Breathe life into your understanding with our guide on the respiratory system anatomy and physiology. Nursing students, immerse yourself in the intricate dance of inhalation and exhalation that fuels every living moment.
Table of Contents
- Functions of the Respiratory System
- Anatomy of the Respiratory System
- Physiology of the Respiratory System
- Age-Related Physiological Changes in the Respiratory System
- See also
Functions of the Respiratory System
The functions of the respiratory system are:
- Oxygen supplier. The job of the respiratory system is to keep the body constantly supplied with oxygen.
- Elimination. Elimination of carbon dioxide.
- Gas exchange. The respiratory system organs oversee the gas exchanges that occur between the blood and the external environment.
- Passageway. Passageways that allow air to reach the lungs.
- Humidifier. Purify, humidify, and warm incoming air.
Anatomy of the Respiratory System
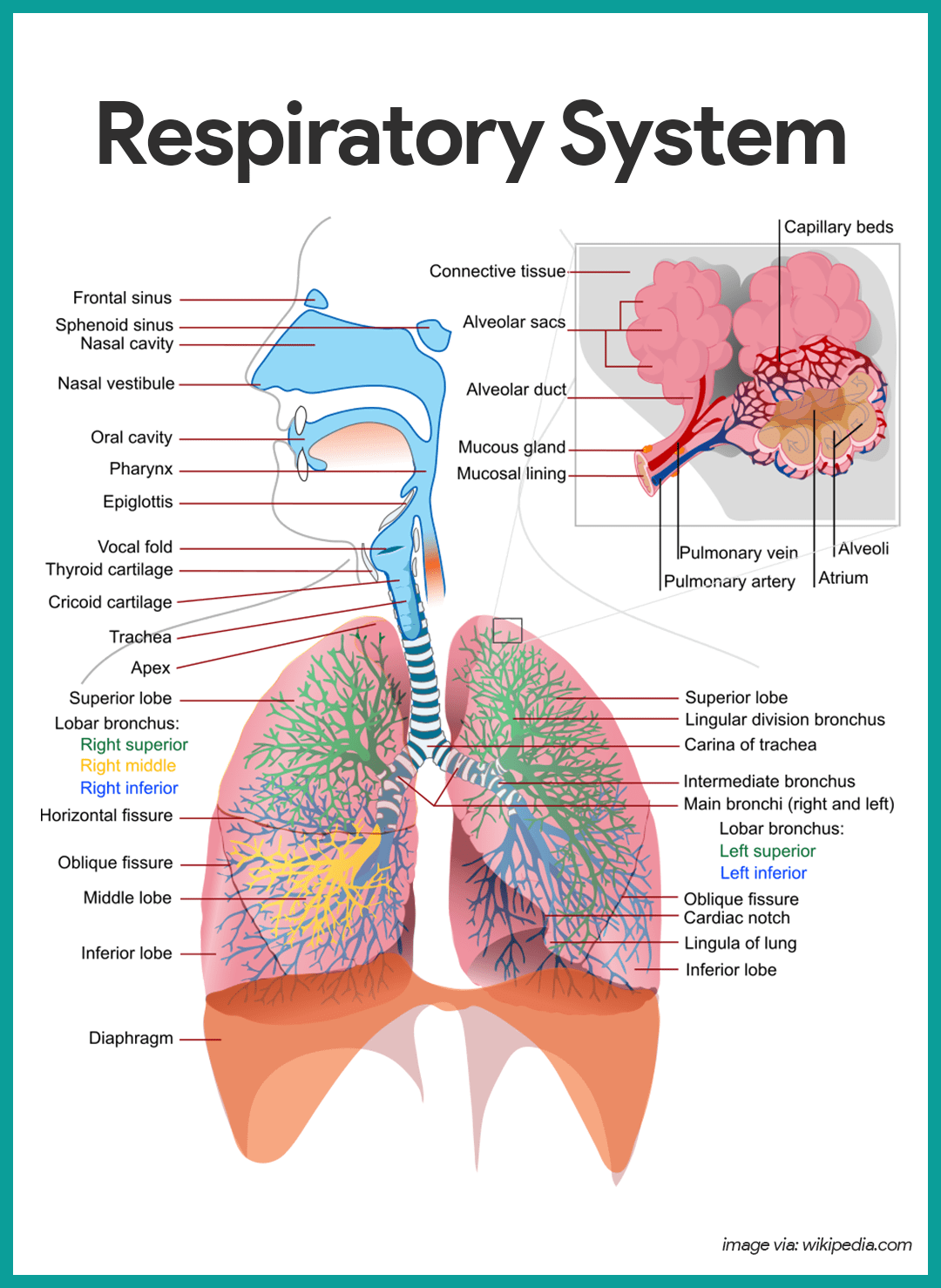
The organs of the respiratory system include the nose, pharynx, larynx, trachea, bronchi, and their smaller branches, and the lungs, which contain the alveoli.
The Nose
The nose is the only externally visible part of the respiratory system.
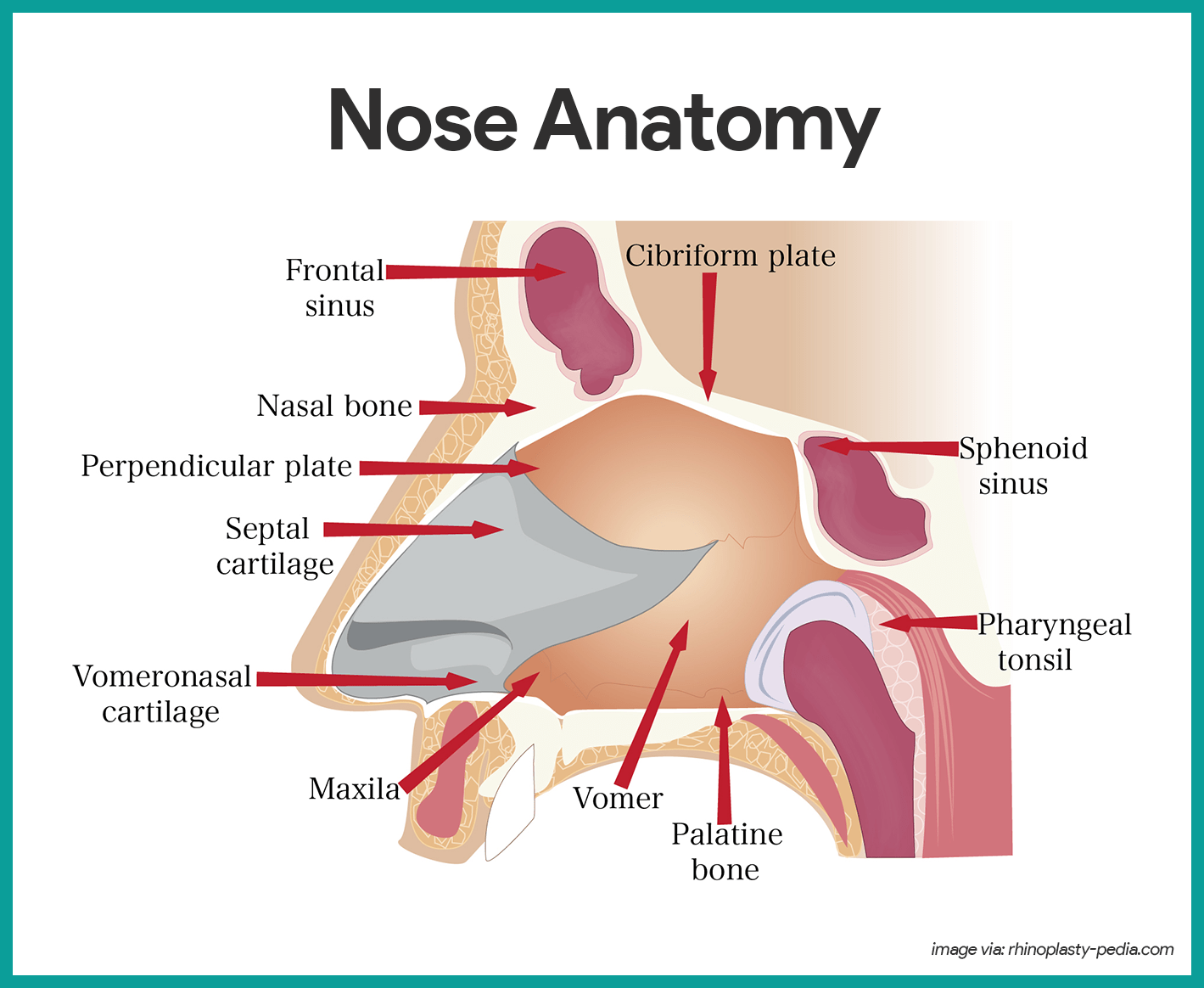
- Nostrils. During breathing, air enters the nose by passing through the nostrils, or nares.
- Nasal cavity. The interior of the nose consists of the nasal cavity, divided by a midline nasal septum.
- Olfactory receptors. The olfactory receptors for the sense of smell are located in the mucosa in the slitlike superior part of the nasal cavity, just beneath the ethmoid bone.
- Respiratory mucosa. The rest of the mucosal lining, the nasal cavity called the respiratory mucosa, rests on a rich network of thin-walled veins that warms the air as it flows past.
- Mucus. In addition, the sticky mucus produced by the mucosa’s glands moistens the air and traps incoming bacteria and other foreign debris, and lysozyme enzymes in the mucus destroy bacteria chemically.
- Ciliated cells. The ciliated cells of the nasal mucosa create a gentle current that moves the sheet of contaminated mucus posteriorly toward the throat, where it is swallowed and digested by stomach juices.
- Conchae. The lateral walls of the nasal cavity are uneven owing to three mucosa-covered projections, or lobes called conchae, which greatly increase the surface area of the mucosa exposed to the air, and also increase the air turbulence in the nasal cavity.
- Palate. The nasal cavity is separated from the oral cavity below by a partition, the palate; anteriorly, where the palate is supported by bone, is the hard palate; the unsupported posterior part is the soft palate.
- Paranasal sinuses. The nasal cavity is surrounded by a ring of paranasal sinuses located in the frontal, sphenoid, ethmoid, and maxillary bones; theses sinuses lighten the skull, and they act as a resonance chamber for speech.
Pharynx
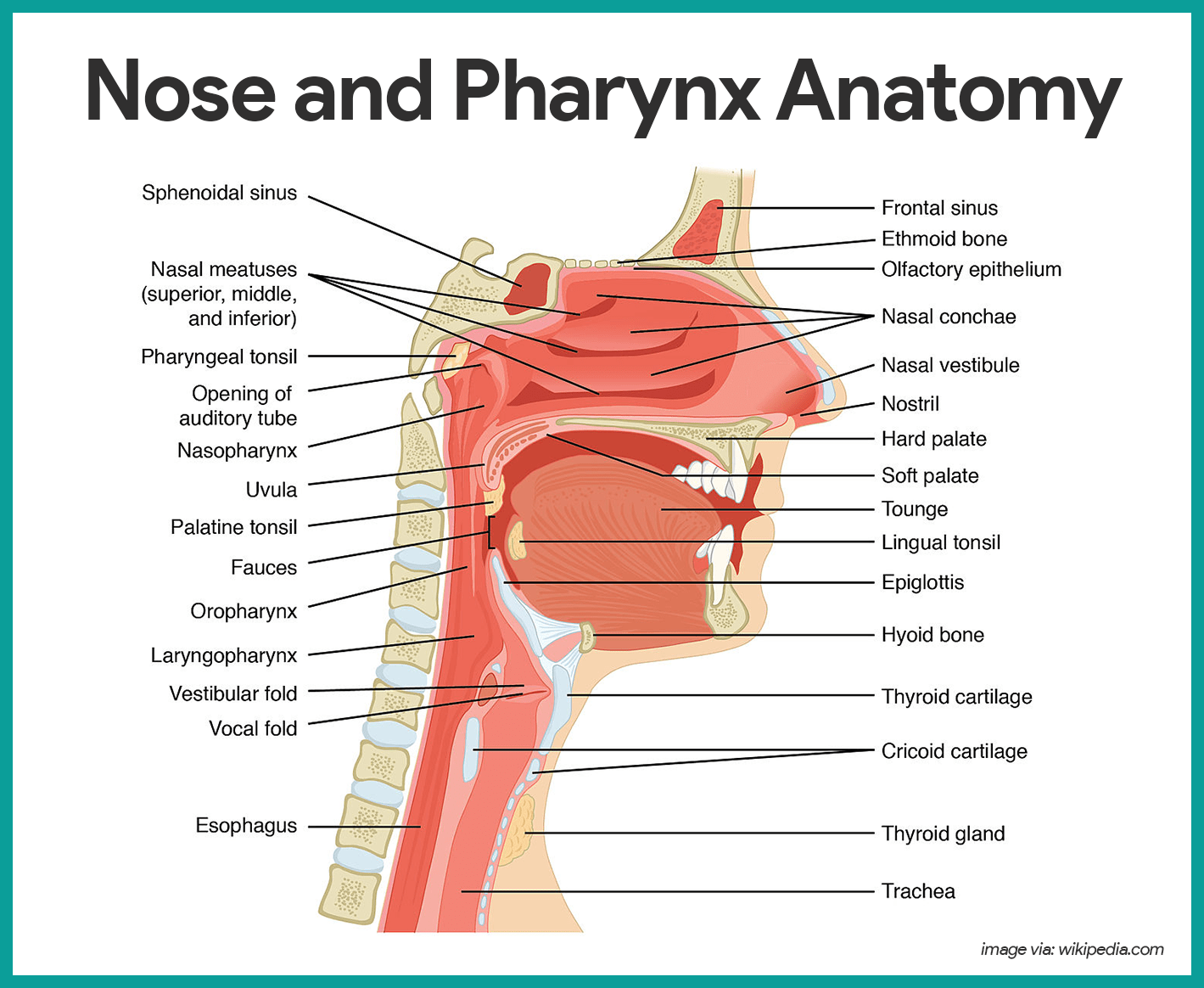
- Size. The pharynx is a muscular passageway about 13 cm (5 inches) long that vaguely resembles a short length of red garden hose.
- Function. Commonly called the throat, the pharynx serves as a common passageway for food and air.
- Portions of the pharynx. Air enters the superior portion, the nasopharynx, from the nasal cavity and then descends through the oropharynx and laryngopharynx to enter the larynx below.
- Pharyngotympanic tube. The pharyngotympanic tubes, which drain the middle ear open into the nasopharynx.
- Pharyngeal tonsil. The pharyngeal tonsil, often called adenoid is located high in the nasopharynx.
- Palatine tonsils. The palatine tonsils are in the oropharynx at the end of the soft palate.
- Lingual tonsils. The lingual tonsils lie at the base of the tongue.
Larynx
The larynx or voice box routes air and food into the proper channels and plays a role in speech.
- Structure. Located inferior to the pharynx, it is formed by eight rigid hyaline cartilages and a spoon-shaped flap of elastic cartilage, the epiglottis.
- Thyroid cartilage. The largest of the hyaline cartilages is the shield-shaped thyroid cartilage, which protrudes anteriorly and is commonly called Adam’s apple.
- Epiglottis. Sometimes referred to as the “guardian of the airways”, the epiglottis protects the superior opening of the larynx.
- Vocal folds. Part of the mucous membrane of the larynx forms a pair of folds, called the vocal folds, or true vocal cords, which vibrate with expelled air and allows us to speak.
- Glottis. The slitlike passageway between the vocal folds is the glottis.
Trachea
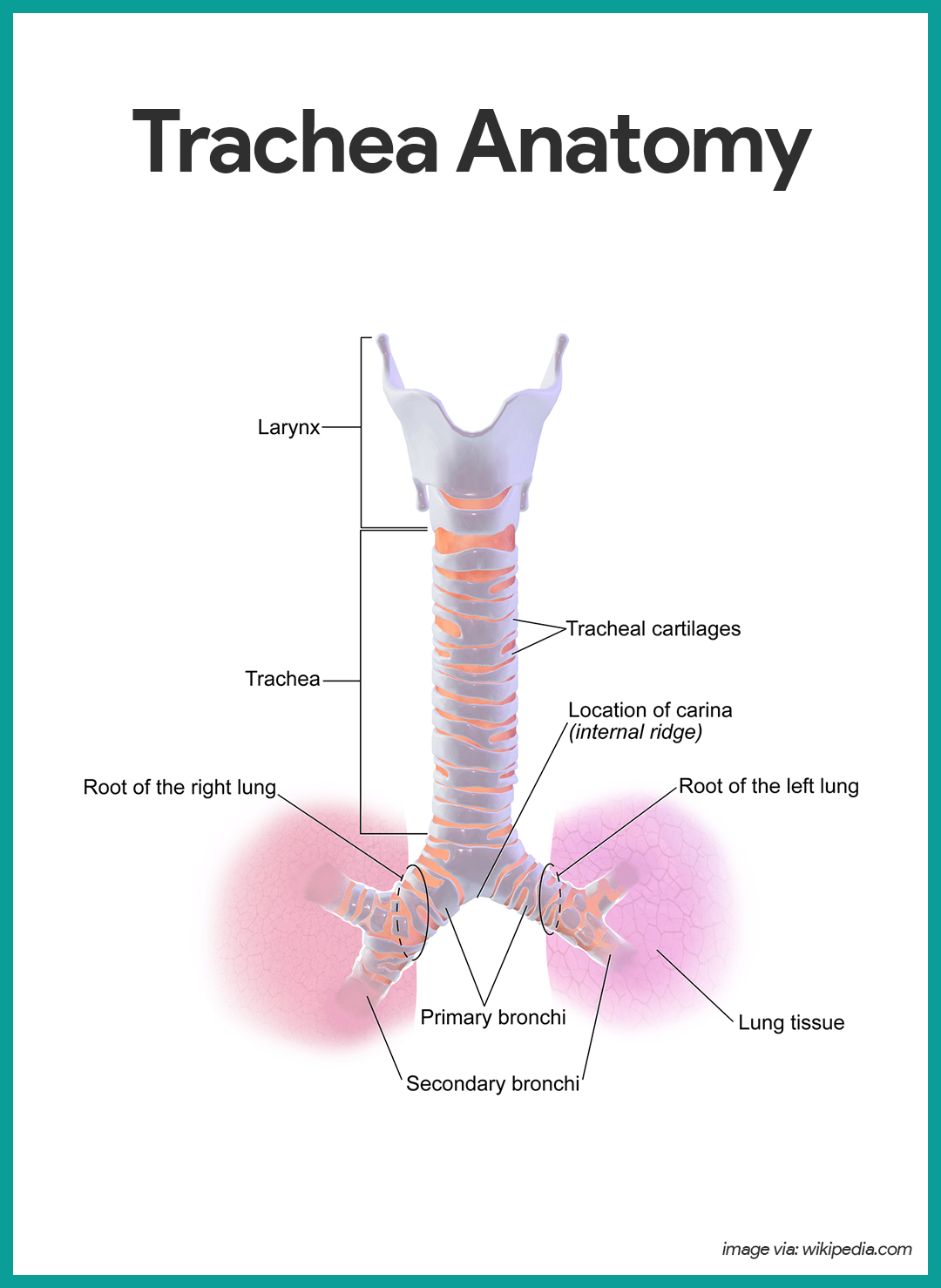
- Length. Air entering the trachea or windpipe from the larynx travels down its length (10 to 12 cm or about 4 inches) to the level of the fifth thoracic vertebra, which is approximately midchest.
- Structure. The trachea is fairly rigid because its walls are reinforced with C-shaped rings of hyaline cartilage; the open parts of the rings abut the esophagus and allow it to expand anteriorly when we swallow a large piece of food, while the solid portions support the trachea walls and keep it patent, or open, in spite of the pressure changes that occur during breathing.
- Cilia. The trachea is lined with ciliated mucosa that beat continuously and in a direction opposite to that of the incoming air as they propel mucus, loaded with dust particles and other debris away from the lungs to the throat, where it can be swallowed or spat out.
Main Bronchi
- Structure. The right and left main (primary) bronchi are formed by the division of the trachea.
- Location. Each main bronchus runs obliquely before it plunges into the medial depression of the lung on its own side.
- Size. The right main bronchus is wider, shorter, and straighter than the left.
Lungs
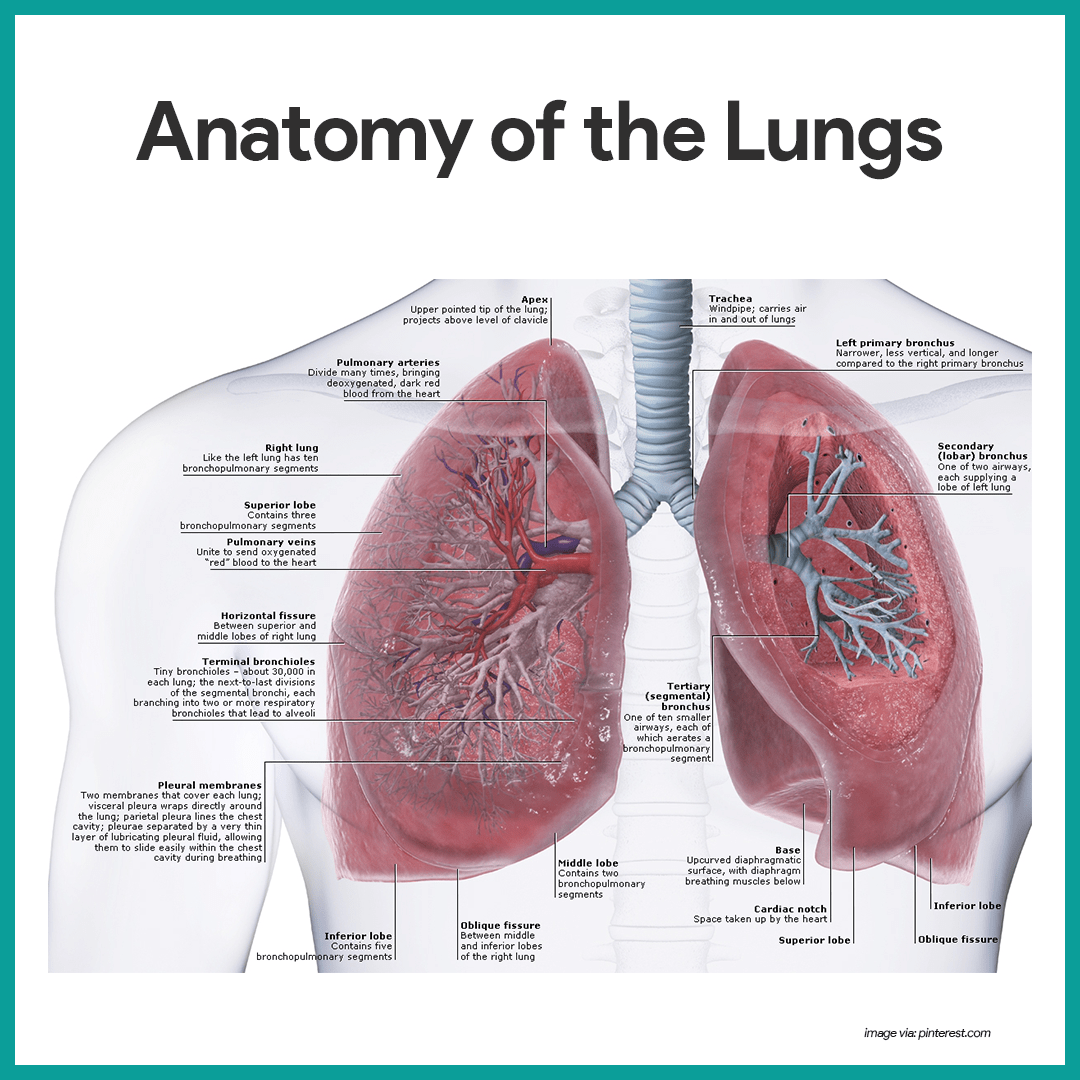
- Location. The lungs occupy the entire thoracic cavity except for the most central area, the mediastinum, which houses the heart, the great blood vessels, bronchi, esophagus, and other organs.
- Apex. The narrow, superior portion of each lung, the apex, is just deep into the clavicle.
- Base. The broad lung area resting on the diaphragm is the base.
- Division. Each lung is divided into lobes by fissures; the left lung has two lobes, and the right lung has three.
- Pleura. The surface of each lung is covered with a visceral serosa called the pulmonary, or visceral pleura, and the walls of the thoracic cavity are lined by the parietal pleura.
- Pleural fluid. The pleural membranes produce pleural fluid, a slippery serous secretion that allows the lungs to glide easily over the thorax wall during breathing movements and causes the two pleural layers to cling together.
- Pleural space. The lungs are held tightly to the thorax wall, and the pleural space is more of a potential space than an actual one.
- Bronchioles. The smallest of the conducting passageways are the bronchioles.
- Alveoli. The terminal bronchioles lead to the respiratory zone structures, even smaller conduits that eventually terminate in alveoli or air sacs.
- Respiratory zone. The respiratory zone, which includes the respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli, is the only site of gas exchange.
- Conducting zone structures. All other respiratory passages are conducting zone structures that serve as conduits to and from the respiratory zone.
- Stroma. The balance of the lung tissue, its stroma, is mainly elastic connective tissue that allows the lungs to recoil passively as we exhale.
The Respiratory Membrane
- Wall structure. The walls of the alveoli are composed largely of a single, thin layer of squamous epithelial cells.
- Alveolar pores. Alveolar pores connect neighboring air sacs and provide alternative routes for air to reach alveoli whose feeder bronchioles have been clogged by mucus or otherwise blocked.
- Respiratory membrane. Together, the alveolar and capillary walls, their fused basement membranes, and occasional elastic fibers construct the respiratory membrane (air-blood barrier), which has gas (air) flowing past on one side and blood flowing past on the other.
- Alveolar macrophages. Remarkably efficient alveolar macrophages sometimes called “dust cells”, wander in and out of the alveoli picking up bacteria, carbon particles, and other debris.
- Cuboidal cells. Also scattered amid the epithelial cells that form most of the alveolar walls are chunky cuboidal cells, which produce a lipid (fat) molecule called surfactant, which coats the gas-exposed alveolar surfaces and is very important in lung function.
Physiology of the Respiratory System
The major function of the respiratory system is to supply the body with oxygen and to dispose of carbon dioxide. To do this, at least four distinct events, collectively called respiration, must occur.
Respiration
- Pulmonary ventilation. Air must move into and out of the lungs so that gasses in the air sacs are continuously refreshed, and this process is commonly called breathing.
- External respiration. Gas exchange between the pulmonary blood and alveoli must take place.
- Respiratory gas transport. Oxygen and carbon dioxide must be transported to and from the lungs and tissue cells of the body via the bloodstream.
- Internal respiration. At systemic capillaries, gas exchanges must be made between the blood and tissue cells.
Mechanics of Breathing
- Rule. Volume changes lead to pressure changes, which lead to the flow of gasses to equalize pressure.
- Inspiration. Air is flowing into the lungs; the chest is expanded laterally, the rib cage is elevated, and the diaphragm is depressed and flattened; lungs are stretched to the larger thoracic volume, causing the intrapulmonary pressure to fall and air to flow into the lungs.
- Expiration. Air is leaving the lungs; the chest is depressed and the lateral dimension is reduced, the rib cage is descended, and the diaphragm is elevated and dome-shaped; lungs recoil to a smaller volume, intrapulmonary pressure rises, and air flows out of the lung.
- Intrapulmonary volume. Intrapulmonary volume is the volume within the lungs.
- Intrapleural pressure. The normal pressure within the pleural space, the intrapleural pressure, is always negative, and this is the major factor preventing the collapse of the lungs.
- Nonrespiratory air movements. Nonrespiratory movements are a result of reflex activity, but some may be produced voluntarily such as coughing, sneezing, crying, laughing, hiccups, and yawning.
Respiratory Volumes and Capacities
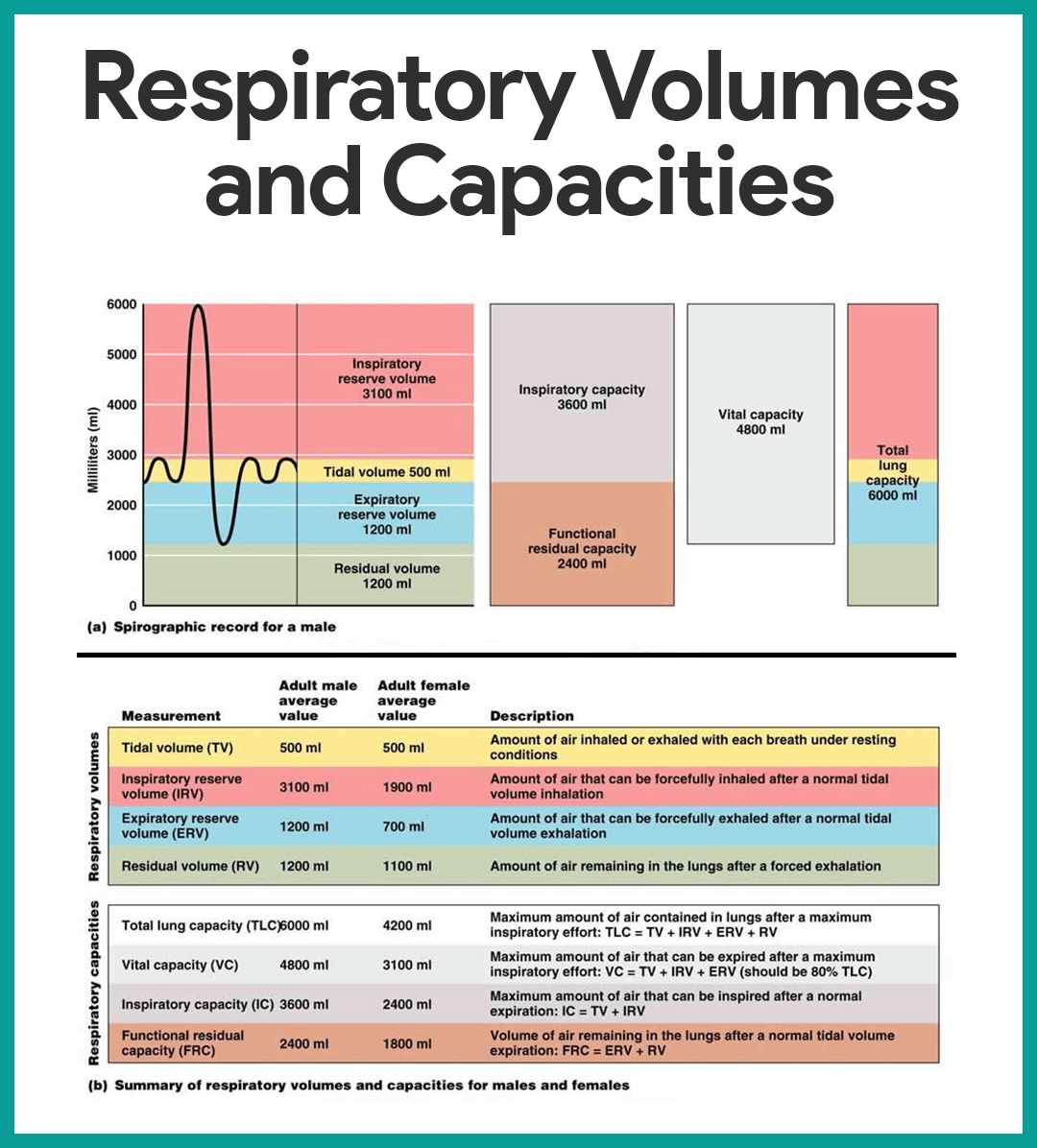
- Tidal volume. Normal quiet breathing moves approximately 500 ml of air into and out of the lungs with each breath.
- Inspiratory reserve volume. The amount of air that can be taken in forcibly over the tidal volume is the inspiratory reserve volume, which is normally between 2100 ml to 3200 ml.
- Expiratory reserve volume. The amount of air that can be forcibly exhaled after a tidal expiration, the expiratory reserve volume, is approximately 1200 ml.
- Residual volume. Even after the most strenuous expiration, about 1200 ml of air still remains in the lungs and it cannot be voluntarily expelled; this is called residual volume, and it is important because it allows gas exchange to go on continuously even between breaths and helps to keep the alveoli inflated.
- Vital capacity. The total amount of exchangeable air is typically around 4800 ml in healthy young men, and this respiratory capacity is the vital capacity, which is the sum of the tidal volume, inspiratory reserve volume, and expiratory reserve volume.
- Dead space volume. Much of the air that enters the respiratory tract remains in the conducting zone passageways and never reaches the alveoli; this is called the dead space volume and during a normal tidal breath, it amounts to about 150 ml.
- Functional volume. The functional volume, which is the air that actually reaches the respiratory zone and contributes to gas exchange, is about 350 ml.
- Spirometer. Respiratory capacities are measured with a spirometer, wherein as a person breathes, the volumes of air exhaled can be read on an indicator, which shows the changes in air volume inside the apparatus.
Respiratory Sounds
- Bronchial sounds. Bronchial sounds are produced by air rushing through the large respiratory passageways (trachea and bronchi).
- Vesicular breathing sounds. Vesicular breathing sounds occur as air fills the alveoli, and they are soft and resemble a muffled breeze.
External Respiration, Gas Transport, and Internal Respiration
- External respiration. External respiration or pulmonary gas exchange involves oxygen being loaded and carbon dioxide being unloaded from the blood.
- Internal respiration. In internal respiration or systemic capillary gas exchange, oxygen is unloaded and carbon dioxide is loaded into the blood.
- Gas transport. Oxygen is transported in the blood in two ways: most attaches to hemoglobin molecules inside the RBCs to form oxyhemoglobin, or a very small amount of oxygen is carried dissolved in the plasma; while carbon dioxide is transported in plasma as bicarbonate ion, or a smaller amount (between 20 to 30 percent of the transported carbon dioxide) is carried inside the RBCs bound to hemoglobin.
Control of Respiration
Neural Regulation
- Phrenic and intercostal nerves. These two nerves regulate the activity of the respiratory muscles, the diaphragm, and external intercostals.
- Medulla and pons. Neural centers that control respiratory rhythm and depth are located mainly in the medulla and pons; the medulla, which sets the basic rhythm of breathing, contains a pacemaker, or self-exciting inspiratory center, and an expiratory center that inhibits the pacemaker in a rhythmic way; pons centers appear to smooth out the basic rhythm of inspiration and expiration set by the medulla.
- Eupnea. The normal respiratory rate is referred to as eupnea, and it is maintained at a rate of 12 to 15 respirations/minute.
- Hyperpnea. During exercise, we breathe more vigorously and deeply because the brain centers send more impulses to the respiratory muscles, and this respiratory pattern is called hyperpnea.
Non-neural Factors Influencing Respiratory Rate and Depth
- Physical factors. Although the medulla’s respiratory centers set the basic rhythm of breathing, there is no question that physical factors such as talking, coughing, and exercising can modify both the rate and depth of breathing, as well as an increased body temperature, which increases the rate of breathing.
- Volition (conscious control). Voluntary control of breathing is limited, and the respiratory centers will simply ignore messages from the cortex (our wishes) when the oxygen supply in the blood is getting low or blood pH is falling.
- Emotional factors. Emotional factors also modify the rate and depth of breathing through reflexes initiated by emotional stimuli acting through centers in the hypothalamus.
- Chemical factors. The most important factors that modify respiratory rate and depth are chemical- the levels of carbon dioxide and oxygen in the blood; increased levels of carbon dioxide and decreased blood pH are the most important stimuli leading to an increase in the rate and depth of breathing, while a decrease in oxygen levels become important stimuli when the levels are dangerously low.
- Hyperventilation. Hyperventilation blows off more carbon dioxide and decreases the amount of carbonic acid, which returns blood pH to the normal range when carbon dioxide or other sources of acids begin to accumulate in the blood.
- Hypoventilation. Hypoventilation or extremely slow or shallow breathing allows carbon dioxide to accumulate in the blood and brings blood pH back into normal range when blood starts to become slightly alkaline.
Age-Related Physiological Changes in the Respiratory System
Respiratory efficiency is reduced with age. They are unable to compensate for increased oxygen need and are significantly increasing the amount of air inspired. Therefore, difficulty in breathing is usually common especially during activities. Expiratory muscles become weaker so their cough efficiency is reduced and the amount of air left in the lungs is increased. Health promotion teaching can include smoking cessation, preventing respiratory infections through handwashing, and ensuring up to date influenza and pneumonia vaccinations.
See also
Craving more insights? Dive into these related materials to enhance your study journey!
- Anatomy and Physiology Nursing Test Banks. This nursing test bank includes questions about Anatomy and Physiology and its related concepts such as: structure and functions of the human body, nursing care management of patients with conditions related to the different body systems.
Hello,
My name is Sharon and I think I just struck gold! This web site is just what I need to study, learn, and understand the Human Body. Thank you so much.
Thank you so much. you just made my day. The information was comprehensive and comes as an easy resource.
Violet.
Thanks very much, I was satisfied with the answers
Thanks very much. I am satisfied with the notes
Thank you so much the notes are perfect and useful to my studies
Very helpful and easy to understand. Thank you so much.
It is fantastic and very helpfull and thanks a lot
This is very helpful, thank you.
You’re welcome! Happy to hear that you found the respiratory system anatomy and physiology material helpful. If there’s anything more you’d like to dive into or any questions you have, feel free to reach out. Always here to help with your learning journey.
Thank you so much
Anatomy and physiology is a subject to learn the figure the rate of human body as well. Thanks