In this ultimate tutorial and nursing diagnosis list, we’ll walk you through the concepts behind writing nursing diagnosis. Learn what a nursing diagnosis is, its history and evolution, the nursing process, the different types and classifications, and how to write nursing diagnoses correctly. Included also in this guide are tips on how you can formulate better nursing diagnoses, plus guides on how you can use them in creating your nursing care plans.
Table of Contents
- What is a Nursing Diagnosis?
- Purposes of Nursing Diagnosis
- Differentiating Nursing Diagnoses, Medical Diagnoses, and Collaborative Problems
- Classification of Nursing Diagnoses (Taxonomy II)
- Nursing Process
- Types of Nursing Diagnoses
- Components of a Nursing Diagnosis
- Diagnostic Process: How to Diagnose
- How to Write a Nursing Diagnosis?
- Nursing Diagnosis for Care Plans
- Recommended Resources
- See also
- References and Sources
What is a Nursing Diagnosis?
A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability to that response, by an individual, family, group, or community. A nursing diagnosis provides the basis for selecting nursing interventions to achieve outcomes for which the nurse has accountability. Nursing diagnoses are developed based on data obtained during the nursing assessment and enable the nurse to develop the care plan.
Purposes of Nursing Diagnosis
The purpose of the nursing diagnosis is as follows:
- For nursing students, nursing diagnoses are an effective teaching tool to help sharpen their problem-solving and critical thinking skills.
- Helps identify nursing priorities and helps direct nursing interventions based on identified priorities.
- Helps the formulation of expected outcomes for quality assurance requirements of third-party payers.
- Nursing diagnoses help identify how a client or group responds to actual or potential health and life processes and knowing their available resources of strengths that can be drawn upon to prevent or resolve problems.
- Provides a common language and forms a basis for communication and understanding between nursing professionals and the healthcare team.
- Provides a basis of evaluation to determine if nursing care was beneficial to the client and cost-effective.
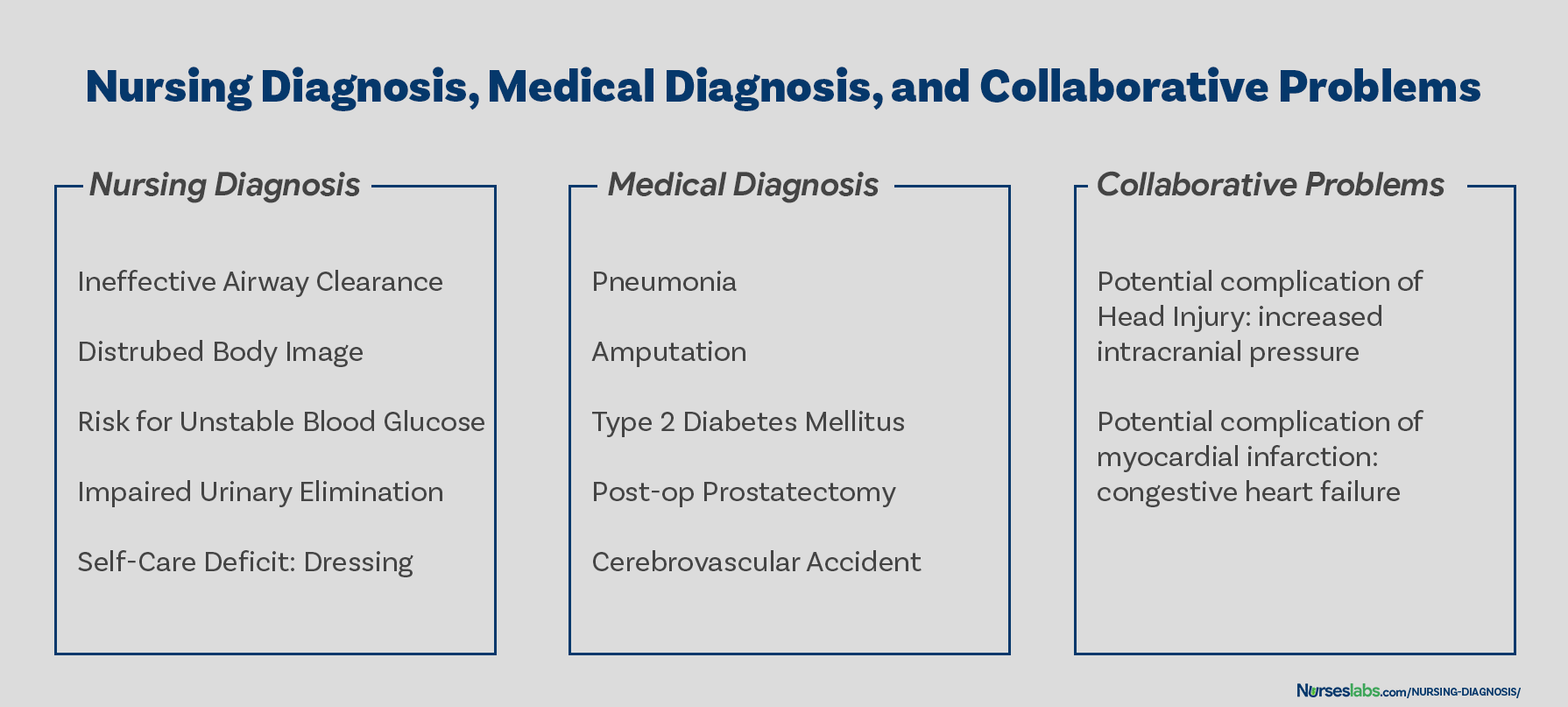
Differentiating Nursing Diagnoses, Medical Diagnoses, and Collaborative Problems
The term nursing diagnosis is associated with different concepts. It may refer to the distinct second step in the nursing process, diagnosis (“D” in “ADPIE“). Also, nursing diagnosis applies to the label when nurses assign meaning to collected data appropriately labeled a nursing diagnosis. For example, during the assessment, the nurse may recognize that the client feels anxious, fearful, and finds it difficult to sleep. Those problems are labeled with nursing diagnoses: respectively, Anxiety, Fear, and Disturbed Sleep Pattern. In this context, a nursing diagnosis is based upon the patient’s response to the medical condition. It is called a ‘nursing diagnosis’ because these are matters that hold a distinct and precise action associated with what nurses have the autonomy to take action about with a specific disease or condition. This includes anything that is a physical, mental, and spiritual type of response. Hence, a nursing diagnosis is focused on care.
On the other hand, a medical diagnosis is made by the physician or advanced health care practitioner that deals more with the disease, medical condition, or pathological state only a practitioner can treat. Moreover, through experience and know-how, the specific and precise clinical entity that might be the possible cause of the illness will then be undertaken by the doctor, therefore, providing the proper medication that would cure the illness. Examples of medical diagnoses are Diabetes Mellitus, Tuberculosis, Amputation, Hepatitis, and Chronic Kidney Disease. The medical diagnosis normally does not change. Nurses must follow the physician’s orders and carry out prescribed treatments and therapies.
Collaborative problems are potential problems that nurses manage using both independent and physician-prescribed interventions. These are problems or conditions that require both medical and nursing interventions, with the nursing aspect focused on monitoring the client’s condition and preventing the development of the potential complication.
As explained above, now it is easier to distinguish a nursing diagnosis from a medical diagnosis. Nursing diagnosis is directed towards the patient and their physiological and psychological response. On the other hand, a medical diagnosis is particular to the disease or medical condition. Its center is on the illness.
Classification of Nursing Diagnoses (Taxonomy II)
How are nursing diagnoses listed, arranged, or classified? In 2002, Taxonomy II was adopted, which was based on the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Taxonomy II has three levels: Domains (13), Classes (47), and nursing diagnoses. Nursing diagnoses are no longer grouped by Gordon’s patterns but coded according to seven axes: diagnostic concept, time, unit of care, age, health status, descriptor, and topology. In addition, diagnoses are now listed alphabetically by their concept, not by the first word.
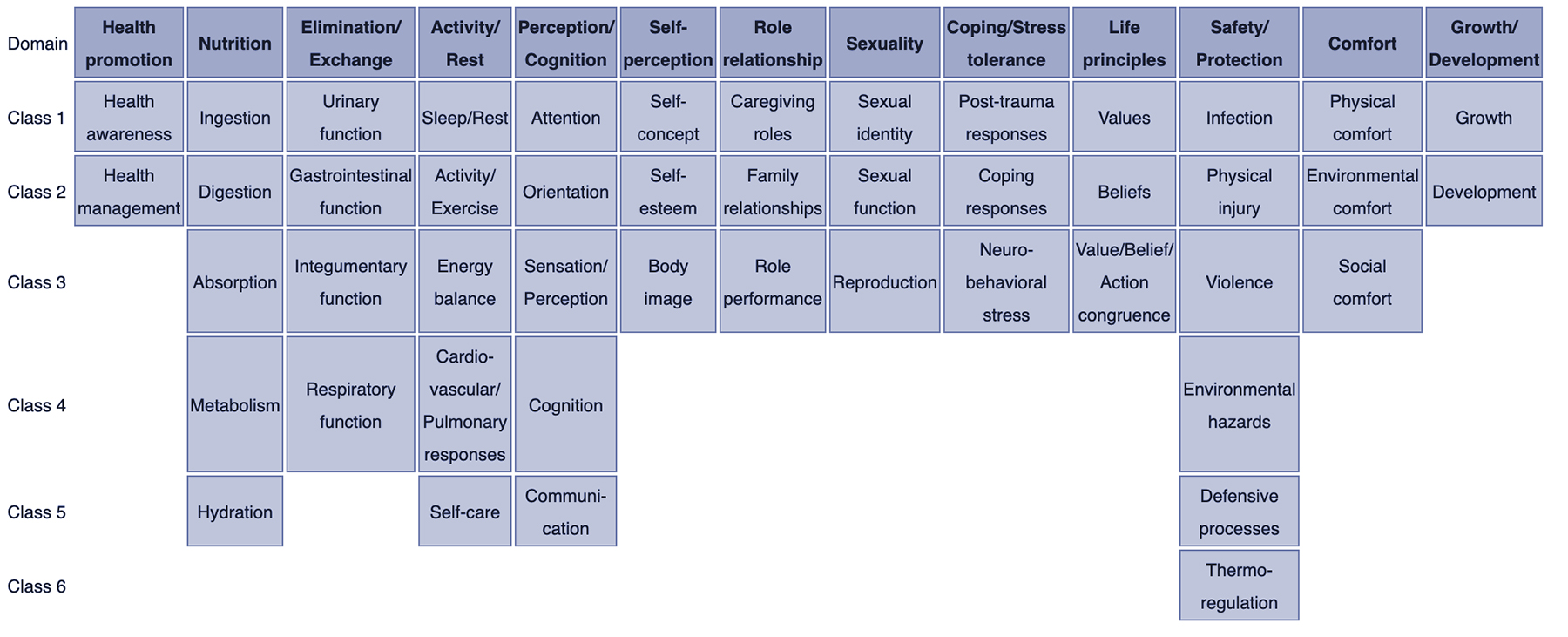
- Domain 1. Health Promotion
- Class 1. Health Awareness
- Class 2. Health Management
- Domain 2. Nutrition
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
- Domain 3. Elimination and Exchange
- Class 1. Urinary function
- Class 2. Gastrointestinal function
- Class 3. Integumentary function
- Class 4. Respiratory function
- Domain 4. Activity/Rest
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy balance
- Class 4. Cardiovascular/Pulmonary responses
- Class 5. Self-care
- Domain 5. Perception/Cognition
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
- Domain 6. Self-Perception
- Class 1. Self-concept
- Class 2. Self-esteem
- Class 3. Body image
- Domain 7. Role relationship
- Class 1. Caregiving roles
- Class 2. Family relationships
- Class 3. Role performance
- Domain 8. Sexuality
- Class 1. Sexual identity
- Class 2. Sexual function
- Class 3. Reproduction
- Domain 9. Coping/stress tolerance
- Class 1. Post-trauma responses
- Class 2. Coping responses
- Class 3. Neurobehavioral stress
- Domain 10. Life principles
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action congruence
- Domain 11. Safety/Protection
- Class 1. Infection
- Class 2. Physical injury
- Class 3. Violence
- Class 4. Environmental hazards
- Class 5. Defensive processes
- Class 6. Thermoregulation
- Domain 12. Comfort
- Class 1. Physical comfort
- Class 2. Environmental comfort
- Class 3. Social comfort
- Domain 13. Growth/Development
- Class 1. Growth
- Class 2. Development
Nursing Process
The five stages of the nursing process are assessment, diagnosing, planning, implementation, and evaluation. All steps in the nursing process require critical thinking by the nurse. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps, importance, purposes, and characteristics of the nursing process are discussed more in detail here: “The Nursing Process: A Comprehensive Guide“
Types of Nursing Diagnoses
The four types of nursing diagnosis are Actual (Problem-Focused), Risk, Health Promotion, and Syndrome. Here are the four categories of nursing diagnoses:
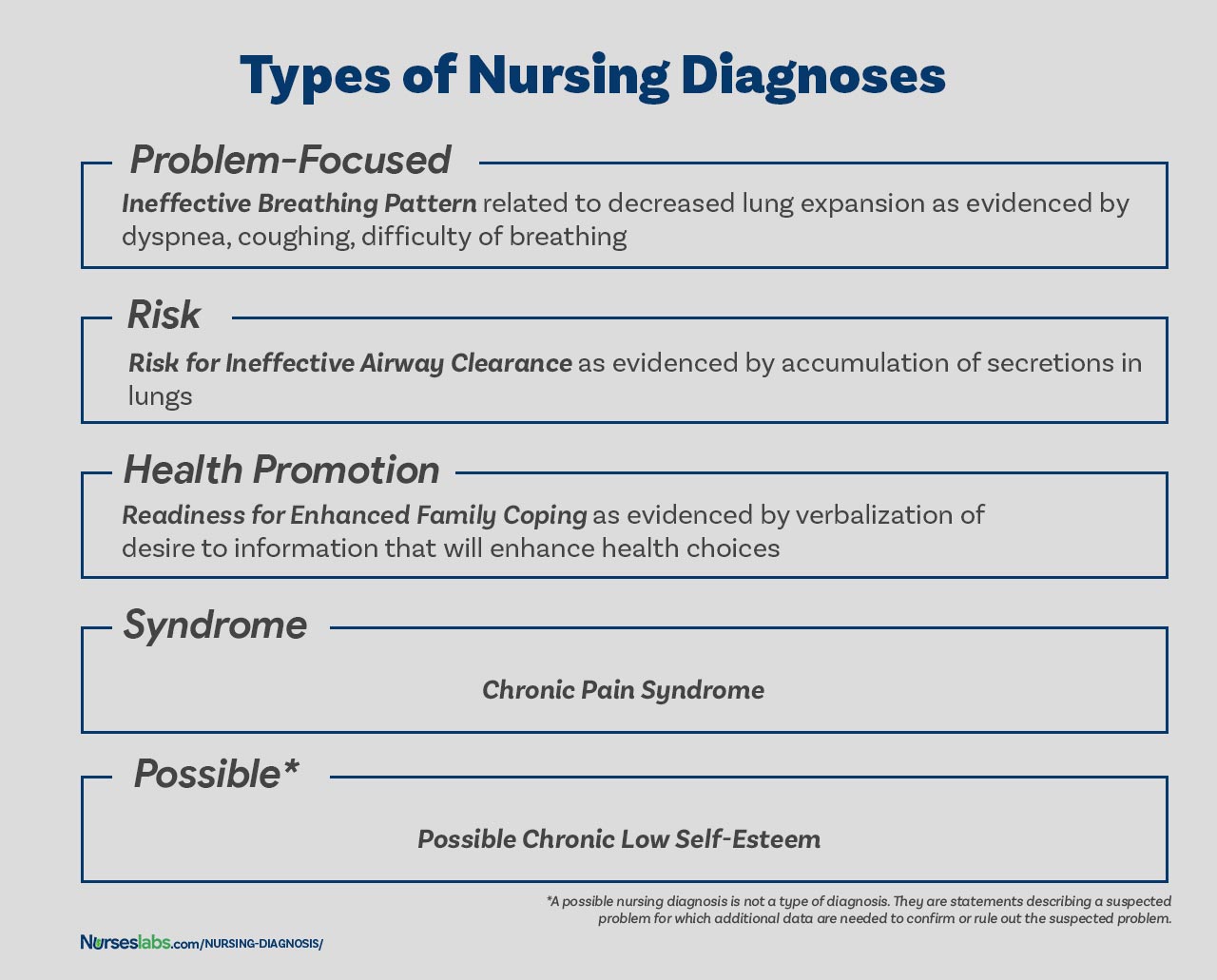
Problem-Focused Nursing Diagnosis
A problem-focused diagnosis (also known as actual diagnosis) is a client problem present at the time of the nursing assessment. These diagnoses are based on the presence of associated signs and symptoms. Actual nursing diagnosis should not be viewed as more important than risk diagnoses. There are many instances where a risk diagnosis can be the diagnosis with the highest priority for a patient.
Problem-focused nursing diagnoses have three components: (1) nursing diagnosis, (2) related factors, and (3) defining characteristics. Examples of actual nursing diagnoses are:
- Anxiety related to stress as evidenced by increased tension, apprehension, and expression of concern regarding upcoming surgery
- Acute pain related to decreased myocardial flow as evidenced by grimacing, expression of pain, guarding behavior.
Risk Nursing Diagnosis
The second type of nursing diagnosis is called risk nursing diagnosis. These are clinical judgments that a problem does not exist, but the presence of risk factors indicates that a problem is likely to develop unless nurses intervene. A risk diagnosis is based on the patient’s current health status, past health history, and other risk factors that may increase the patient’s likelihood of experiencing a health problem. These are integral part of nursing care because they help to identify potential problems early on and allows the nurse to take steps to prevent or mitigate the risk.
There are no etiological factors (related factors) for risk diagnoses. The individual (or group) is more susceptible to developing the problem than others in the same or a similar situation because of risk factors. For example, an elderly client with diabetes and vertigo who has difficulty walking refuses to ask for assistance during ambulation may be appropriately diagnosed with risk for injury or risk for falls.
Components of a risk nursing diagnosis include (1) risk diagnostic label, and (2) risk factors. Examples of risk nursing diagnosis are:
- Risk for injury
- Risk for infection
Health Promotion Diagnosis
Health promotion diagnosis (also known as wellness diagnosis) is a clinical judgment about motivation and desire to increase well-being. It is a statement that identifies the patient’s readiness for engaging in activities that promote health and well-being. For example, if a first-time mother shows interest on how to properly breastfeed her baby, a nurse make make a health promotion diagnosis of “Readiness for Enhanced Breastfeeding.” This nursing diagnosis will be then used to guide nursing interventions aimed at supporting the patient in learning about proper breastfeeding.
Additionally, health promotion diagnosis is concerned with the individual, family, or community transition from a specific level of wellness to a higher level of wellness. Components of a health promotion diagnosis generally include only the diagnostic label or a one-part statement. Examples of health promotion diagnosis:
- Readiness for enhanced health literacy
Syndrome Diagnosis
A syndrome diagnosis is a clinical judgment concerning a cluster of problem or risk nursing diagnoses that are predicted to present because of a certain situation or event. They, too, are written as a one-part statement requiring only the diagnostic label. Examples of a syndrome nursing diagnosis are:
- Chronic Pain Syndrome
Possible Nursing Diagnosis
A possible nursing diagnosis is not a type of diagnosis as are actual, risk, health promotion, and syndrome. Possible nursing diagnoses are statements describing a suspected problem for which additional data are needed to confirm or rule out the suspected problem. It provides the nurse with the ability to communicate with other nurses that a diagnosis may be present but additional data collection is indicated to rule out or confirm the diagnosis. Examples include:
- Possible chronic low self-esteem
- Possible social isolation.
Components of a Nursing Diagnosis
A nursing diagnosis has typically three components: (1) the problem and its definition, (2) the etiology, and (3) the defining characteristics or risk factors (for risk diagnosis).
Problem and Definition
The problem statement, or the diagnostic label, describes the client’s health problem or response to which nursing therapy is given concisely. A diagnostic label usually has two parts: qualifier and focus of the diagnosis. Qualifiers (also called modifiers) are words that have been added to some diagnostic labels to give additional meaning, limit, or specify the diagnostic statement. Exempted in this rule are one-word nursing diagnoses (e.g., Anxiety, Constipation, Diarrhea, Nausea, etc.) where their qualifier and focus are inherent in the one term.
| Qualifier | Focus of the Diagnosis |
|---|---|
| Deficient | Fluid volume |
| Imbalanced | Nutrition: Less Than Body Requirements |
| Impaired | Gas Exchange |
| Ineffective | Tissue Perfusion |
| Risk for | Injury |
Etiology
The etiology, or related factors, component of a nursing diagnosis label identifies one or more probable causes of the health problem, are the conditions involved in the development of the problem, gives direction to the required nursing therapy, and enables the nurse to individualize the client’s care. Nursing interventions should be aimed at etiological factors in order to remove the underlying cause of the nursing diagnosis. Etiology is linked with the problem statement with the phrase “related to” for example:
- Activity intolerance related to generalized weakness.
- Decreased cardiac output related to abnormality in blood profile
Risk Factors
Risk factors are used instead of etiological factors for risk nursing diagnosis. Risk factors are forces that put an individual (or group) at an increased vulnerability to an unhealthy condition. Risk factors are written following the phrase “as evidenced by” in the diagnostic statement.
- Risk for falls as evidenced by old age and use of walker.
- Risk for infection as evidenced by break in skin integrity.
Defining Characteristics
Defining characteristics are the clusters of signs and symptoms that indicate the presence of a particular diagnostic label. In actual nursing diagnosis, the defining characteristics are the identified signs and symptoms of the client. For risk nursing diagnosis, no signs and symptoms are present therefore the factors that cause the client to be more susceptible to the problem form the etiology of a risk nursing diagnosis. Defining characteristics are written following the phrase “as evidenced by” or “as manifested by” in the diagnostic statement.
Diagnostic Process: How to Diagnose
There are three phases during the diagnostic process: (1) data analysis, (2) identification of the client’s health problems, health risks, and strengths, and (3) formulation of diagnostic statements.
Analyzing Data
Analysis of data involves comparing patient data against standards, clustering the cues, and identifying gaps and inconsistencies.
Identifying Health Problems, Risks, and Strengths
In this decision-making step, after data analysis, the nurse and the client identify problems that support tentative actual, risk, and possible diagnoses. It involves determining whether a problem is a nursing diagnosis, medical diagnosis, or a collaborative problem. Also, at this stage, the nurse and the client identify the client’s strengths, resources, and abilities to cope.
Formulating Diagnostic Statements
Formulation of diagnostic statements is the last step of the diagnostic process wherein the nurse creates diagnostic statements. The process is detailed below.
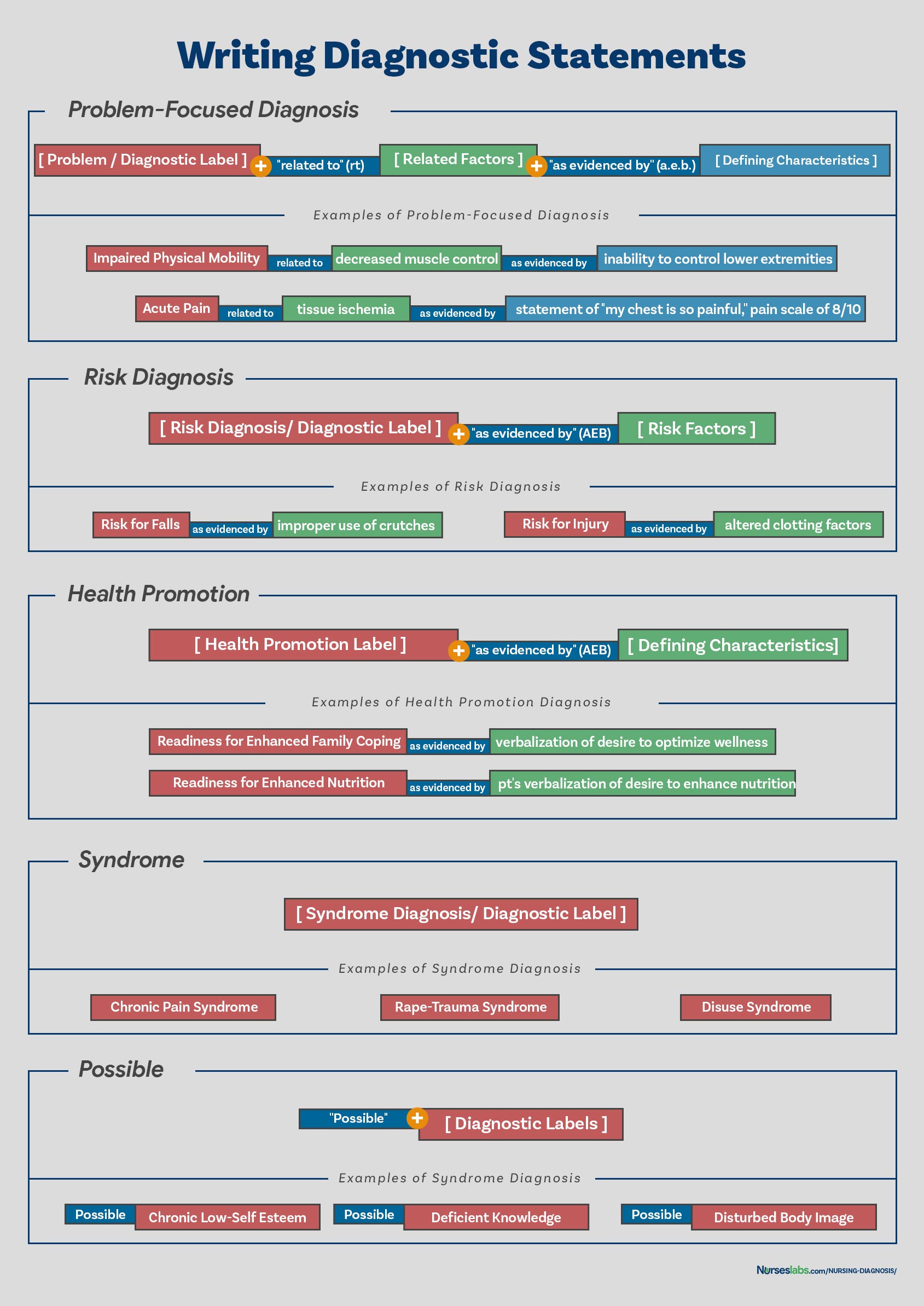
How to Write a Nursing Diagnosis?
In writing nursing diagnostic statements, describe an individual’s health status and the factors that have contributed to the status. You do not need to include all types of diagnostic indicators. Writing diagnostic statements vary per type of nursing diagnosis (see below).
PES Format
Another way of writing nursing diagnostic statements is by using the PES format, which stands for Problem (diagnostic label), Etiology (related factors), and Signs/Symptoms (defining characteristics). Diagnostic statements can be one-part, two-part, or three-part using the PES format.
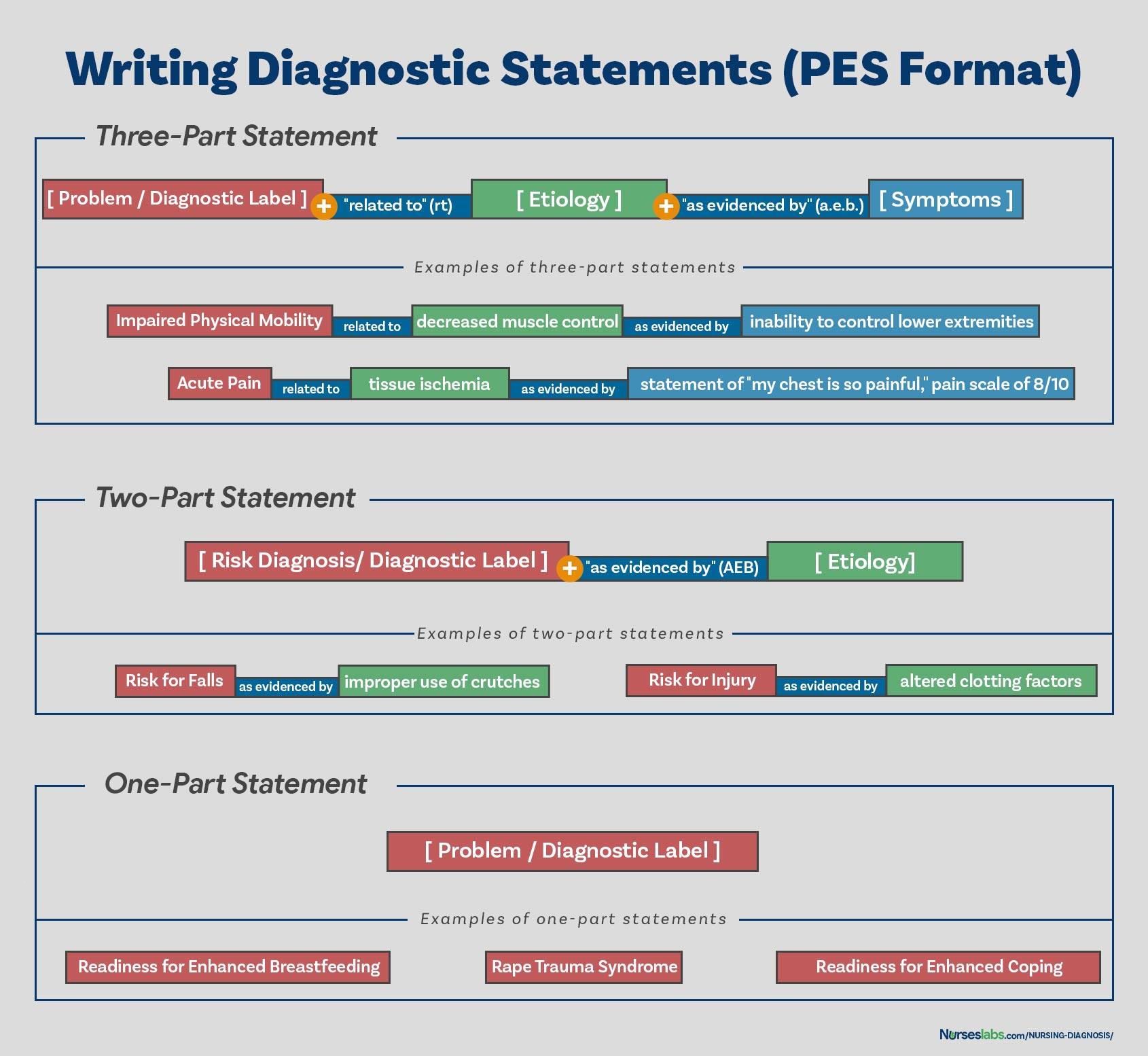
One-Part Nursing Diagnosis Statement
Health promotion nursing diagnoses are usually written as one-part statements because related factors are always the same: motivated to achieve a higher level of wellness through related factors may be used to improve the chosen diagnosis. Syndrome diagnoses also have no related factors. Examples of one-part nursing diagnosis statements include:
- Readiness for enhanced coping
- Rape Trauma Syndrome
Two-Part Nursing Diagnosis Statement
Risk and possible nursing diagnoses have two-part statements: the first part is the diagnostic label and the second is the validation for a risk nursing diagnosis or the presence of risk factors. It’s not possible to have a third part for risk or possible diagnoses because signs and symptoms do not exist. Examples of two-part nursing diagnosis statements include:
- Risk for infection as evidenced by weakened immune system response
- Risk for injury as evidenced by unstable hemodynamic profile
Three-part Nursing Diagnosis Statement
An actual or problem-focus nursing diagnosis has three-part statements: diagnostic label, contributing factor (“related to”), and signs and symptoms (“as evidenced by” or “as manifested by”). The three-part nursing diagnosis statement is also called the PES format which includes the Problem, Etiology, and Signs and Symptoms. Example of three-part nursing diagnosis statements include:
- Acute pain related to tissue ischemia as evidenced by statement of “I feel severe pain on my chest!”
Variations on Basic Statement Formats
Variations in writing nursing diagnosis statement formats include the following:
- Using “secondary to” to divide the etiology into two parts to make the diagnostic statement more descriptive and useful. Following the “secondary to” is often a pathophysiologic or disease process or a medical diagnosis. For example, Risk for Decreased Cardiac Output related to reduced preload secondary to myocardial infarction.
- Using “complex factors” when there are too many etiologic factors or when they are too complex to state in a brief phrase. For example, Chronic Low Self-Esteem related to complex factors.
- Using “unknown etiology” when the defining characteristics are present but the nurse does not know the cause or contributing factors. For example, Ineffective Coping related to unknown etiology.
- Specifying a second part of the general response or diagnostic label to make it more precise. For example, Impaired Skin Integrity (Right Anterior Chest) related to disruption of skin surface secondary to burn injury.
Nursing Diagnosis for Care Plans
This section is the list or database of the common nursing diagnosis examples that you can use to develop your nursing care plans.
See also: Nursing Care Plans (NCP): Ultimate Guide and List
- Acute Pain
- Anxiety
- Chronic Pain
- Constipation
- Decreased Cardiac Output
- Diarrhea
- Fatigue
- Fear
- Grieving
- Hopelessness
- Hyperthermia
- Hypothermia
Recommended Resources
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care
We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition)
Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales
Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care
Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health
Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

See also
Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ!
Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch. - Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing
Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
References and Sources
References for this Nursing Diagnosis guide and recommended resources to further your reading.
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.
Very useful document indeed.
Thank you Sima! Hope it helps come up with great nursing care plans!
Thank you for this resource material. This is very simple, concise and easy to understand. This would be of great help both for the students and the teacher.
Please make proper table for nursing diagnosis it’ll be easy to read and understand .
Thank youu
This is simple and easy to understand.
Happy to know! Hope you visit our guide on nursing care plans too! Thanks for dropping by Modupe!
I need a complete pdf file
Hi! If you want to save it as a PDF file, simply “Print” this page and “Save as PDF”.
So very happy to stumble upon nurseslabs. Thanks so much
Happy to have helped you. Please do check out our nursing care plans list too! Thanks for visiting, Hussaina!
I want to acknowledge the writer of Understand, Matt Vera for using the initiative in simplifying the nursing notes into simple English that we as upcoming nursing students can understand nursing notes in order to practice them in our clinical. I’ve learned so much from this website and I want to be part of the nurses website so I can gather some more informations. Get me on my email.
Thanks so much..
Thank you Lawrencia. Glad to be of help!
VERY NICE EXPLANATION .THANK YOU . DEAR MADAM /SIR PLEASE CAN YOU PROVIDE ME LIST OF NURSING DIAGNOSIS ALONG WITH REVISED ONE TILL DATE .
I am Lecturer in college of nursing ,India
Thank You
this is so educative thank you
Thank you! Glad you liked it.
really simple and effective, thank you so much.
This is great! Simple and easy to understand for the nursing students.
Comment:nice work, great nurses.
I am a nurse more than 30 yeras and try to teach my team how to used nursing process but it not success. You make me feel it simple and easy to understand . I will use your concept for my team. Thank you somuch
THANK, THANK YOU, THANK YOU FOR THE RESOURCEFUL INFORMATION.
please i want care plan on risk for unstable blood pressure
i am a nursing student
@joseph auarshie jnr, can you please send me your care plan if you made it already ? I am a nursing student too. Thank you appreciated
Thanks, I look forward to learning more from you and maybe joining you in writing once am done with school. It’s awesome.
You’re very much welcome! Please feel free to ask further questions. Thank you and goodluck!
I what to check out nursing care plan
Comment: good explanation of health issue pattern
This is great. Thanks for given your time to this. Is so educative. Up thumb
Thanks alot am so interested on this
Great Work!
THANK, THANK YOU, THANK YOU FOR THE RESOURCEFUL INFORMATION.
Thank you for the resourceful information which I was thought in school but almost forgotten until now, brain refresh, thanks
Excellent job done congratulations to all the team worker .
Each time I research about nursing diagnoses, there is something new to learn. This is a very well written piece giving great insights about nursing. More than ever, I have a better understanding of the unique body of nursing knowledge. Bravo to the Matt and entire Nurseslabs team
Thank you! Be sure to visit also our nursing care plans here.
Sorry madam the risk factors thus the potential problem has the related factors not the sign and symptom because that something has not happed yet so there is no sign and symptoms. Thank you
Excellent work and expertise team work
Usefull information
Nice work Sir/Madam thank you for giving us more hints on Nursing Diagnoses. Excellent team work.
Thank you so much for this nursing diagnosis.
Formulations of the DX has been hectic but thanks to matt vera has been of great help especally answering medsurge quizes just try to expand more on the second part (related to)of actual diagnosis
Hi Ruth,
Thank you!
Hi Mary,
Thanks you so much for your comment and endorsement. We welcome your students, thanks again!
Very useful indeed. thank you
I’m practicing nursing diagnosis by using the practice case studies my professor provided but I’m not sure if I’m doing it correctly. Here’s what I’m thinking:
Problem:Anxiety
Etiology: morning bouts of fear
Signs and symptoms: patient stated waking nervous, light headed, agitated, and having a pounding heart
Anxiety related to morning bouts of fear as evidenced by patient’s reports of waking light headed, agitated, and having a pounding heart.
In this case study we know to patient has been experiencing anxiety since childhood and was verbally abused by his father. His anxiety is causing difficulties for him to make decisions and he fears he’ll experience misfortunes whenever going to school. We also know about these bouts he has ever morning, which I thought would be a good primary diagnosis because they almost seem like a panic attack which would be extreme anxiety which is a big deal right? Am I thinking about this the right way or not and if not, what should I be concerned about as most important and how should my diagnosis be worded?
The nursing diagnostic statement you made sounds right. For the “as evidenced by” part, I would add the statement of the patient in verbatim since this is a subjective data (place it also under quotation marks) and if possible, do your own assessment and objectively obtain the data.
I would write it this way:
Anxiety related to morning bouts of fear as evidenced by increased in heart rate, apprehensiveness, and patient stating “waking lightheaded, agitated, and having a pounding heart”
well precised and nice to read.
Thanks so much for this readings, am so interested with this website I hope i could use this for my whole time
Hello Professor Matt Vera
I am Mai Ba Hai, from Hue University of Medicine and Pharmacy,faculty of nursing.I found that this content is very useful and helpful to me. I think that this content is really fit to my teaching, so I would like to ask your permission that I can translate this content into my languages (Vietnamese) to teach for my nursing students in Vietnam. I will cite you as author of this document. If you are willing to help in this point I really appreciate about it. I am looking forward to receiving your agreement. Yours sincerely.
This is so fantastic!!
Thank you for taking out time to create this wonderful piece
You guys are wonderful. Thanks so much.
Very nice and very interested More ink to your pen I pray
Very useful, thank you so much
Amazing
Thanks so much for the good job. Nurse Timothy Idachaba (RN, RNE, .MSC in view) from Nigeria
Matt Vera, BSN, R.N, First, I want to thank you for your amazing, short and precise note you provided for us.
But I think I’ve got some trouble understanding about 3 components of Nursing diagnosis.
This is because there is some variation between defining characteristics among your examples of actual and potential nursing diagnosis.
Actual nursing diagnosis
-Ineffective breathing pattern related to decreased lung expansion AS EVIDENCED BY dyspnoea, coughing, and difficulty of breathing.
Risk diagnosis
-Risk for ineffective airway clearance AS EVIDENCED BY accumulation_of_secreations_in_the_Lung.
-Risk for fall AS EVIDENCED BY Muscle_weakness
…………………………………………………….
As I know before, risk Nursing diagnosis misses Defining characteristics. because, the problem is not happened. but it is to happen.
So, when I compare defining characteristics among actual and risk diagnosis, there is disagreement.
Accumulation of secretion in the lung is aetiology for ineffective airway clearance.
But you provided it as defining characteristics.
So, please make it clear.
Well elaborated, i like using nurseslabs, i always understand easily
Educative I appreciate
Such a beautiful explanation. Thank you
Very comprehensive and understandable. A job Well done by the group
Nice piece, thanks for painstakingly organizing this concise notes, God bless you
Very educative and simple to understand. Thank you for the effort
This is very handy. Your work is appreciated
This is an excellent work . I was having lectures just now on nursing diagnosis and care plan and this note helps me a lot
Its so helpful. Thank you!
Very good content. Happy to learn the Nursing diagnosis. Thanks Nurseslabs
This is a great educative article, kind of review of the nursing diagnosis. Thanks a lot for refreshing my memory.
Sorry, it’s not.
This was so simple and very helpful
Good one
So simple, concise and very helpful.
I APPRECIATE THIS WORK, USEFUL AND EASY TO UNDERSTAND.
Beautiful. I love the nursing care plan links. it is just what I have been searching for to assist my students.
Thank you
I’ve been a nurse (currently working PRN) since 2015 and not having used nursing diagnosis in my day to day, this source was super helpful and a great refresher! Much thanks to the author!
Thanks for this it was very good and easy to comprehend
Thank you for your opinion; however, I agree with Mebratu. The description shown in your article for statement of “risk for” problem is confusing to me.
My view is as follows:
“Actual problem” has 3 parts: nursing diagnosis (client’s problem) related to etiology (pathophysiology of what is causing the problem) as evidenced by defining characteristics (signs and symptoms of the problem)
“Risk for problem” has 2 parts: nursing diagnosis (client’s potential problem) related to etiology (client condition that may cause the problem)
There is no “as evidenced by” because there IS no evidence of the problem since the problem does not yet exist.
Very nice and easy explanation, thanku
Please I need the actual manual that’s currently being used or at least a link to it -the NANDA-I document.
For the most current NANDA-I Nursing Diagnosis manual, you might want to check out the latest edition of the “Nursing Diagnosis Handbook” by NANDA International. This handbook is frequently updated with new diagnoses and guidelines.
congratulations MATT VERA, for the very nice and usefully presentation in nursing diagnosis. it has been very usefully for patient care and teaching activities.
simple and very nice understandable.
Thankyou.
Thanks a lot Matt Vera for the simplicity of the nursing diagnoses. Continue with other pieces of work
Hi Mutebe,
You’re welcome! I’m thrilled to hear you found the simplicity of the nursing diagnoses helpful. Your encouragement means a lot, and I’m definitely motivated to keep creating and simplifying more content for you and others in the nursing community.
If there are any specific topics or areas you’d like to see covered next, please let me know. Your feedback is invaluable in guiding the work I do.
Really interesting
I thank you
Very impressive step by step explanations
Its good explanation. how to download
Really helpful
Thank you
Hi Aneena, You’re welcome! I’m glad to hear you found the nursing diagnosis guide helpful. Is there a particular area or diagnosis you’d like to explore more deeply, or do you have any other questions about nursing diagnoses? Always here to help!