Holter monitoring (Ambulatory electrocardiography, ambulatory monitoring, event recorder, Holter electrocardiography) is a noninvasive procedure that continuously records the heart’s activity as the patient does his normal routine, usually for 24 to 72 hours.
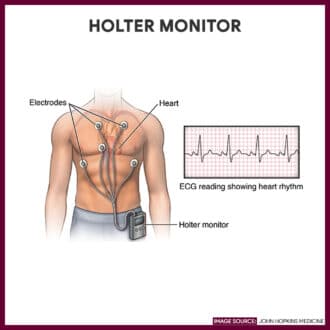
Holter monitoring involves the use of a portable external monitor worn by means of a strap around the waist or over the shoulder that measures and records the heart electrical impulses on a tape. The monitor is equipped with a clock that permits accurate time monitoring. The patient is asked to carry a diary and record daily activities, as well as any cardiac symptoms that may experience during the testing. As the patient pushes a button signifying that symptoms have occurred, an event marker is placed on the tape for later correlation with the cardiac activity recordings and the daily event diary. The tape is then interpreted by a computer to detect any significant abnormal waveform patterns.
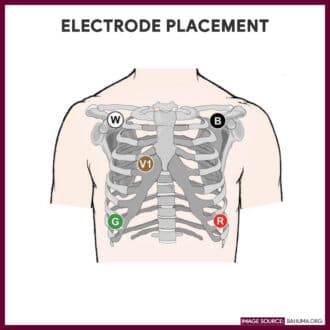
A critical duty of the nurse during this procedure is to make sure the electrodes are placed correctly. This will ensure the avoidance of having inaccurate results. This study guide can help nurses understand their tasks and responsibilities when handling a patient with a Holter monitor.
Table of Contents
- Indications of Holter Monitoring
- Interfering Factors
- Holter Monitoring Procedure
- Nursing Responsibilities of Holter Monitoring
- Normal Results
- Abnormal Results
- Gallery
- References
Indications of Holter Monitoring
Holter monitoring is indicated for the following reasons:
- Detect cardiac dysrhythmias that occur during normal activities and correlate them with symptoms experienced by the patient
- Detect sporadic arrhythmias missed by an exercise or resting ECG
- Evaluate chest pain, palpitations, dizziness, and syncope
- Evaluate activity intolerance associated with an imbalance of oxygen supply and demand
- Monitor the effectiveness of antiarrhythmic drug therapy or a pacemaker
- Monitor for ischemia and dysrhythmias following myocardial infarction or heart surgery before changing rehabilitation and other therapeutic regimens
Interfering Factors
These are factors or conditions that may alter the outcome or results of Holter monitoring: Improper placement of the electrodes or movement of the electrodes
- Failure of the patient to keep an accurate diary of symptoms or to push button to produce a mark on the strip when experiencing symptoms
Holter Monitoring Procedure
The following steps will explain how Holter monitoring is done:
- Prepare the skin
The area where the electrode patches are placed are cleaned with alcohol; Excess hair may be shaved or clipped from the site if appropriate. - Attach the electrodes.
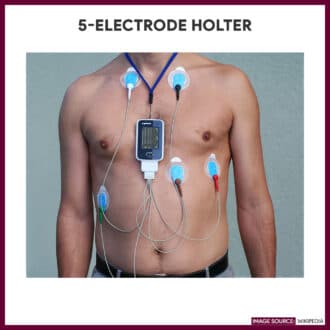
Electrodes are applied to the chest wall securely attached to the lead wires and monitor. The monitor box may be worn around the waist or over the shoulder. - Check the equipment.
A new or fully charged battery is inserted in the recorder, and the monitor box is checked for paper supply. - Activate the device.
A tape is inserted, and the box is activated. This will record and store continuous cardiac rhythm data transmitted by the electrodes. - Keep a diary.
The patient is advised to keep a diary of activities and of any cardiac symptoms such as chest pain, palpitations, dizziness, syncope, dyspnea, etc. that can occur while wearing the monitor for 24 to 72 hours. - Remove the monitor from the body.
Once the data measurement period is completed, the pads are removed and the monitor device is returned to its box. - Return the device.
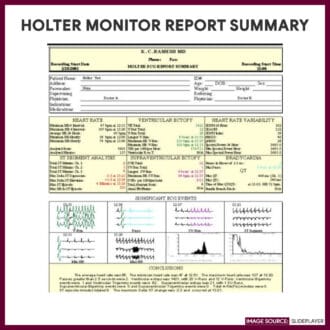
The monitor is returned to the technician where the tape is interpreted by the computer and is submitted to the requesting health care provider.
Nursing Responsibilities of Holter Monitoring
The following are the nursing interventions and nursing care considerations for a patient indicated for Holter monitoring
Before the procedure
The following are the nursing interventions before wearing a Holter monitor
- Advise the patient to wear loose-fitting clothing. This will allow the Holter monitor to stay in place and to avoid lead dislodgment.
- Provide precautionary measures. Advise patient to avoid contact with magnetic or electrical devices such as magnets, metal detectors, high-voltage areas, and electric blankets where it can interfere with the function of the monitor; Refrain from taking showers and tub bathing.
- Apply electropaste or conductive paste to the skin sites. This will provide conduction between the skin and electrodes.
- Explain the importance of maintaining a diary to record activities. The patient may perform his or her normal routine such as walking, eating, sleeping, sexual activity, emotional upsets, exercise, and ingestion of medications and to log them in a diary.
- Explain how to check the recorder to make sure it’s working properly. A light signal on the monitor will signify that an equipment malfunction or that an electrode has accidentally come off.
After the procedure
The nurse should note of the following nursing interventions after Holter monitoring
- Remove all chest electrodes. After the patient has worn the monitor, gently remove the tape and other paraphernalia securing the electrodes.
- Schedule appointment with the health care provider (HCP). The ECG recording will be interpreted by a computer and a copy of a report is printed. This will be forwarded to the HCP who will discuss the results with the patient.
Normal Results
Normal findings after Holter monitoring will show:
- No significant arrhythmias or ST-segment changes in the electrocardiogram.
- Heart changes during various activities
Abnormal Results
Abnormalities in a Holter monitoring will reveal:
- Palpitations
- Cardiomyopathy
- Dysrhythmias such as premature ventricular contractions, bradycardias, tachycardias, and conduction effects.
- Hypoxic or ischemic changes
- Mitral valve abnormality
Gallery
Images related to Holter monitoring:




References
Additional resources and references for this guide:
- Suzanne C. Smeltzer. Brunner & Suddarth’s Handbook of Laboratory and Diagnostic Tests: Lippincott Williams & Wilkins
- Anne M. Van Leeuwen, Mickey Lynn Bladh. Laboratory & Diagnostic Tests with Nursing Implications: Davis’s
- Lazzaro, M. A., Krishnan, K., & Prabhakaran, S. (2012). Detection of atrial fibrillation with concurrent Holter monitoring and continuous cardiac telemetry following ischemic stroke and transient ischemic attack. Journal of Stroke and Cerebrovascular Diseases, 21(2), 89-93. [Link]
