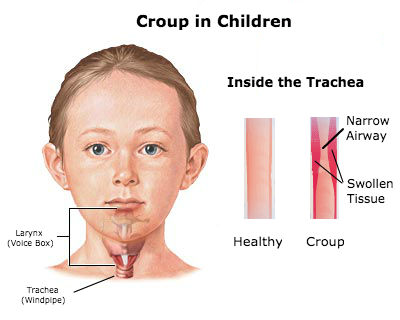
Croup, a common childhood respiratory condition, is characterized by inflammation and swelling of the upper airway, primarily affecting the vocal cords and the area below the vocal cords (subglottic region). This condition is most prevalent in young children, often occurring in children between the ages of 6 months and 3 years. The hallmark symptom of croup is a harsh, barking cough, often accompanied by stridor (a high-pitched, crowing sound) and respiratory distress.
Understanding the essentials of croup is crucial for nurses in recognizing and managing this transient yet distressing respiratory condition, promoting health education, and reassuring parents during the child’s recovery.
Table of Contents
- What is Croup Syndrome?
- Pathophysiology
- Statistics and Incidences
- Causes
- Clinical Manifestations
- Assessment and Diagnostic Findings
- Medical Management
- Nursing Management
What is Croup Syndrome?
Croup is a common, primarily pediatric viral respiratory tract illness.
- Croup is the most common etiology for hoarseness, cough, and the onset of acute stridor in febrile children.
- As its alternative names, acute laryngotracheitis and acute laryngotracheobronchitis, indicate, croup generally affects the larynx and trachea, although this illness may also extend to the bronchi.
- This respiratory illness, recognized by physicians for centuries, derives its name from an Anglo-Saxon word, kropan, or from an old Scottish word, roup, meaning to cry out in a hoarse voice.
Pathophysiology
Viruses causing acute infectious croup are spread through either direct inhalation from a cough and/or sneeze, or by contamination of hands from contact with fomites with subsequent touching the mucosa of the eyes, nose, and/or mouth.

- The primary ports of viral entry are the nose and nasopharynx.
- The infection spreads and eventually involves the larynx and trachea.
- Inflammation and edema of the subglottic larynx and trachea, especially near the cricoid cartilage, are most clinically significant.
- Histologically, the involved area is edematous, with cellular infiltration located in the lamina propria, submucosa, and adventitia.
- This narrowing results in the seal-like barky cough, turbulent airflow, stridor, and chest wall retractions.
- Decreased mobility of the vocal cords due to edema leads to the associated hoarseness.
Statistics and Incidences
Croup is the most common pediatric illness that causes acute stridor, accounting for approximately 15% of annual clinic and emergency department visits for pediatric respiratory tract infections.
- Croup is primarily a disease of infants and toddlers, with an age peak incidence of age 6 months to 36 months (3 years).
- In North America, incidence peaks in the second year of life, with an incidence of about 5-6 cases per 100 toddlers.
- Although uncommon after age 6 years, croup may be diagnosed in the preteen and adolescent years, and rarely in adults.
- The male-to-female ratio for croup is approximately 1.4:1.
- The disease occurs most often in late fall and early winter, but may present at any time of the year.
- Approximately 5% of children will experience more than 1 episode.
Causes
Viruses causing acute infectious croup are spread through either direct inhalation from a cough and/or sneeze, or by contamination of hands from contact with fomites with subsequent touching the mucosa of the eyes, nose, and/or mouth.
- Parainfluenza viruses. Parainfluenza viruses (types 1, 2, 3) are responsible for about 80% of croup cases, with parainfluenza types 1 and 2, accounting for nearly 66% of cases.
- Mycoplasma pneumoniae. The bacterial pathogen, Mycoplasma pneumoniae, has also been identified in a few cases of croup.
Clinical Manifestations
Croup usually begins with nonspecific respiratory symptoms.
- Coryza. The attack may be preceded by coryza (runny nose) and hoarseness or by no apparent signs of respiratory irregularity during the evening.
- Fever. Fever is generally low grade (38-39°C) but can exceed 40°C.
- Respiratory symptoms. Within 1-2 days, the characteristic signs of hoarseness, barking cough, and inspiratory stridor develop, often suddenly, along with a variable degree of respiratory distress; symptoms are perceived as worsening at night, with most emergency room visits occurring between the hours of 10 pm and 4 am.
- Spasmodic croup. Spasmodic croup (recurrent croup) typically presents at night with the sudden onset of “croupy” cough and stridor.
Assessment and Diagnostic Findings
Croup is primarily a clinical diagnosis, with diagnostic clues based on presenting history and physical examination findings.
- Pulse oximetry. Pulse oximetry readings are within the normal reference range for most patients; however, this monitoring is helpful to assess for the need for supplemental oxygen support and to monitor for worsening respiratory compromise as evident with tachypnea and poor maintenance of oxygen saturations.
- Radiography. Radiographs can be used as a tool to help confirm this diagnosis, but are not required in uncomplicated cases.
Medical Management
Urgent care or emergency department treatment of croup depends on the patient’s degree of respiratory distress.
- Corticosteroids. Corticosteroids are beneficial due to their anti-inflammatory action; their use decreases both laryngeal mucosal edema and the need for salvage nebulized epinephrine; corticosteroids may be warranted even in those children who present with mild symptoms.
- Epinephrine. Patients who receive nebulized racemic epinephrine in the emergency department should be observed for at least 3 hours post-treatment because of concerns for a return of bronchospasm, worsening respiratory distress, and/or persistent tachycardia; patients can be discharged home only if they demonstrate clinical stability with good air entry, baseline consciousness, no stridor at rest and have received a dose of corticosteroids.
- Heliox. Heliox is a gas that contains a mixture of helium and oxygen (with not less than 20% oxygen); delivery to the patient is via nasal cannula, face mask, or hood; it has low viscosity and low specific gravity, which allows for greater laminar airflow through the respiratory tract; helium facilitates the movement of oxygen through the airways and decreases the mechanical work of respiratory muscles; this clinical response reduces respiratory distress.
Pharmacologic Management
As previously mentioned, current treatment approaches for patients with croup are corticosteroids and nebulized epinephrine; steroids have proven beneficial in severe, moderate, and even mild croup.
- Corticosteroids. Steroids are thought to decrease airway edema via their anti-inflammatory effect; corticosteroids have been shown to reduce hospitalization rates by 86%, and in mild disease, they have been proven to reduce the number of children returning to the ED for further treatment.
- Epinephrine. Epinephrine stimulates alpha receptors and beta2 receptors; it constricts the precapillary arterioles, thus decreasing airway edema; because of the potential adverse effects of tachycardia and hypertension, it is reserved for children with moderate to severe disease.
Nursing Management
In mild croup, a child may present with only a croupy cough and may just require parental guidance and reassurance, given alertness, baseline minimal respiratory distress, proper oxygenation, and stable fluid status.
Nursing Assessment
- History. The initial assessment should be made whilst taking the history; the child can be observed, preferably whilst seated on the parent’s lap at a non-threatening distance; much information can be obtained without having to disturb the child.
- Respiratory status. The respiratory rate can be assessed, as can the use of accessory muscles of respiration, tracheal tug, and the presence (or absence) of central cyanosis.
- General appearance. A child, who is agitated, appears to be tired from the effort of breathing, or has a decreasing level of consciousness needs to be closely monitored.
- Degree of respiratory distress. The presence of stridor at rest, tracheal tug, chest wall retractions, changing respiratory rate, and pulse rate indicate treatment is necessary.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses are:
- Ineffective airway clearance related to presence of thick, tenacious mucus, and swelling or spasm of the epiglottis.
- Deficient fluid volume related to decreased ability or aversion to swallowing, presence of fever, and increased respiratory losses.
Nursing Care Planning and Goals
The goals for a child with croup include:
- Patient will maintain clear, open airways as evidence by normal breath sounds, normal rate and depth of respirations, and ability to effectively cough up secretions after treatments and deep breaths.
- Patient will demonstrate increased air exchange.
- Patient will classify methods to enhance secretion removal.
- Patient will recognize the significance of changes in sputum to include color, character, amount, and odor.
- Patient will identify and avoid specific factors that inhibit effective airway clearance.
- Patient is normovolemic as evidenced by systolic BP greater than or equal to 90 mm HG (or patient’s baseline), absence of orthostasis, HR 60 to 100 beats/min, urine output greater than 30 mL/hr and normal skin turgor.
- Patient demonstrates lifestyle changes to avoid progression of dehydration.
- Patient verbalizes awareness of causative factors and behaviors essential to correct fluid deficit.
Nursing Interventions
Nursing treatment for a child with croup must focus on:
- Humidified air. Cool mist from a humidifier and/or sitting with the child in a bathroom (not in the shower) filled with steam generated by running hot water from the shower, help minimize symptoms.
- Antipyretics. Treat fever with an antipyretic such as acetaminophen or ibuprofen.
- Fluid intake. Encourage oral intake and frozen juice popsicles also can be given to ease throat soreness.
- Education on smoking. Educate caregivers to avoid smoking in the home; smoke can worsen a child’s cough.
- Head elevation. Keep the child’s head elevated; an infant can be placed in a car seat; a child may be propped up in bed with an extra pillow; and pillows should not be used with infants younger than 12 months of age.
- Decreasing anxiety. Young children should be kept as comfortable as possible, allowing him or her to remain in a parent’s arms and avoiding unnecessary painful interventions that may cause agitation, and respiratory distress, and lead to increased oxygen requirements; persistent crying increases oxygen demands, and respiratory muscle fatigue can worsen the airway obstruction.
- Vital signs monitoring. Concurrently, careful monitoring of heart rate (for tachycardia), respiratory rate (for tachypnea), respiratory mechanics (for sternal wall retractions), and pulse oximetry (for hypoxia) are important.
- Cool mist administration. Historically, cool mist administration was the mainstay of treatment for croup; hospitals had “croup rooms” filled with cool mist; theoretically, mist moistens airway secretions, decreases their viscosity, and soothes the inflamed mucosa.
Evaluation
Goals are met as evidenced by:
- Patient maintained clear, open airways as evidence by normal breath sounds, normal rate and depth of respirations, and ability to effectively cough up secretions after treatments and deep breaths.
- Patient demonstrated increased air exchange.
- Patient classified methods to enhance secretion removal.
- Patient recognized the significance of changes in sputum to include color, character, amount, and odor.
- Patient identified and avoid specific factors that inhibit effective airway clearance.
- Patient is normovolemic as evidenced by systolic BP greater than or equal to 90 mm HG (or patient’s baseline), absence of orthostasis, HR 60 to 100 beats/min>urine output greater than 30 mL/hr and normal skin turgor.
- Patient demonstrated lifestyle changes to avoid progression of dehydration
- Patient verbalized awareness of causative factors and behaviors essential to correct fluid deficit.
Documentation Guidelines
- Breath sounds, presence and character of secretions, use of accessory muscles for breathing.
- Plan of care.
- Teaching plan.
- Responses to interventions, and actions performed.
- Attainment or progress towards desired outcomes.
- Modifications to plan of care.