Learn about the nursing care management of patients with cerebrovascular accident in this nursing study guide.
What is Cerebrovascular Accident?
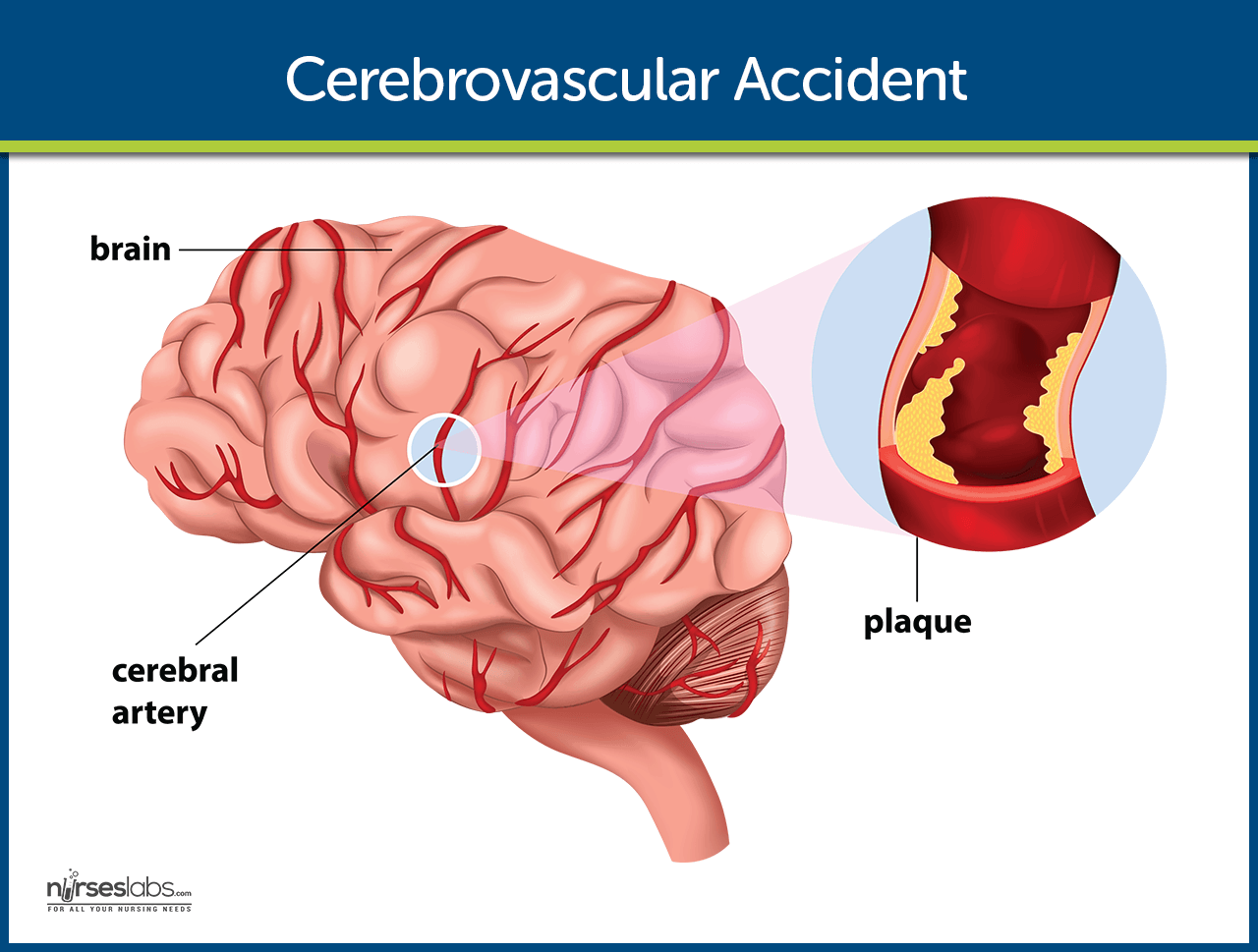
A cerebrovascular accident (CVA), an ischemic stroke or “brain attack,” is a sudden loss of brain function resulting from a disruption of the blood supply to a part of the brain.
- Cerebrovascular accident or stroke is the primary cerebrovascular disorder in the United States.
- A cerebrovascular accident is a sudden loss of brain functioning resulting from a disruption of the blood supply to a part of the brain.
- It is a functional abnormality of the central nervous system.
- Cryptogenic strokes have no known cause, and other strokes result from causes such as illicit drug use, coagulopathies, migraine, and spontaneous dissection of the carotid or vertebral arteries.
- The result is an interruption in the blood supply to the brain, causing temporary or permanent loss of movement, thought, memory, speech, or sensation.
Classification
Strokes can be divided into two classifications.
- Ischemic stroke. This is the loss of function in the brain as a result of a disrupted blood supply.
- Hemorrhagic stroke. Hemorrhagic strokes are caused by bleeding into the brain tissue, the ventricles, or the subarachnoid space.
Risk Factors
The following are the nonmodifiable and modifiable risk factors of Cerebrovascular accident:
Nonmodifiable
- Advanced age (older than 55 years)
- Gender (Male)
- Race (African American)
Modifiable
- Hypertension
- Atrial fibrillation
- Hyperlipidemia
- Obesity
- Smoking
- Diabetes
- Asymptomatic carotid stenosis and valvular heart disease (eg, endocarditis, prosthetic heart valves)
- Periodontal disease
Pathophysiology
The disruption in the blood flow initiates a complex series of cellular metabolic events.
- Decreased cerebral blood flow. The ischemic cascade begins when cerebral blood flow decreases to less than 25 mL per 100g of blood per minute.
- Aerobic respiration. At this point, neurons are unable to maintain aerobic respiration.
- Anaerobic respiration. The mitochondria would need to switch to anaerobic respiration, which generates large amounts of lactic acid, causing a change in pH and rendering the neurons incapable of producing sufficient quantities of ATP.
- Loss of function. The membrane pumps that maintain electrolyte balances fail and the cells cease to function.
Statistics and Epidemiology
Stroke is a worldwide phenomenon suffered through all walks of life.
- Morbidity: In 2005, prevalence of stroke was estimated at 2.3 million males and 3.4 million females; many of the approximately 5.7 million U.S. stroke survivors have permanent stroke-related disabilities.
- Mortality: In 2004, stroke ranked fifth as the cause of death for those aged 45 to 64 years and third for those aged 65 years or older (National Heart, Lung and Blood Institute [NHLBI], 2007), with 150,000 deaths (American Heart Association and American Stroke Association, 2008); hemorrhagic strokes are more severe, and mortality rates are higher than ischemic strokes, with a 30-day mortality rate of 40% to 80%.
- Cost: Estimated direct and indirect cost for 2008 was $65.5 billion (American Heart Association and American Stroke Association, 2008).
- Stroke is the third leading cause of death after heart disease and cancer.
- Approximately 780, 000 people experience a stroke each year in the United States.
- Approximately 600, 000 of these are new strokes, and 180, 000 are recurrent strokes.
- About 5.6 million noninstitutionalized stroke survivors are alive today.
- Stroke is the leading cause of serious, long-term disability in the United States.
- Direct and indirect costs for stroke cost $65.5 billion in 2008.
- Strokes are usually hemorrhagic (15%) or ischemic/nonhemorrhagic (85%).
- Ischemic strokes are categorized according to their cause: large artery thrombotic strokes (20%), small penetrating artery thrombotic strokes (25%), cardiogenic embolic strokes (20%), cryptogenic strokes (30%), and other (5%).
Causes
Strokes are caused by the following:
- Large artery thrombosis. Large artery thromboses are caused by atherosclerotic plaques in the large blood vessels of the brain.
- Small penetrating artery thrombosis. Small penetrating artery thrombosis affects one or more vessels and is the most common type of ischemic stroke.
- Cardiogenic emboli. Cardiogenic emboli are associated with cardiac dysrhythmias, usually atrial fibrillation.
Clinical Manifestations
Stroke can cause a wide variety of neurologic deficits, depending on the location of the lesion, the size of the area of inadequate perfusion, and the amount of the collateral blood flow. General signs and symptoms include numbness or weakness of face, arm, or leg (especially on one side of the body); confusion or change in mental status; trouble speaking or understanding speech; visual disturbances; loss of balance, dizziness, difficulty walking; or sudden severe headache.
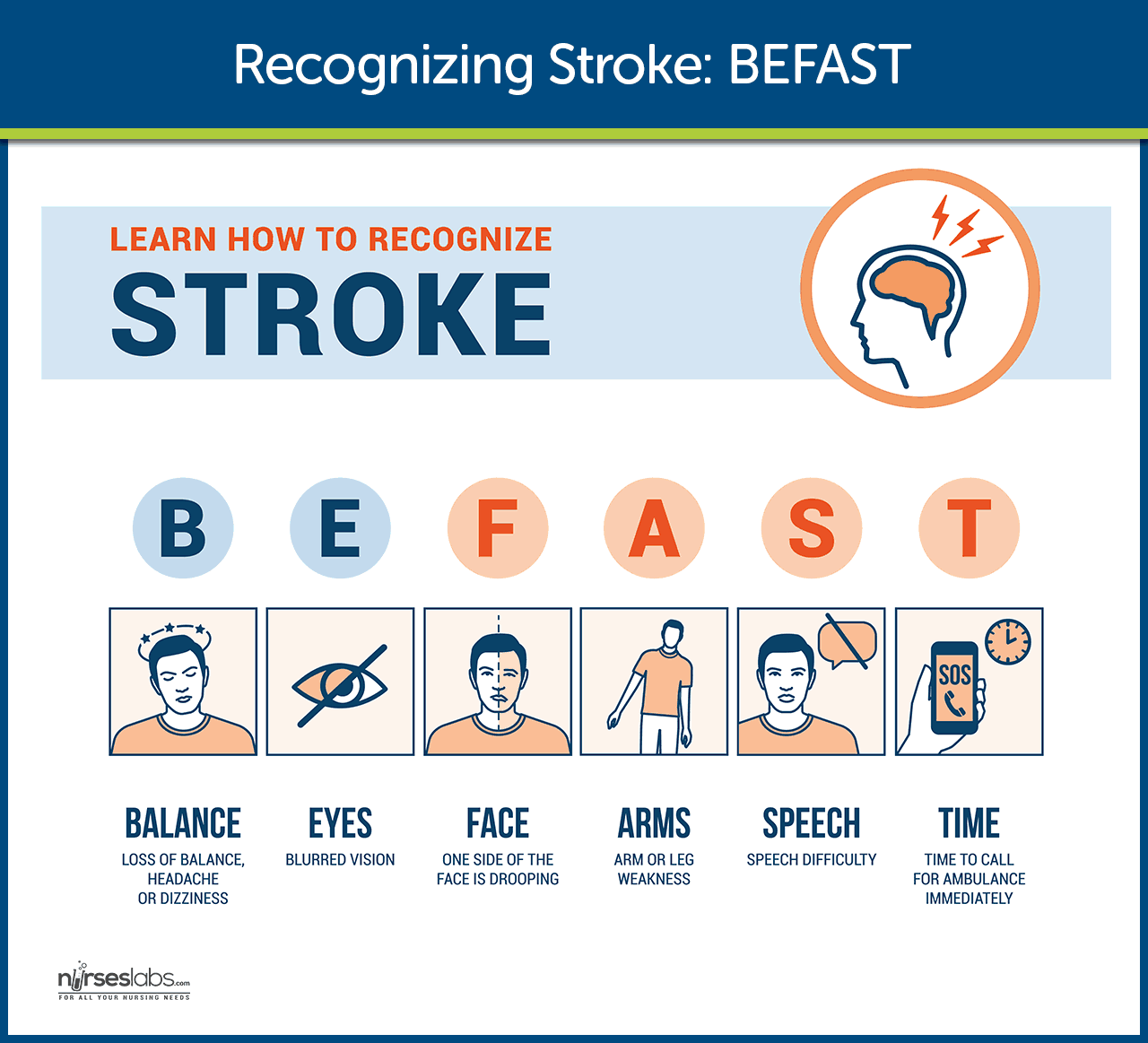
General signs and symptoms include numbness or weakness of face, arm, or leg (especially on one side of the body); confusion or change in mental status; trouble speaking or understanding speech; visual disturbances; loss of balance, dizziness, difficulty walking; or sudden severe headache.
- Numbness or weakness of the face. Without adequate perfusion, oxygen is also low, and facial tissues could not function properly without them.
- Change in mental status. Due to decreased oxygen, the patient experiences confusion.
- Trouble speaking or understanding speech. Cells cease to function as a result of inadequate perfusion.
- Visual disturbances. The eyes also need enough oxygen for optimal functioning.
- Homonymous hemianopsia. There is loss of half of the visual field.
- Loss of peripheral vision. The patient experiences difficulty seeing at night and is unaware of objects or the borders of objects.
- Hemiparesis. There is a weakness of the face, arm, and leg on the same side due to a lesion in the opposite hemisphere.
- Hemiplegia. Paralysis of the face, arm, and leg on the same side due to a lesion in the opposite hemisphere.
- Ataxia. Staggering, unsteady gait and inability to keep feet together.
- Dysarthria. This is the difficulty in forming words.
- Dysphagia. There is difficulty in swallowing.
- Paresthesia. There is numbness and tingling of extremities and difficulty with proprioception.
- Expressive aphasia. The patient is unable to form words that is understandable yet can speak in single-word responses.
- Receptive aphasia. The patient is unable to comprehend the spoken word and can speak but may not make any sense.
- Global aphasia. This is a combination of both expressive and receptive aphasia.
Motor Loss
- Hemiplegia, hemiparesis
- Flaccid paralysis and loss of or decrease in the deep tendon reflexes (initial clinical feature) followed by (after 48 hours) reappearance of deep reflexes and abnormally increased muscle tone (spasticity)
Communication Loss
- Dysarthria (difficulty speaking)
- Dysphasia (impaired speech) or aphasia (loss of speech)
- Apraxia (inability to perform a previously learned action)
Perceptual Disturbances and Sensory Loss
- Visual-perceptual dysfunctions (homonymous hemianopia [loss of half of the visual field])
- Disturbances in visual-spatial relations (perceiving the relation of two or more objects in spatial areas), frequently seen in patients with right hemispheric damage
- Sensory losses: slight impairment of touch or more severe with loss of proprioception; difficulty in interrupting visual, tactile, and auditory stimuli
Impaired Cognitive and Psychological Effects
- Frontal lobe damage: Learning capacity, memory, or other higher cortical intellectual functions may be impaired. Such dysfunction may be reflected in a limited attention span, difficulties in comprehension, forgetfulness, and lack of motivation.
- Depression, other psychological problems: emotional lability, hostility, frustration, resentment, and lack of cooperation.
Prevention
Primary prevention of stroke remains the best approach.
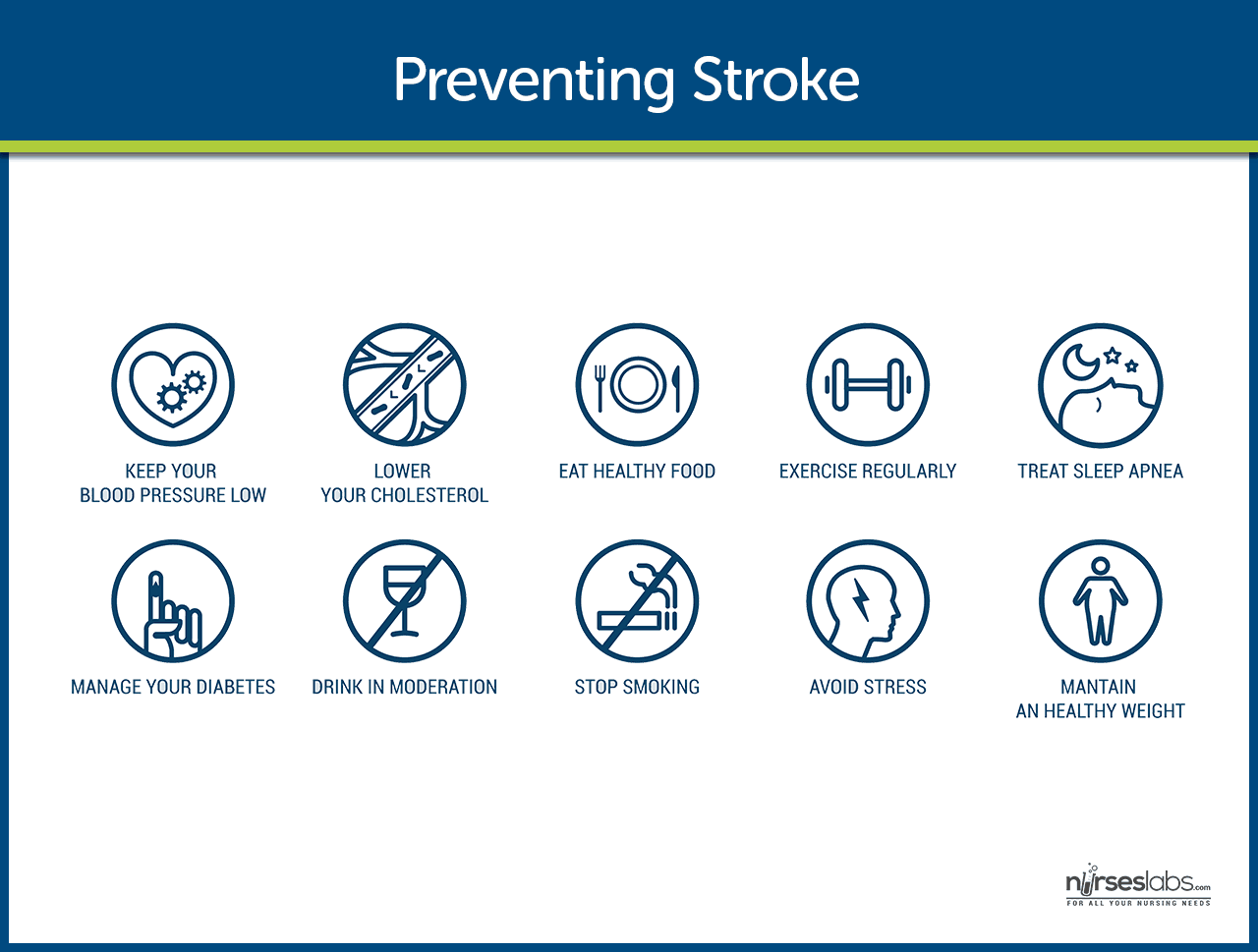
- Healthy lifestyle. Leading a healthy lifestyle which includes not smoking, maintaining a healthy weight, following a healthy diet, and daily exercise can reduce the risk of having a stroke by about one half.
- DASH diet. The DASH (Dietary Approaches to Stop Hypertension) diet is high in fruits and vegetables, moderate in low-fat dairy products, and low in animal protein and can lower the risk of stroke.
- Stroke risk screenings. Stroke risk screenings are an ideal opportunity to lower stroke risk by identifying people or groups of people who are at high risk for stroke.
- Education. Patients and the community must be educated about recognition and prevention of stroke.
- Low-dose aspirin. Research findings suggest that low-dose aspirin may lower the risk of stroke in women who are at risk.
Complications
If cerebral oxygenation is still inadequate; complications may occur.
- Tissue ischemia. If cerebral blood flow is inadequate, the amount of oxygen supplied to the brain is decreased, and tissue ischemia will result.
- Cardiac dysrhythmias. The heart compensates for the decreased cerebral blood flow, and with too much pumping, dysrhythmias may occur.
Assessment and Diagnostic Findings
Any patient with neurologic deficits needs a careful history and complete physical and neurologic examination.
- CT scan. Demonstrates structural abnormalities, edema, hematomas, ischemia, and infarctions. Demonstrates structural abnormalities, edema, hematomas, ischemia, and infarctions. Note: May not immediately reveal all changes, e.g., ischemic infarcts are not evident on CT for 8–12 hr; however, intracerebral hemorrhage is immediately apparent; therefore, emergency CT is always done before administering tissue plasminogen activator (t-PA). In addition, patients with TIA commonly have a normal CT scan
- PET scan. Provides data on cerebral metabolism and blood flow changes.
- MRI. Shows areas of infarction, hemorrhage, AV malformations, and areas of ischemia.
- Cerebral angiography. Helps determine specific cause of stroke, e.g., hemorrhage or obstructed artery, pinpoints site of occlusion or rupture. Digital subtraction angiography evaluates patency of cerebral vessels, identifies their position in head and neck, and detects/evaluates lesions and vascular abnormalities.
- Lumbar puncture. Pressure is usually normal and CSF is clear in cerebral thrombosis, embolism, and TIA. Pressure elevation and grossly bloody fluid suggest subarachnoid and intracerebral hemorrhage. CSF total protein level may be elevated in cases of thrombosis because of inflammatory process. LP should be performed if septic embolism from bacterial endocarditis is suspected.
- Transcranial Doppler ultrasonography. Evaluates the velocity of blood flow through major intracranial vessels; identifies AV disease, e.g., problems with carotid system (blood flow/presence of atherosclerotic plaques).
- EEG. Identifies problems based on reduced electrical activity in specific areas of infarction; and can differentiate seizure activity from CVA damage.
- Skull x-ray. May show a shift of pineal gland to the opposite side from an expanding mass; calcifications of the internal carotid may be visible in cerebral thrombosis; partial calcification of walls of an aneurysm may be noted in subarachnoid hemorrhage.
- ECG and echocardiography. To rule out cardiac origin as source of embolus (20% of strokes are the result of blood or vegetative emboli associated with valvular disease, dysrhythmias, or endocarditis).
- Laboratory studies to rule out systemic causes: CBC, platelet and clotting studies, VDRL/RPR, erythrocyte sedimentation rate (ESR), chemistries (glucose, sodium).
Medical Management
Patients who have experienced TIA or stroke should have medical management for secondary prevention.
- Recombinant tissue plasminogen activator would be prescribed unless contraindicated, and there should be monitoring for bleeding.
- Increased ICP. Management of increased ICP includes osmotic diuretics, maintenance of PaCO2 at 30-35 mmHg, and positioning to avoid hypoxia through elevation of the head of the bed.
- Endotracheal Tube. There is a possibility of intubation to establish patent airway if necessary.
- Hemodynamic monitoring. Continuous hemodynamic monitoring should be implemented to avoid an increase in blood pressure.
- Neurologic assessment to determine if the stroke is evolving and if other acute complications are developing
Surgical Management
Surgical management may include prevention and relief from increased ICP.
- Carotid endarterectomy. This is the removal of atherosclerotic plaque or thrombus from the carotid artery to prevent stroke in patients with occlusive disease of the extracranial cerebral arteries.
- Hemicraniectomy. Hemicraniectomy may be performed for increased ICP from brain edema in severe cases of stroke.
Nursing Management
After the stroke is complete, management focuses on the prompt initiation of rehabilitation for any deficits.
Nursing Assessment
During the acute phase, a neurologic flow sheet is maintained to provide data about the following important measures of the patient’s clinical status:
- Change in level of consciousness or responsiveness.
- Presence or absence of voluntary or involuntary movements of extremities.
- Stiffness or flaccidity of the neck.
- Eye opening, comparative size of pupils, and pupillary reaction to light.
- Color of the face and extremities; temperature and moisture of the skin.
- Ability to speak.
- Presence of bleeding.
- Maintenance of blood pressure.
During the postacute phase, assess the following functions:
- Mental status (memory, attention span, perception, orientation, affect, speech/language).
- Sensation and perception (usually the patient has decreased awareness of pain and temperature).
- Motor control (upper and lower extremity movement); swallowing ability, nutritional and hydration status, skin integrity, activity tolerance, and bowel and bladder function.
- Continue focusing nursing assessment on impairment of function in patient’s daily activities.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses for a patient with stroke may include the following:
- Impaired physical mobility related to hemiparesis, loss of balance and coordination, spasticity, and brain injury.
- Acute pain related to hemiplegia and disuse.
- Deficient self-care related to stroke sequelae.
- Disturbed sensory perception related to altered sensory reception, transmission, and/or integration.
- Impaired urinary elimination related to flaccid bladder, detrusor instability, confusion, or difficulty in communicating.
- Disturbed thought processes related to brain damage.
- Impaired verbal communication related to brain damage.
- Risk for impaired skin integrity related to hemiparesis or hemiplegia and decreased mobility.
- Interrupted family processes related to catastrophic illness and caregiving burdens.
- Sexual dysfunction related to neurologic deficits or fear of failure.
Nursing Care Planning & Goals
Main article: Cerebrovascular Accident (Stroke) Nursing Care Plans
The major nursing care planning goals for the patient and family may include:
- Improve mobility.
- Avoidance of shoulder pain.
- Achievement of self-care.
- Relief of sensory and perceptual deprivation.
- Prevention of aspiration.
- Continence of bowel and bladder.
- Improved thought processes.
- Achieving a form of communication.
- Maintaining skin integrity.
- Restore family functioning.
- Improve sexual function.
- Absence of complications.
Nursing Interventions
Nursing care has a significant impact on the patient’s recovery. In summary, here are some nursing interventions for patients with stroke:
- Positioning. Position to prevent contractures, relieve pressure, attain good body alignment, and prevent compressive neuropathies.
- Prevent flexion. Apply splint at night to prevent flexion of the affected extremity.
- Prevent adduction. Prevent adduction of the affected shoulder with a pillow placed in the axilla.
- Prevent edema. Elevate affected arm to prevent edema and fibrosis.
- Full range of motion. Provide full range of motion four or five times a day to maintain joint mobility.
- Prevent venous stasis. Exercise is helpful in preventing venous stasis, which may predispose the patient to thrombosis and pulmonary embolus.
- Regain balance. Teach patient to maintain balance in a sitting position, then to balance while standing and begin walking as soon as standing balance is achieved.
- Personal hygiene. Encourage personal hygiene activities as soon as the patient can sit up.
- Manage sensory difficulties. Approach patient with a decreased field of vision on the side where visual perception is intact.
- Visit a speech therapist. Consult with a speech therapist to evaluate gag reflexes and assist in teaching alternate swallowing techniques.
- Voiding pattern. Analyze voiding pattern and offer urinal or bedpan on patient’s voiding schedule.
- Be consistent in patient’s activities. Be consistent in the schedule, routines, and repetitions; a written schedule, checklists, and audiotapes may help with memory and concentration, and a communication board may be used.
- Assess skin. Frequently assess skin for signs of breakdown, with emphasis on bony areas and dependent body parts.
Improving Mobility and Preventing Deformities
- Position to prevent contractures; use measures to relieve pressure, assist in maintaining good body alignment, and prevent compressive neuropathies.
- Apply a splint at night to prevent flexion of affected extremity.
- Prevent adduction of the affected shoulder with a pillow placed in the axilla.
- Elevate affected arm to prevent edema and fibrosis.
- Position fingers so that they are barely flexed; place hand in slight supination. If upper extremity spasticity is noted, do not use a hand roll; dorsal wrist splint may be used.
- Change position every 2 hours; place patient in a prone position for 15 to 30 minutes several times a day.
Establishing an Exercise Program
- Provide full range of motion four or five times a day to maintain joint mobility, regain motor control, prevent contractures in the paralyzed extremity, prevent further deterioration of the neuromuscular system, and enhance circulation. If tightness occurs in any area, perform a range of motion exercises more frequently.
- Exercise is helpful in preventing venous stasis, which may predispose the patient to thrombosis and pulmonary embolus.
- Observe for signs of pulmonary embolus or excessive cardiac workload during exercise period (e.g., shortness of breath, chest pain, cyanosis, and increasing pulse rate).
- Supervise and support the patient during exercises; plan frequent short periods of exercise, not longer periods; encourage the patient to exercise unaffected side at intervals throughout the day.
Preparing for Ambulation
- Start an active rehabilitation program when consciousness returns (and all evidence of bleeding is gone, when indicated).
- Teach patient to maintain balance in a sitting position, then to balance while standing (use a tilt table if needed).
- Begin walking as soon as standing balance is achieved (use parallel bars and have a wheelchair available in anticipation of possible dizziness).
- Keep training periods for ambulation short and frequent.
Preventing Shoulder Pain
- Never lift patient by the flaccid shoulder or pull on the affected arm or shoulder.
- Use proper patient movement and positioning (e.g., flaccid arm on a table or pillows when patient is seated, use of sling when ambulating).
- Range of motion exercises are beneficial, but avoid over strenuous arm movements.
- Elevate arm and hand to prevent dependent edema of the hand; administer analgesic agents as indicated.
Enhancing Self Care
- Encourage personal hygiene activities as soon as the patient can sit up; select suitable self-care activities that can be carried out with one hand.
- Help patient to set realistic goals; add a new task daily.
- As a first step, encourage patient to carry out all self-care activities on the unaffected side.
- Make sure patient does not neglect affected side; provide assistive devices as indicated.
- Improve morale by making sure patient is fully dressed during ambulatory activities.
- Assist with dressing activities (e.g., clothing with Velcro closures; put garment on the affected side first); keep environment uncluttered and organized.
- Provide emotional support and encouragement to prevent fatigue and discouragement.
Managing Sensory-Perceptual Difficulties
- Approach patient with a decreased field of vision on the side where visual perception is intact; place all visual stimuli on this side.
- Teach patient to turn and look in the direction of the defective visual field to compensate for the loss; make eye contact with patient, and draw attention to affected side.
- Increase natural or artificial lighting in the room; provide eyeglasses to improve vision.
- Remind patient with hemianopsia of the other side of the body; place extremities so that patient can see them.
Assisting with Nutrition
- Observe patient for paroxysms of coughing, food dribbling out or pooling in one side of the mouth, food retained for long periods in the mouth, or nasal regurgitation when swallowing liquids.
- Consult with speech therapist to evaluate gag reflexes; assist in teaching alternate swallowing techniques, advise patient to take smaller boluses of food, and inform patient of foods that are easier to swallow; provide thicker liquids or pureed diet as indicated.
- Have patient sit upright, preferably on chair, when eating and drinking; advance diet as tolerated.
- Prepare for GI feedings through a tube if indicated; elevate the head of bed during feedings, check tube position before feeding, administer feeding slowly, and ensure that cuff of tracheostomy tube is inflated (if applicable); monitor and report excessive retained or residual feeding.
Attaining Bowel and Bladder Control
- Perform intermittent sterile catheterization during the period of loss of sphincter control.
- Analyze voiding pattern and offer urinal or bedpan on patient’s voiding schedule.
- Assist the male patient to an upright posture for voiding.
- Provide highfiber diet and adequate fluid intake (2 to 3 L/day), unless contraindicated.
- Establish a regular time (after breakfast) for toileting.
Improving Thought Processes
- Reinforce structured training program using cognitive, perceptual retraining, visual imagery, reality orientation, and cueing procedures to compensate for losses.
- Support patient: Observe performance and progress, give positive feedback, convey an attitude of confidence and hopefulness; provide other interventions as used for improving cognitive function after a head injury.
Improving Communication
- Reinforce the individually tailored program.
- Jointly establish goals, with the patient taking an active part.
- Make the atmosphere conducive to communication, remaining sensitive to patient’s reactions and needs and responding to them in an appropriate manner; treat the patient as an adult.
- Provide strong emotional support and understanding to allay anxiety; avoid completing patient’s sentences.
- Be consistent in schedule, routines, and repetitions. A written schedule, checklists, and audiotapes may help with memory and concentration; a communication board may be used.
- Maintain patient’s attention when talking with the patient, speak slowly, and give one instruction at a time; allow the patient time to process.
- Talk to aphasic patients when providing care activities to provide social contact.
Maintaining Skin Integrity
- Frequently assess skin for signs of breakdown, with emphasis on bony areas and dependent body parts.
- Employ pressure relieving devices; continue regular turning and positioning (every 2 hours minimally); minimize shear and friction when positioning.
- Keep skin clean and dry, gently massage the healthy dry skin and maintain adequate nutrition.
Improving Family Coping
- Provide counseling and support to the family.
- Involve others in patient’s care; teach stress management techniques and maintenance of personal health for family coping.
- Give family information about the expected outcome of the stroke, and counsel them to avoid doing things for the patient that he or she can do.
- Develop attainable goals for the patient at home by involving the total health care team, patient, and family.
- Encourage everyone to approach the patient with a supportive and optimistic attitude, focusing on abilities that remain; explain to the family that emotional lability usually improves with time.
Helping the Patient Cope with Sexual Dysfunction
- Perform indepth assessment to determine sexual history before and after the stroke.
- Interventions for patient and partner focus on providing relevant information, education, reassurance, adjustment
- of medications, counseling regarding coping skills, suggestions for alternative sexual positions, and a means of sexual expression and satisfaction.
Teaching points
- Teach patient to resume as much self care as possible; provide assistive devices as indicated.
- Have occupational therapist make a home assessment and recommendations to help the patient become more independent.
- Coordinate care provided by numerous health care professionals; help family plan aspects of care.
- Advise family that patient may tire easily, become irritable and upset by small events, and show less interest in daily events.
- Make a referral for home speech therapy. Encourage family involvement. Provide family with practical instructions to help patient between speech therapy sessions.
- Discuss patient’s depression with the physician for possible antidepressant therapy.
- Encourage patient to attend community-based stroke clubs to give a feeling of belonging and fellowship to others.
- Encourage patient to continue with hobbies, recreational and leisure interests, and contact with friends to prevent social isolation.
- Encourage family to support patient and give positive reinforcement.
- Remind spouse and family to attend to personal health and wellbeing.
Evaluation
Expected patient outcomes may include the following:
- Improved mobility.
- Absence of shoulder pain.
- Self-care achieved.
- Relief of sensory and perceptual deprivation.
- Prevention of aspiration.
- Continence of bowel and bladder.
- Improved thought processes.
- Achieved a form of communication.
- Maintained skin integrity.
- Restored family functioning.
- Improved sexual function.
- Absence of complications.
Discharge and Home Care Guidelines
Patient and family education is a fundamental component of rehabilitation.
- Consult an occupational therapist. An occupational therapist may be helpful in assessing the home environment and recommending modifications to help the patient become more independent.
- Physical therapy. A program of physical therapy may be beneficial, whether it takes place in the home or in an outpatient program.
- Antidepressant therapy. Depression is a common and serious problem in the patient who has had a stroke.
- Support groups. Community-based stroke support groups may allow the patient and the family to learn from others with similar problems and to share their experiences.
- Assess caregivers. Nurses should assess caregivers for signs of depression, as depression is also common among caregivers of stroke survivors.
Documentation Guidelines
The focus of documentation should involve:
- Individual findings including level of function and ability to participate in specific or desired activities.
- Needed resources and adaptive devices.
- Results of laboratory tests, diagnostic studies, and mental status or cognitive evaluation.
- SO/family support and participation.
- Plan of care and those involved in planning.
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcomes.
- Modifications to plan of care.
See Also
Posts related to Cerebrovascular Accident (Stroke):








Leave a Comment