Another way of providing relaxation to patients is by initiating back care and giving them a massage. Learn on how you can be a pro-masseur and a nurse at the same time.
Purpose
- To stimulate the circulation and give general relief.
- To prevent bedsore
- To give comfort to the patient.
Equipment Needed
- Alcohol 25%
- Talcum powder
- Bath towel
Procedure
- Help the patient to turn on his abdomen or on his side with his back toward the nurse and his body near the edge of the bed so that he is as near the operator as possible. If the supine position is used and the patient is a woman, pillow under the abdomen removes pressure from the breasts and favor relaxation.
- Raise the gown.
- Apply to back rubbing lotion or talcum powder to reduce friction. In rubbing the back use firm long strokes and kneading motions (see below). The amount of pressure to exert depends upon the patient’s condition. Begin from neck and shoulders then proceed over the entire back.
- Massage with both hands working with a strong stroke. In upward then in downward motions. Give particular attention to pressure areas in rubbing (Alcohol 25%) to 50% is generally used for its refreshing effect, but rubbing lotion may be used.
- Powder again the area at the completion of the rubbing process which should consume from 3-5 minutes.
- Turn patient on his back and put on the gown.
- Fix and make patient comfortable.
Movements Used
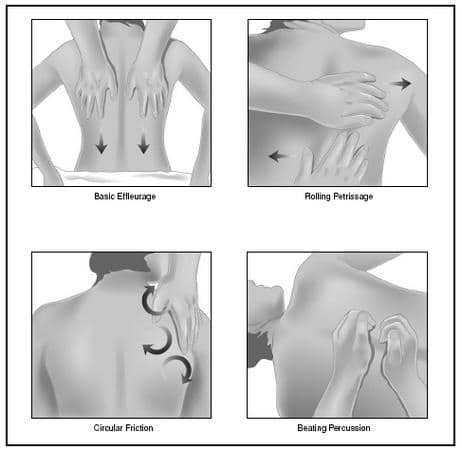
- Effleurage (stroking) —is a long sweeping movement with palm of hand conforming to the contour of the surface treated, over small surface (on the neck) the thumb and fingers are used. Strokes should be slow, rhythmical and gentle with pressure constant and in the direction of venous stream.
- Kneading—performed with the ulnar side palm resting on the surface and the fingers, and thumb grasping the skin and subcutaneous tissues which move with the hand of the operator.
- Friction—is performed with the whole palmar surface of the hand or fingers and thumbs over limited areas. This movement is a circular form of kneading with pressure against the underlying part of tissue which cannot be grasped.

Am 2 year clinical nursing student i want know more…
You work gives nursing its scientific upgrade. Most things I did as a nurse were done as per tradition not with rationale. Thank u
How frequently we should we give back care to a conscious bedridden patent?
And to a unconscious patient?
And to a patient having pressure sour?