboratory tests like renal and hepatic function tests, serum electrolyte, and complete blood count (CBC) with differential to assess patient’s response to therapy.
Nursing Diagnoses
Here are some of the nursing diagnoses that can be formulated in the use of this drug for therapy:
- Decreased cardiac output related to effect of drug in increasing fluid volume excretion
- Impaired skin integrity related to dermatological effects of the drug
- Increased risk for infection related to potential decreasing effect of drug to circulating blood cells
Implementation with Rationale
These are vital nursing interventions done in patients who are taking ACE inhibitors:
- Educate patient on importance of healthy lifestyle choices which include regular exercise, weight loss, smoking cessation, and low-sodium diet to maximize the effect of antihypertensive therapy.
- Administer drug on empty stomach one hour before or two hours after meal to ensure optimum drug absorption.
- Monitor renal and hepatic function tests to alert doctor for possible development of renal and/or hepatic failure as well as to signal need for reduced drug dose.
- Monitor for presence of manifestations that signal decreased in fluid volume (e.g. diarrhea, vomiting, dehydration) to prevent exacerbation of hypotensive effect of drug.
- Educate patient and family members about drug’s effect to the body and manifestations that would need reporting to enhance patient knowledge on drug therapy and promote adherence.
Evaluation
Here are aspects of care that should be evaluated to determine effectiveness of drug therapy:
- Monitor patient response to therapy through blood pressure monitoring.
- Monitor for adverse effects (e.g. hypotension, arrhythmias, renal failure, cough, and pancytopenia).
- Evaluate patient understanding on drug therapy by asking patient to name the drug, its indication, and adverse effects to watch for.
- Monitor patient compliance to drug therapy.
Angiotensin II-Receptor Blockers
- ARBs are antihypertensive agents that exert their action by blocking vasoconstriction and release of aldosterone through selective blocking of angiotensin II receptors in vascular smooth muscles and adrenal cortex.
Therapeutic Action
- The main action is to block the blood pressure raising effect of the renin-angiotensin-aldosterone system (RAAS).
Indications
- Like ACE inhibitors, they can also be used alone for treatment of hypertension or in combination with other antihypertensive agents.
- Utilized in treatment of heart failure for patients who do not respond to ACE inhibitors.
- By blocking the effects of angiotensin receptors in vascular endothelium, these drugs are able to slow down the progress of renal disease in patients with type 2 diabetes and hypertension.
- Children: safety and efficacy of ARBs has not been established in this age group.
- Adults: ARBs are not allowed during pregnancy.
- Older adults: are more susceptible to drug toxicity because of underlying conditions that would interfere with metabolism and excretion of drug. Renal and hepatic function should always be monitored.
Pharmacokinetics
| Route | Onset | Peak | Duration |
| Oral | Varies | 1-3 h | 24 h |
| T1/2: 2 h Metabolism: liver Excretion: urine and feces |
Contraindications and Cautions
- Allergy to ARBs. Prevent severe hypersensitivity reactions.
- Renal and hepatic impairment. Can alter metabolism and excretion of drugs which can increase the risk for toxicity.
- Hypovolemia. Can be exacerbated by the drug’s action on blocking important life-saving compensatory mechanisms.
- Pregnancy and lactation. Can cause potential adverse effects to the fetus and potential termination of pregnancy between second and third trimester. It is still not known whether ARBs can enter breast milk but it is generally not allowed in lactating women because of potential adverse effects to the neonate.
Adverse Effects
- CNS: headache, dizziness, syncope, weakness
- Respiratory: symptoms of upper respiratory tract infections (URTI), cough
- GI: diarrhea, abdominal pain, nausea, dry mouth, tooth pain
- EENT: rash, alopecia, dry skin
Interactions
- Phenobarbital, indomethacin, rifamycin: loss of effectiveness of ARBs
- Ketoconazole, fluconazole, diltiazem: decreased antihypertensive effects of ARBs
Nursing Considerations
Here are important nursing considerations when administering ARBs:
Nursing Assessment
These are the important things the nurse should include in conducting assessment, history taking, and examination:
- Assess for the mentioned contraindications to this drug (e.g. drug allergy, hypovolemia, renal impairment, etc.) to prevent potential adverse effects.
- Obtain baseline status for weight, vital signs, overall skin condition, and laboratory tests like renal and hepatic function tests, and serum electrolyte to assess patient’s response to therapy.
Nursing Diagnoses
Here are some of the nursing diagnoses that can be formulated in the use of this drug for therapy:
- Ineffective tissue perfusion related to fluid excretory effect of the drug
- Impaired skin integrity related to dermatological effects of the drug
- Risk for injury related to CNS side effects of the drug
Implementation with Rationale
These are vital nursing interventions done in patients who are taking ARBs:
- Educate patient on importance of healthy lifestyle choices which include regular exercise, weight loss, smoking cessation, and low-sodium diet to maximize the effect of antihypertensive therapy.
- Administer drug with food to prevent GI distress associated with drug intake.
- Monitor renal and hepatic function tests to alert doctor for possible development of renal and/or hepatic failure as well as to signal need for reduced drug dose.
- Provide comfort measures (e.g. quiet environment, relaxation techniques, etc.) to help patient tolerate drug effects.
- Educate patient and family members about drug’s effect to the body and manifestations that would need reporting to enhance patient knowledge on drug therapy and promote adherence.
Evaluation
Here are aspects of care that should be evaluated to determine effectiveness of drug therapy:
- Monitor patient response to therapy through blood pressure monitoring.
- Monitor for adverse effects (e.g. skin reactions, cough, headache, etc.)
- Evaluate patient understanding on drug therapy by asking patient to name the drug, its indication, and adverse effects to watch for.
- Monitor patient compliance to drug therapy.
Calcium-Channel Blockers
- Calcium-channel blockers as antihypertensive agents decrease blood pressure, cardiac workload, and myocardial consumption of oxygen.
- Since these drugs can significantly decrease cardiac workload, they are effective in treatment of angina.
Therapeutic Action
- These drugs inhibit the movement of calcium ions across myocardial and arterial muscle cell membranes. As a result, action potential of these cells are altered and cell contractions are blocked.
- Resultant effects include: depressed myocardial contractility, slow cardiac impulse in conductive tissues, and arterial dilation and relaxation.
Indications
- Like ACE inhibitors and ARBs, they can also be used alone for treatment of hypertension or in combination with other antihypertensive agents.
- Extended-release preparations are usually indicated for hypertensions in adults.
- Children: calcium-channel blockers is the drug group that is first considered in cases of hypertension in this age group that needs drug therapy.
- Adults: these drugs are not allowed during pregnancy.
- Older adults: are more susceptible to drug toxicity because of underlying conditions that would interfere with metabolism and excretion of drug. Renal and hepatic function should always be monitored.
Pharmacokinetics
| Route | Onset | Peak | Duration |
| Oral and extended release | 30-60 min | 6-11 h | 12 h |
| T1/2: 5-7 h Metabolism: liver Excretion: urine |
Contraindications and Cautions
- Allergy to calcium-channel blockers. Prevent severe hypersensitivity reactions.
- Heart block (sick sinus syndrome). Can be exacerbated by conduction-slowing effect of the drug.
- Renal and hepatic impairment. Can alter metabolism and excretion of drugs which can increase the risk for toxicity.
- Pregnancy and lactation. Can cause potential adverse effects to the fetus and should not be used unless the benefit to the mother clearly outweighs the risk to the fetus. It is not clear whether this drug can enter breast milk so another method of feeding is implemented for lactating mothers who are taking this drug.
Adverse Effects
- CNS: headache, dizziness, light-headedness, fatigue
- CV: hypotension, bradycardia, peripheral edema, heart block
- GI: nausea, hepatic injury
- EENT: rash, skin flushing
Interactions
- Increased serum level and toxicity of cyclosporine if taken with diltiazem.
- Grapefruit juice can increase serum level and toxicity of calcium-channel blockers.
Nursing Considerations
Here are important nursing considerations when administering calcium-channel blockers:
Nursing Assessment
These are the important things the nurse should include in conducting assessment, history taking, and examination:
- Assess for the mentioned contraindications to this drug (e.g. headache, rash, bradycardia, etc.) to prevent potential adverse effects.
- Monitor cardiopulmonary status closely as the drug can cause severe effects on these two body systems.
Nursing Diagnoses
Here are some of the nursing diagnoses that can be formulated in the use of this drug for therapy:
- Decreased cardiac output related to hypotension and vasodilating effect of the drug
- Risk for injury related to cardiovascular and CNS adverse drug effects
Implementation with Rationale
These are vital nursing interventions done in patients who are taking calcium-channel blockers:
- Educate patient on importance of healthy lifestyle choices which include regular exercise, weight loss, smoking cessation, and low-sodium diet to maximize the effect of antihypertensive therapy.
- Monitor blood pressure and heart rate and rhythm to detect possible development of adverse effects.
- Provide comfort measures for the patient to tolerate side effects (e.g. small frequent meals for nausea, limiting noise and controlling room light and temperature to prevent aggravation of stress which can increase demand to the heart, etc.)
- Educate patient and family members about drug’s effect to the body and manifestations that would need reporting to enhance patient knowledge on drug therapy and promote adherence.
- Emphasize to the client the importance of strict adherence to drug therapy to ensure maximum therapeutic effects.
Evaluation
Here are aspects of care that should be evaluated to determine effectiveness of drug therapy:
- Monitor patient response to therapy through blood pressure monitoring.
- Monitor for presence of mentioned adverse effects.
- Monitor for effectiveness of comfort measures.
- Monitor for compliance to drug therapy regimen.
- Monitor laboratory tests.
Vasodilators
- Direct vasodilators are used when the previous drugs mentioned are not effective.
- These antihypertensive agents are reserved for severe hypertension and hypertensive emergencies.
Therapeutic Action
- These antihypertensive agents exert their effect by acting directly on smooth muscles. Consequently, there will be muscle relaxation and vasodilation. Both of these will cause drop in blood pressure.
Indications
- As mentioned, these drugs are only used for hypertension cases that do not respond to other drug therapies.
- Nitroprusside is used in maintaining controlled hypotension during surgery.
- Nitroprusside is administered intravenously; hydralazine is available for oral, intravenous, and intramuscular use; and minoxidil is available for oral use only.
Pharmacokinetics
| Route | Onset | Peak | Duration |
| IV | 1-2 min | Rapid | 1-10 min |
| T1/2: 2 min Metabolism: liver Excretion: urine |
Contraindications and Cautions
- Allergy to direct vasodilators. Prevent severe hypersensitivity reactions.
- Cerebral insufficiency. Can be exacerbated by drug’s action to cause sudden drop in blood pressure.
- Peripheral vascular disease, CAD, heart failure, tachycardia. These conditions can be exacerbated by sudden drop in blood pressure.
- Pregnancy and lactation. Can cause potential adverse effects to the fetus and should not be used unless the benefit to the mother clearly outweighs the risk to the fetus. The drug can enter the breast milk and can cause potential adverse effects to the neonate. If needed by lactating mothers, another method of feeding is instituted.
Adverse Effects
- CNS: headache, dizziness, anxiety
- CV: reflex tachycardia, heart failure, edema, chest pain
- GI: nausea, vomiting, GI upset
- EENT: rash, lesions (e.g. minoxidil is associated with abnormal hair growth.)
- Nitroprusside is metabolized into cyanide so it can cause cyanide toxicity characterized by dyspnea, ataxia, loss of consciousness, distant heart sounds, and dilated pupil.
- Nitroprusside suppresses iodine uptake which leads to development of hypothyroidism.
Interactions
- Each drug in this group act differently on the body so each drug should be checked for potential drug-to-drug and drug-to-food interactions.
Nursing Considerations
Here are important nursing considerations when administering direct vasodilators:
Nursing Assessment
These are the important things the nurse should include in conducting assessment, history taking, and examination:
- Assess for the mentioned contraindications to this drug (e.g. drug allergy, CAD, cerebral insufficiency etc.) to prevent potential adverse effects.
- Obtain baseline status for weight, vital signs, overall skin condition, and laboratory tests like renal and hepatic function tests, and serum electrolyte to assess patient’s response to therapy.
Nursing Diagnoses
Here are some of the nursing diagnoses that can be formulated in the use of this drug for therapy:
- Decreased tissue perfusion related to changes in volume of blood pumped out by the heart
- Acute pain related to GI distress, headache, and skin effects of the drug
Implementation with Rationale
These are vital nursing interventions done in patients who are taking vasodilators:
- Educate patient on importance of healthy lifestyle choices which include regular exercise, weight loss, smoking cessation, and low-sodium diet to maximize the effect of antihypertensive therapy.
- Monitor blood pressure and heart rate and rhythm closely to evaluate for effectiveness and ensure quick response if blood pressure falls rapidly or too much.
- Provide comfort measures for the patient to tolerate side effects (e.g. small frequent meals for nausea, limiting noise and controlling room light and temperature to prevent aggravation of stress which can increase demand to the heart, etc.)
- Monitor patient for any manifestations that could decrease fluid volume inside the body (e.g. vomiting, diarrhea, excessive sweating, etc.) to detect and treat excessive hypotension.
- Educate patient and family members about drug’s effect to the body and manifestations that would need reporting to enhance patient knowledge on drug therapy and promote adherence.
- Emphasize to the client the importance of strict adherence to drug therapy to ensure maximum therapeutic effects.
Evaluation
Here are aspects of care that should be evaluated to determine effectiveness of drug therapy:
- Monitor patient response to therapy through blood pressure monitoring.
- Monitor for presence of mentioned adverse effects (e.g. hypotension, GI distress, skin reactions, etc.)
- Monitor for effectiveness of comfort measures.
- Monitor for compliance to drug therapy regimen.
- Monitor laboratory tests.
Practice Quiz: Antihypertensive Agents
Quiz time! Just how much you’ve learned from our nursing pharmacology study guide for Antihypertensive Agents? Take the 5-item quiz below and find out!
1. The three primary elements that determine the pressure in the cardiovascular system are heart rate, stroke volume, and:
A. Baroreceptors
B. Peripheral resistance
C. Renin-Angiotensin-Aldosterone System (RAAS)
D. All of the above
2. Untreated hypertension can result to which of the following:
A. Stroke
B. Renal failure
C. Loss of vision
D. All of the above
3. A student nurse was asked to take the blood pressure of a patient in the emergency room. The BP reads 140/90 mmHg. She would be correct to say that this BP belongs to ____________ classification.
A. Normal
B. Elevated
C. Stage 1 Hypertension
D. Stage 2 Hypertension
4. Which of the following medications will decrease the therapeutic effects of quinapril (Accupril)?
A. NSAIDs
B. Allopurinol
C. Antacids
D. All of the above
5. A patient receiving nitroprusside begun manifesting headache, distant heart sounds, imperceptible pulses, and shallow breathing. The nurse knows that these are signs of?
A. Reflex tachycardia
B. Hypothyroidism
C. Cyanide toxicity
D. Severe alteration of blood pressure
Answers and Rationale
1. Answer: B. Peripheral resistance.
Small arterioles help regulate blood pressure in a constant basis and are the most important factor affecting peripheral resistance. When small arterioles constrict, they are almost able to stop the flow of the blood. Their high responsiveness to sympathetic nervous stimulation cause them to constrict and increase blood pressure. Baroreceptors are pressure receptors located in the arch of the aorta and carotid arteries that send information to the brain when pressure increases. RAAS is a compensatory mechanism activated in the kidney when blood pressure falls.
2. Answer: D. All of the above.
The force of the blood propelled against blood vessels can damage their linings, making them susceptible to atherosclerosis and narrowing. When these happen, tiny vessels in the retina, kidneys, and brain can be destroyed leading to unresponsiveness of the system.
3. Answer: D. Stage 2 Hypertension
A category rating the severity of hypertension has been devised and the classifications of blood pressure are as follows: Normal – systolic: <120 mmHg; diastolic: <80 mmHg; Elevated – systolic: 120-129 mmHg; diastolic: <80 mmHg; Stage 1 Hypertension – systolic: 130-139 mmHg; diastolic: 80-89 mmHg; Stage 2 Hypertension – systolic: less than or equal to 140 mmHg; diastolic: less than or equal to 90 mmHg.
4. Answer: A. NSAIDs.
Quinapril belongs to the class ACE inhibitors. NSAIDs are linked to decreased antihypertensive effects of ACE inhibitors. Allopurinol increases risk of hypersensitivity when combined with ACE inhibitors.
5. Answer: C. Cyanide toxicity.
Nitroprusside is metabolized into cyanide. Other manifestations of cyanide toxicity include pink color, loss of consciousness, and absence of reflexes.
Recommended Resources
Our recommended nursing pharmacology resources and books:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase which will help support us. Thank you! For more information, check out our privacy policy.
Pharm Phlash! Pharmacology Flash Cards #1 BEST SELLER!
Test-yourself review cards put critical clinical information for nearly 400 of the top generic medications at your fingertips. And, you can count on them for accuracy, because each card is based on content from Davis’s Drug Guide for Nurses. Increase your test scores in pharmacology class.

Focus on Pharmacology (8th Edition)
Focus on Nursing Pharmacology makes challenging concepts more approachable. Engaging learning features cultivate your clinical application, critical thinking and patient education capabilities. This updated 8th edition builds on your knowledge of physiology, chemistry and nursing fundamentals to help you conceptualize need-to-know information about each group of drugs.

Pharmacology Made Incredibly Easy (Incredibly Easy! Series®)
Nursing pharmacology guide offers step-by-step guidance so you can grasp the fundamentals in enjoyable Incredibly Easy style. This is the perfect supplement to class materials, offering solid preparation for NCLEX® as well as a handy refresher for experienced nurses. Colorfully illustrated chapters offer clear, concise descriptions of crucial nursing pharmacology concepts and procedures.
Lehne’s Pharmacology for Nursing Care (11th Edition)
The Eleventh Edition of Lehne’s Pharmacology for Nursing Care provides a thorough understanding of key drugs and their implications for nursing care. This text, written by renowned nursing educators, helps you comprehend and apply pharmacology principles. A clear and engaging writing style simplifies complex concepts, making even the most challenging pharmacology content enjoyable. We recommend this book if you want a comprehensive nursing pharmacology guide.

Nursing Drug Handbook
Nursing2023 Drug Handbook delivers evidence-based, nursing-focused drug monographs for nearly 3700 generic, brand-name, and combination drugs. With a tabbed, alphabetical organization and a “New Drugs” section, NDH2023 makes it easy to check drug facts on the spot.

Pharmacology and the Nursing Process
The 10th edition of Pharmacology and the Nursing Process offers practical, user-friendly pharmacology information. The photo atlas contains over 100 unique illustrations and photographs depicting drug administration techniques. Updated drug content reflects the most recent FDA drug approvals, withdrawals, and therapeutic uses.

Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, and Memory Aids for Nurses
The 6th edition of Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, & Memory Aids for Nurses incorporates illustrations and humor to make studying easier and more enjoyable. This unique pharmacology review can be utilized as a spiral-bound notebook or as individual flashcards, making it ideal for mobile study.

See Also
Here are other nursing pharmacology study guides:
- Nursing Pharmacology – Study Guide for Nurses
Our collection of topics related to nursing pharmacology - Pharmacology Nursing Mnemonics & Tips
These nursing mnemonics aim to simplify the concepts of pharmacology through the use of a simple, concise guide. - Generic Drug Name Stems Cheat Sheet
Learn about these generic drug name stems to help you make sense of drugs easier! - Common Drugs and Their Antidotes
A guide to drug antidotes that nurses should be familiar about. - IV Fluids and Solutions Guide & Cheat Sheet
Get to know the different types of intravenous solutions or IV fluids in this guide and cheat sheet. - Drug Dosage Calculations NCLEX Practice Questions (100+ Items)
Care to take the challenge? This quiz aims to help students and registered nurses alike grasp and master the concepts of medication calculation.
Drug Guides NEW!
Individual drug guides and nursing considerations for the most common medications used in nursing pharmacology:
- Acetaminophen (Tylenol)
- Aspirin
- Atorvastatin (Lipitor)
- Enoxaparin (Lovenox)
- Furosemide (Lasix)
- Gabapentin
- Hydromorphone (Dilaudid)
- Lisinopril
- Metoprolol
- Morphine
Gastrointestinal System Drugs
Respiratory System Drugs
- Antihistamines
- Bronchodilators and Antiasthmatics
- Decongestants
- Expectorants and Mucolytics
- Inhaled Steroids
- Lung Surfactants
Endocrine System Drugs
- Adrenocortical Agents
- Antidiabetic Agents
- Glucose-Elevating Agents
- Hypothalamic Agents
- Insulin
- Parathyroid Agents: Bisphosphonates, Calcitonins
- Pituitary Drugs
- Sulfonylureas
- Thyroid Agents
Autonomic Nervous System Drugs
- Adrenergic Agonists (Sympathomimetics)
- Adrenergic Antagonists (Sympatholytics)
- Anticholinergics (Parasympatholytics)
- Cholinergic Agonists (Parasympathomimetics)
Immune System Drugs
Chemotherapeutic Agents
- Anthelmintics
- Anti-Infective Drugs
- Antibiotics
- Antifungals
- Antineoplastic Agents
- Antiprotozoal Drugs
- Antiviral Drugs
Reproductive System Drugs
Nervous System Drugs
- Antidepressants
- Antiparkinsonism Drugs
- Antiseizure Drugs
- Anxiolytics and Hypnotic Drugs
- General and Local Anesthetics
- Muscle Relaxants
- Narcotics, Narcotic Agonists, and Antimigraine Agents
- Neuromuscular Junction Blocking Agents
- Psychotherapeutic Drugs
Cardiovascular System Drugs
References and Sources
References and sources for this pharmacology guide for Antihypertensive Agents:
- Karch, A. M., & Karch. (2011). Focus on nursing pharmacology. Wolters Kluwer Health/Lippincott Williams & Wilkins. [Link]
- Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
- Lehne, R. A., Moore, L. A., Crosby, L. J., & Hamilton, D. B. (2004). Pharmacology for nursing care.
- Smeltzer, S. C., & Bare, B. G. (1992). Brunner & Suddarth’s textbook of medical-surgical nursing. Philadelphia: JB Lippincott. [Link]

Hello Iris, I don’t see beta-blockers listed as a anti-hypertensive here.
Please make correction above:
“Stage 2 Hypertension – systolic: less than or equal to 140 mmHg; diastolic: less than or equal to 90 mmHg”
This should be greater than or equal to for both sys and dias.
eg. “systolic: greater than or equal to 140 mmHg; diastolic: greater than or equal to 90 mmHg”
This has been corrected and updated, thanks for the heads up!