Use this EKG interpretation cheat sheet that summarizes all heart arrhythmias in an easy-to-understand fashion.
One of the most useful and commonly used diagnostic tools is electrocardiography (EKG) which measures the heart’s electrical activity as waveforms. An EKG uses electrodes attached to the skin to detect electric currents moving through the heart. These signals are transmitted to produce a record of cardiac activity. Arrhythmia or dysrhythmia are disturbances in the normal cardiac rhythm of the heart which occur as a result of alterations within the conduction of electrical impulses. These impulses stimulate and coordinate atrial and ventricular myocardial contractions that provide cardiac output.
Interpreting EKG
Ever wonder how nurses and doctors can read ECG papers with ease? How do they differentiate atrial tachycardia from atrial fibrillation, or how even to know what atrial fibrillation or tachycardia is?
EKG interpretation takes some great skill, a keen eye, and a good theoretical foundation on the different arrhythmias and the concepts around the heart’s conduction and the EKG machine itself. It takes time to develop a skill in interpreting EKGs, but once you get the hang of it, you’ll be able to interpret any squiggly line in the EKG paper.
Sinus Tachycardia
Sinus tachycardia is a heart rate greater than 100 beats per minute originating from the sinus node.
- Rate: 100 to 180 beats per minute
- P Waves precede each QRS complex
- PR interval is normal
- QRS complex is normal
- Conduction is normal
- Rhythm is regular
Causes of sinus tachycardia may include exercise, anxiety, fever, drugs, anemia, heart failure, hypovolemia, and shock. Sinus tachycardia is often asymptomatic. Management, however is directed at the treatment of the primary cause. Carotid sinus pressure (carotid massage) or a beta-blocker may be used to reduce heart rate.
Sinus Bradycardia
Sinus bradycardia is a heart rate of less than 60 beats per minute and originates from the sinus node (as the term “sinus” refers to the sinoatrial node). It has the following characteristics
- Rate is less than 60 beats per minute
- P Waves precede each QRS complex
- PR interval is normal
- QRS complex is normal
- Conduction is normal
- Rhythm is regular
Causes may include drugs, vagal stimulation, hypoendocrine states, hypothermia, or sinus node involvement in MI. This arrhythmia may be normal in athletes as they have quality stroke volume. It is often asymptomatic but manifestations may include: syncope, fatigue, dizziness. Management includes treating the underlying cause and administering anticholinergic drugs like atropine sulfate as prescribed.
Premature Atrial Contraction
Premature Atrial Contraction are ectopic beats that originates from the atria and they are not rhythms. Cells in the heart starts to fire or go off before the normal heartbeat is supposed to occur. These are called heart palpitations and has the following characteristics:
- Premature and abnormal-looking P waves that differ in configuration from normal P waves
- QRS complex after P waves except in very early or blocked PACs
- P waves often buried in the preceding T wave or identified in the preceding T wave.
Causes includes coronary or valvular heart diseases, atrial ischemia, coronary artery atherosclerosis, heart failure, COPD, electrolyte imbalance and hypoxia. Usually there is no treatment needed but may include procainamide and quinidine administration (antidysrhythmic drugs) and carotid sinus massage.
Atrial Flutter
Atrial flutter is an abnormal rhythm that occurs in the atria of the heart. Atrial flutter has an atrial rhythm that is regular but has an atrial rate of 250 to 400 beats/minute. It has sawtooth appearance. QRS complexes are uniform in shape but often irregular in rate.
- Normal atrial rhythm
- Abnormal atrial rate: 250 to 400 beats/minute
- Sawtooth P wave configuration
- QRS complexes uniform in shape but irregular in rate
Causes includes heart failure, tricuspid valve or mitral valve diseases, pulmonary embolism, cor pulmonale, inferior wall MI, carditis and digoxin toxicity.
Management if the patient is unstable with ventricular rate of greater than 150 bpm, prepare for immediate cardioversion. If patient is stable, drug therapy may include calcium channel blocker, beta-adrenergic blockers, or antiarhythmics. Anticoagulation may be necessary as there would be pooling of blood in the atria.
Atrial Fibrillation
Atrial fibrillation is disorganized and uncoordinated twitching of atrial musculature caused by overly rapid production of atrial impulses. This arrhythmia has the following characteristics:
- Atrial Rate: 350 to 600 bpm
- Ventricular Rate: 120 to 200 bpm
- P wave is not discernible with an irregular baseline
- PR interval is not measurable
- QRS complex is normal
- Rhythm is irregular and usually rapid unless controlled.
Causes includes atherosclerosis, heart failure, congenital heart disease, chronic obstructive pulmonary disease, hypothyroidism and thyrotoxicosis. Atrial fibrillation may be asymptomatic but clinical manifestation may include palpitations, dyspnea, and pulmonary edema. Nursing goal is towards administration of prescribed treatment to decrease ventricular response, decrease atrial irritability and eliminate the cause.
Premature Junctional Contraction
Premature Junctional Contraction (PJC) occurs when some regions of the heart becomes excitable than normal. It has the following characteristics.
- PR interval less than 0.12 seconds if P wave precedes QRS complex
- QRS complex configuration and duration is normal
- P wave is inverted
- Atrial and ventricular rhythms irregular
Causes of PJC may include myocardial infarction or ischemia, digoxin toxicity, excessive caffeine or amphetamine use. Management includes correction of underlying cause, discontinuation of digoxin if appropriate.
Atrioventricular Blocks
AV blocks are conduction defects within the AV junction that impairs conduction of atrial impulses to ventricular pathways. The three types are first degree, second degree and third degree.
First Degree AV Block
- Rate is usually 60 to 100 bpm
- PR intervals are prolonged for usually 0.20 seconds
- QRS complex is usually normal
- Rhythm is regular
First degree AV block is asymptomatic and may be caused by inferior wall MI or ischemia, hyperkalemia, hypokalemia, digoxin toxicity, calcium channel blockers, amiodarone and use of antidysrhythmics. Management includes correction of underlying cause. Administer atropine if PR interval exceeds 0.26 second or symptomatic bradycardia develops.
Second Degree AV Block Mobitz I (Wenckebach)
- Atrial rhythm is regular
- Ventricular rhythm is irregular
- Atrial rate exceeds ventricular rate
- PR interval progressively but only slightly, longer with each cycle until QRS complex disappears (dropped beat)
- PR Interval shorter after dropped beat.
Clinical manifestations include vertigo, weakness, and an irregular pulse. This may be caused by Inferior wall MI, cardiac surgery, acute rheumatic fever, vagal stimulation. Treatment includes correction of underlying cause, atropine or temporary pacemaker for symptomatic bradycardia and discontinuation of digoxin if appropriate.
Second Degree AV Block Mobitz II
- Atrial rhythm is regular
- Ventricular rhythm maybe regular or irregular depending on the degree of block
- P-P interval constant
- QRS complex periodically absent or disappears
Clinical manifestations same as Mobitz I. Causes includes: severe coronary artery diseases, anterior wall MI, acute myocarditis and digoxin toxicity. Treatment includes: atropine, epinephrine, and dopamine for symptomatic bradycardia. Discontinuation of digoxin if appropriate. Installation of pacemaker.
Third Degree AV Block (Complete Heart Block)
- Atrial rhythm regular
- Ventricular rhythm regular and rate slower than atrial rate
- No relation between P waves and QRS complexes
- NO constant PR interval
- QRS interval normal or wide and bizarre
Manifestations include hypotension, angina, and heart failure. This may be caused by congenital abnormalities, rheumatic fever, hypoxia, MI, LEv’s disease, Lenegre’s disease and digoxin toxicity. Management includes atropine, epinephrine, and dopamine for bradycardia. Installation of pacemaker may also be considered.
Premature Ventricular Contractions (PVC)
Early or premature ventricular contractions are caused by increased automaticity of ventricular muscle cells. PVCs usually are not considered harmful but are of concern if more than six occur in 1 minute, if they occur in pairs or triplets if they are multifocal or if they occur or near a T wave.
- Atrial rhythm is regular
- Ventricular rhythm is irregular
- QRS complex premature, usually followed by a complete compensatory pause
- QRS complex is also wide and distorted, usually >0.14 second.
- Premature QRS complexes occurring singly, in pairs, or in threes
Clinical manifestations includes palpitations, weakness, lightheadedness but it is most of the time asymptomatic. Management includes assessment of the cause and treat as indicated. Treatment is indicated if the client has underlying disease because PVCs may precipitate ventricular tachycardia or fibrillation. Assess for life threatening PVCs. Administer antiarrhythmic medication as prescribed.
Ventricular Tachycardia
Ventricular tachycardia (VT) is three or more consecutive PVCs. it is considered a medical emergency because cardiac output (CO) cannot be maintained because of decreased diastolic filling (preload).
- Rate is 100 to 250 beats per minute
- P wave is blurred in the QRS complex but the QRS complex has no associate with P wave.
- PR Interval is not present
- QRS complex is wide and bizarre; T wave is in the opposite direction
- Rhythm is usually regular
- May start and stop suddenly
Clinical manifestations of VT includes lightheadedness, weakness, dyspnea and unconsciousness. Causes includes MI, aneurysm, CAD, rheumatic heart diseases, mitral valve prolapse, hypokalemia, hyperkalemia, and pulmonary embolism. Anxiety may also caused VT.
Pulseless Ventricular Tachycardia
Management for Pulseless VT: Initiate cardiopulmonary resuscitation; follow ACLS protocol for defibrillation, ET intubation and administration of epinephrine or vasopressin.
Ventricular Tachycardia with Pulse
Management with Pulse VT: If hemodynamically stable, follow ACLS protocol for administration of amiodarone, if ineffective, initiate synchronized cardioversion.
Ventricular Fibrillation
Ventricular fibrillation is rapid, ineffective quivering of ventricles that may be rapidly fatal.
- Rate is rapid and uncoordinated, with ineffective contractions
- Rhythm is chaotic
- QRS complexes wide and irregular
- P wave is not seen
- PR interval is not seen
Causes of ventricular fibrillation is most commonly myocardia ischemia or infarction. It ma result from untreated ventricular tachycardia, electrolyte imbalances, digoxin or quinide toxicity, or hypothermia. Clinical manifestations may include loss of consciousness, pulselessness, loss of blood pressure, cessation of respirations, possible seizures and sudden death.
Start CPR is pulseless. Follow ACLS protocol for defibrillation, ET intubation and administration of epinephrine or vasopressin.
Other Arrhythmias
Atrial Tachycardia
2nd Degree AV Block Type 1, Mobitz I
Torsade de Pointes
Pulseless Ventricular Tachycardia
Supraventricular Tachycardia
ST Depression
EKG Interpretation Cheat Sheets
Download the printable cheat sheet for EKG interpretation below. To download, simply click on the images below and save.

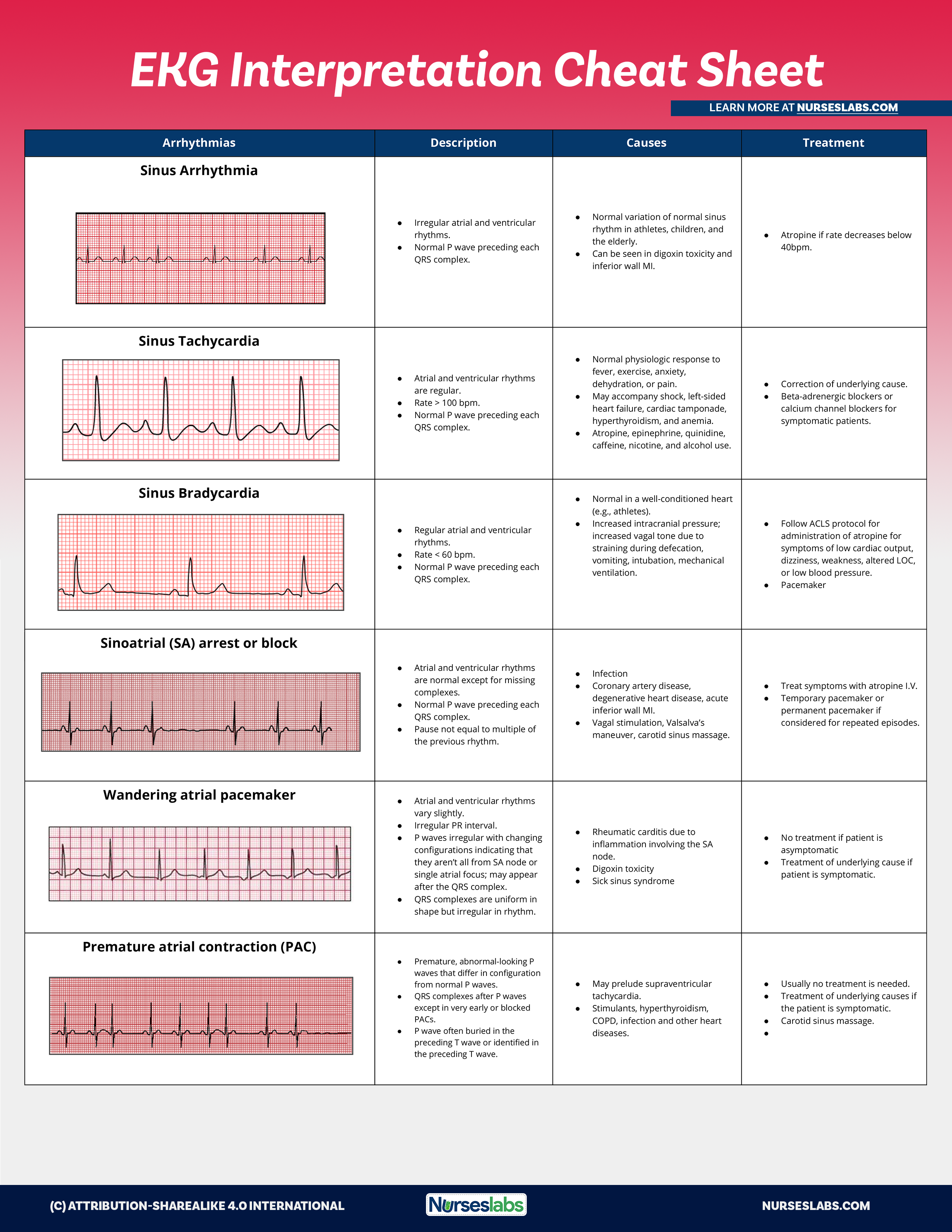
| Arrhythmias | Description | Causes | Treatment |
|---|---|---|---|
| Sinus Arrhythmia |
|
|
|
| Sinus Tachycardia |
|
|
|
| Sinus Bradycardia |
|
|
|
| Sinoatrial (SA) arrest or block |
|
| |
| Wandering atrial pacemaker |
|
|
|
| Premature atrial contraction (PAC) |
|
|
|
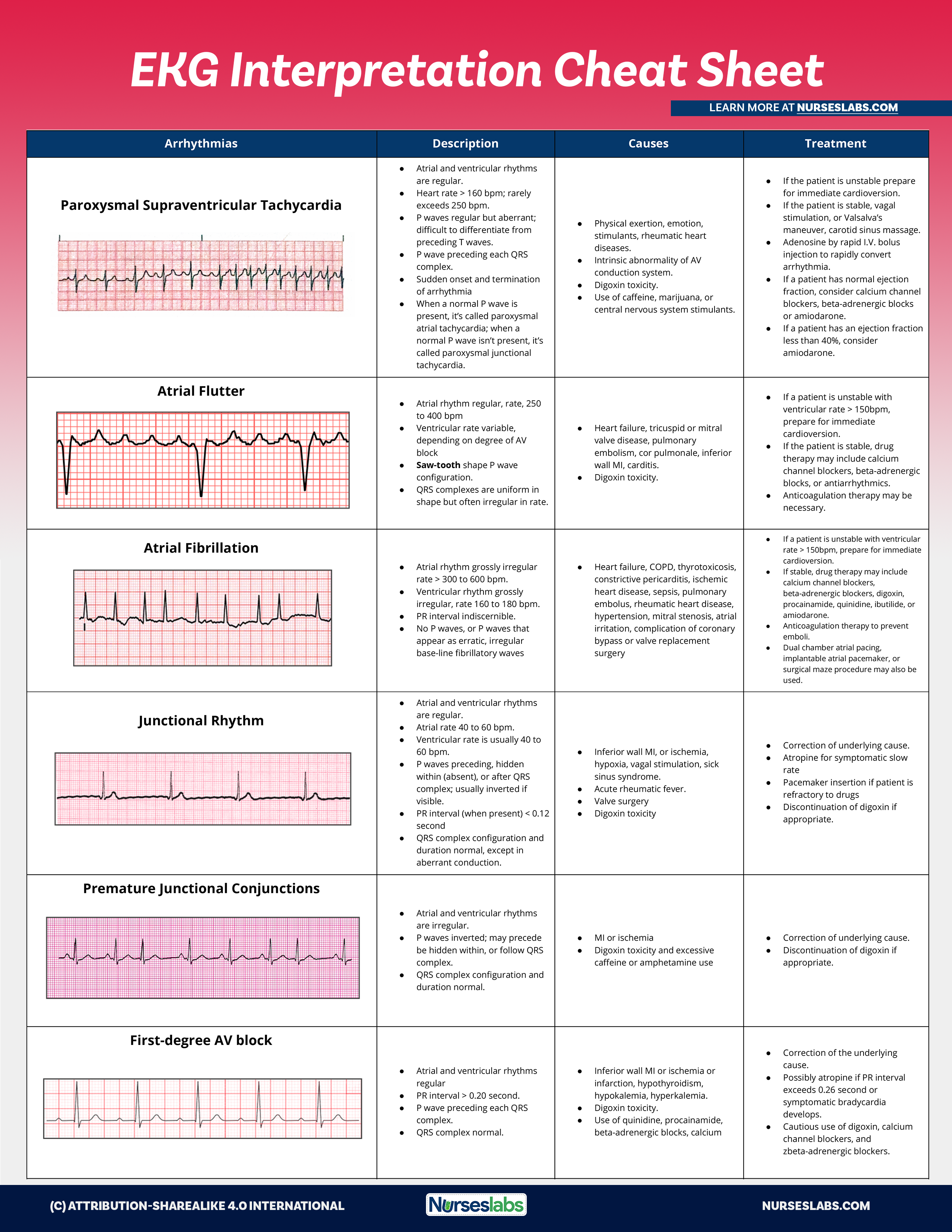
| Paroxysmal Supraventricular Tachycardia |
|
|
|
| Atrial flutter |
|
|
|
| Atrial Fibrillation |
|
|
|
| Junctional Rhythm |
|
| |
| Premature Junctional Conjunctions |
|
|
|
| First-degree AV block |
|
|
|
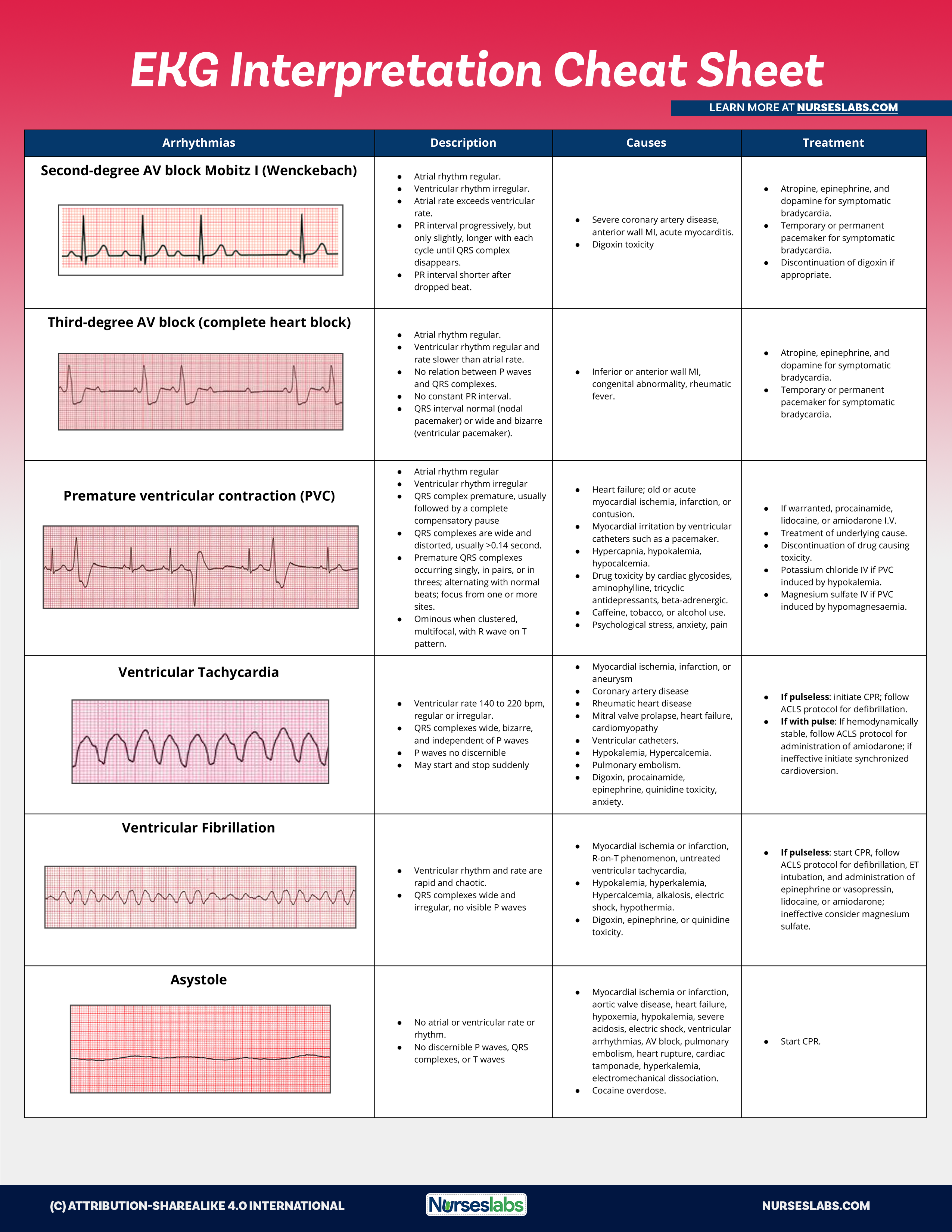
| Second-degree AV block Mobitz I (Wenckebach) |
|
|
|
| Third-degree AV block (complex heart block) |
|
|
|
| Premature ventricular contraction (PVC) |
|
| |
| Ventricular Tachycardia |
|
|
|
| Ventricular Fibrillation |
|
|
|
| Asystole |
|
|
|





























Leave a Comment