Welcome to the fascinating world of the Urinary System Anatomy and Physiology tailored for nurses. As the body’s vital system for filtering and expelling waste, understanding its intricate workings is crucial for every nurse. Dive in to explore its structures, functions, and importance in maintaining overall health, ensuring you’re equipped with comprehensive knowledge to provide the best patient care.
Functions of the Urinary System
The function of the kidneys are as follows:
- Filter. Every day, the kidneys filter gallons of fluid from the bloodstream.
- Waste processing. The kidneys then process this filtrate, allowing wastes and excess ions to leave the body in urine while returning needed substances to the blood in just the right proportions.
- Elimination. Although the lungs and the skin also play roles in excretion, the kidneys bear the major responsibility for eliminating nitrogenous wastes, toxins, and drugs from the body.
- Regulation. The kidneys also regulate the blood’s volume and chemical makeup so that the proper balance between water and salts and between acids and bases is maintained.
- Other regulatory functions. By producing the enzyme renin, they help regulate blood pressure, and their hormone erythropoietin stimulates red blood cell production in the bone marrow.
- Conversion. Kidney cells also convert vitamin D to its active form.
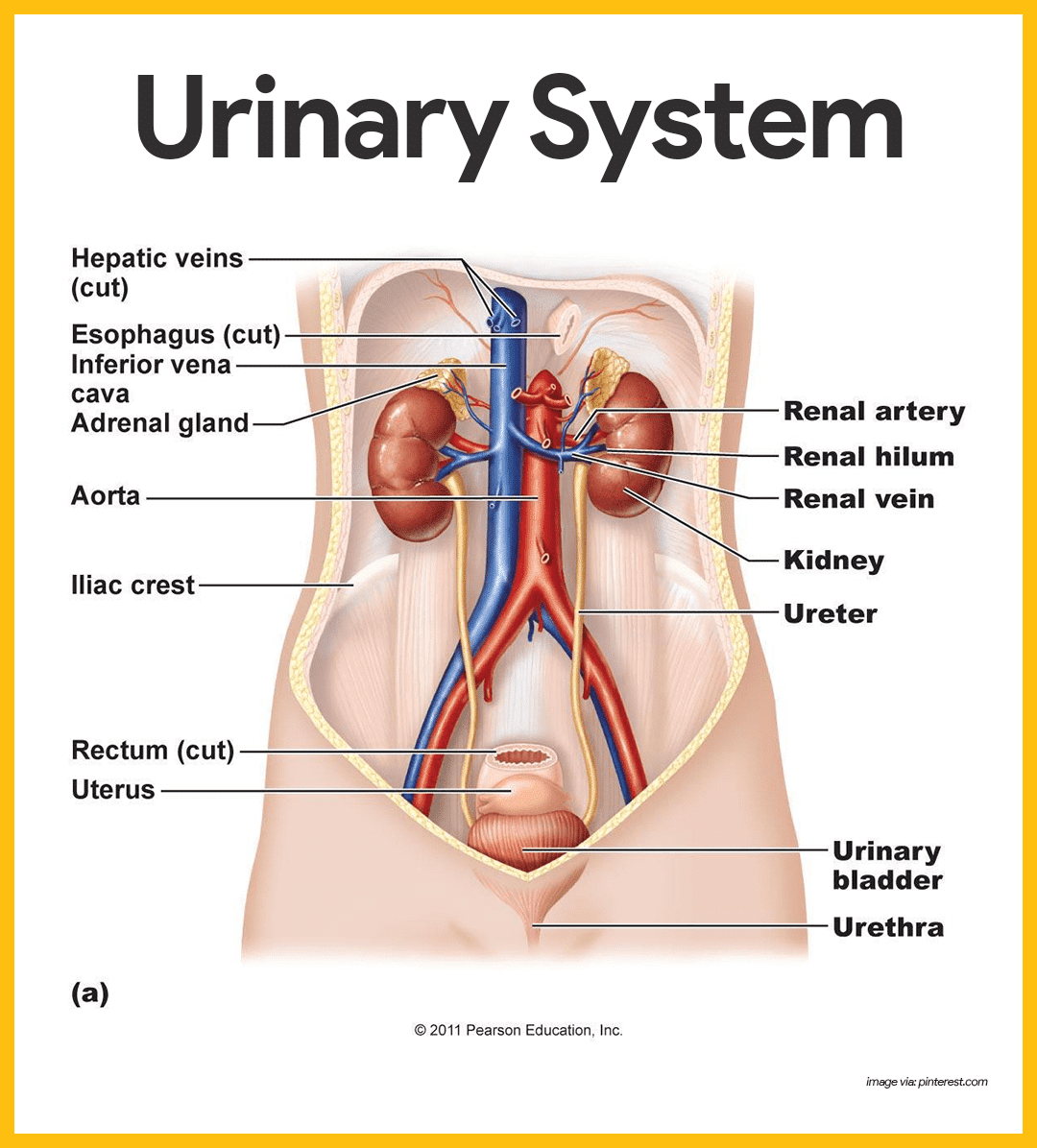
Anatomy of the Urinary System
The urinary system consists of two kidneys, two ureters, a urinary bladder, and a urethra. The kidneys alone perform the functions just described and manufacture urine in the process, while the other organs of the urinary system provide temporary storage reservoirs for urine or serve as transportation channels to carry it from one body region to another.
The Kidneys
The kidneys, which maintain the purity and constancy of our internal fluids, are perfect examples of homeostatic organs.
- Location. These small, dark red organs with a kidney-bean shape lie against the dorsal body wall in a retroperitoneal position (beneath the parietal peritoneum) in the superior lumbar region; they extend from the T12 to the L3 vertebra, thus they receive protection from the lower part of the rib cage.
- Positioning. Because it is crowded by the liver, the right kidney is positioned slightly lower than the left.
- Size. An adult kidney is about 12 cm (5 inches) long, 6 cm (2.5 inches) wide, and 3 cm (1 inch) thick, about the size of a large bar of soap.
- Adrenal gland. Atop each kidney is an adrenal gland, which is part of the endocrine system is a distinctly separate organ functionally.
- Fibrous capsule. A transparent fibrous capsule encloses each kidney and gives a fresh kidney a glistening appearance.
- Perirenal fat capsule. A fatty mass, the perirenal fat capsule, surrounds each kidney and acts to cushion it against blows.
- Renal fascia. The renal fascia, the outermost capsule, anchors the kidney and helps hold it in place against the muscles of the trunk wall.
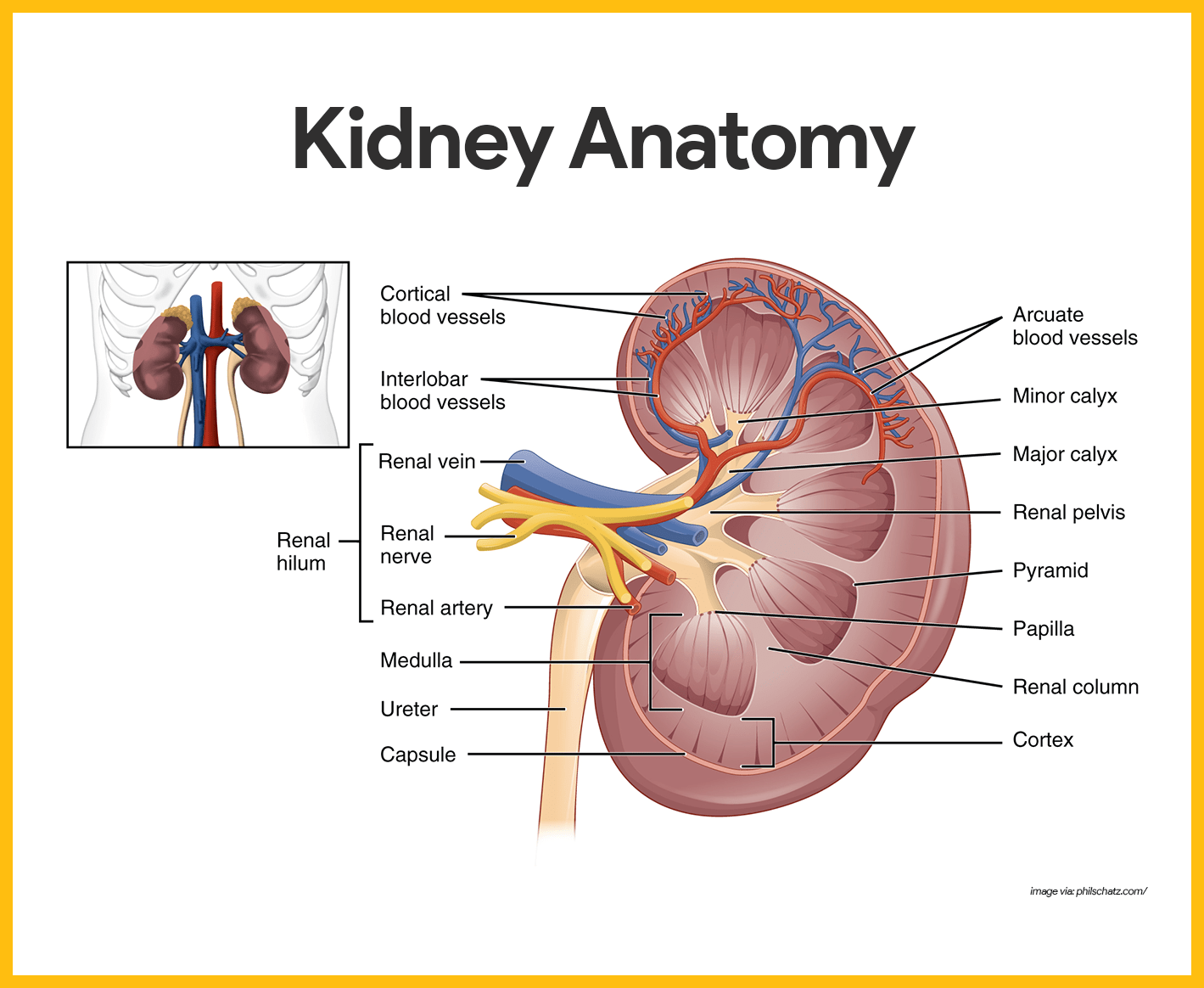
- Renal cortex. The outer region, which is light in color, is the renal cortex.
- Renal medulla. Deep to the cortex is a darker, reddish-brown area, the renal medulla.
- Renal pyramids. The medulla has many basically triangular regions with a striped appearance, the renal, or medullary pyramids; the broader base of each pyramid faces toward the cortex while its tip, the apex, points toward the inner region of the kidney.
- Renal columns. The pyramids are separated by extensions of cortex-like tissue, the renal columns.
- Renal pelvis. Medial to the hilum is a flat, basinlike cavity, the renal pelvis, which is continuous with the ureter leaving the hilum.
- Calyces. Extensions of the pelvis, calyces, form cup-shaped areas that enclose the tips of the pyramid and collect urine, which continuously drains from the tips of the pyramids into the renal pelvis.
- Renal artery. The arterial supply of each kidney is the renal artery, which divides into segmental arteries as it approaches the hilum, and each segmental artery gives off several branches called interlobar arteries.
- Arcuate arteries. At the cortex-medulla junction, interlobar arteries give off arcuate arteries, which curve over the medullary pyramids.
- Cortical radiate arteries. Small cortical radiate arteries then branch off the arcuate arteries and run outward to supply the cortical tissue.
Nephrons
Nephrons are the structural and functional units of the kidneys.
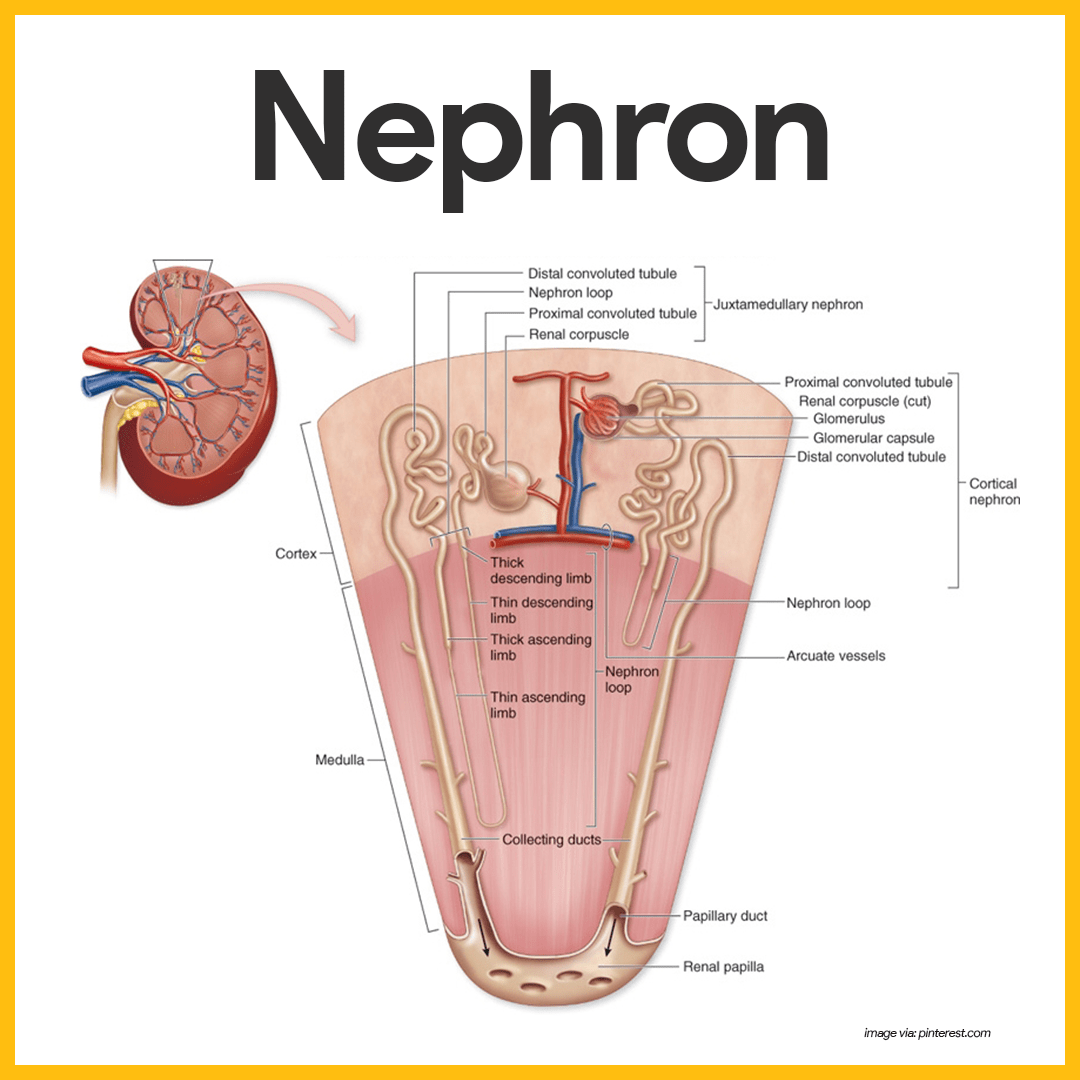
- Nephrons. Each kidney contains over a million tiny structures called nephrons, and they are responsible for forming urine.
- Glomerulus. One of the main structures of a nephron, a glomerulus is a knot of capillaries.
- Renal tubule. Another one of the main structures in a nephron is the renal tubule.
- Bowman’s capsule. The closed end of the renal tubule is enlarged and cup-shaped and completely surrounds the glomerulus, and it is called the glomerular or Bowman’s capsule.
- Podocytes. The inner layer of the capsule is made up of highly modified octopus-like cells called podocytes.
- Foot processes. Podocytes have long branching processes called foot processes that intertwine with one another and cling to the glomerulus.
- Collecting duct. As the tubule extends from the glomerular capsule, it coils and twists before forming a hairpin loop and then again becomes coiled and twisted before entering a collecting tubule called the collecting duct, which receives urine from many nephrons.
- Proximal convoluted tubule. This is the part of the tubule that is near to the glomerular capsule.
- Loop of Henle. The loop of Henle is the hairpin loop following the proximal convoluted tubule.
- Distal convoluted tubule. After the loop of Henle, the tubule continues to coil and twist before the collecting duct, and this part is called the distal convoluted tubule.
- Cortical nephrons. Most nephrons are called cortical nephrons because they are located almost entirely within the cortex.
- Juxtamedullary nephrons. In a few cases, the nephrons are called juxtamedullary nephrons because they are situated next to the cortex-medullary junction, and their loops of Henle dip deep into the medulla.
- Afferent arteriole. The afferent arteriole, which arises from a cortical radiate artery, is the “feeder vessel”.
- Efferent arteriole. The efferent arteriole receives blood that has passed through the glomerulus.
- Peritubular capillaries. They arise from the efferent arteriole that drains the glomerulus.
Ureters
The ureters do play an active role in urine transport.
- Size. The ureters are two slender tubes each 25 to 30 cm (10 to 12 inches) long and 6 mm (1/4 inch) in diameter.
- Location. Each ureter runs behind the peritoneum from the renal hilum to the posterior aspect of the bladder, which it enters at a slight angle.
- Function. Essentially, the ureters are passageways that carry urine from the kidneys to the bladder through contraction of the smooth muscle layers in their walls that propel urine into the bladder by peristalsis and is prevented from flowing back by small valve-like folds of bladder mucosa that flap over the ureter openings.
Urinary Bladder
The urinary bladder is a smooth, collapsible, muscular sac that stores urine temporarily.
- Location. It is located retroperitoneally in the pelvis just posterior to the symphysis pubis.
- Function. The detrusor muscles and the transitional epithelium both make the bladder uniquely suited for its function of urine storage.
- Trigone. The smooth triangular region of the bladder base outlined by these three openings is called the trigone, where infections tend to persist.
- Detrusor muscles. The bladder wall contains three layers of smooth muscle, collectively called the detrusor muscle, and its mucosa is a special type of epithelium, transitional epithelium.
Urethra
The urethra is a thin-walled tube that carries urine by peristalsis from the bladder to the outside of the body.
- Internal urethral sphincter. At the bladder-urethral junction, a thickening of the smooth muscle forms the internal urethral sphincter, an involuntary sphincter that keeps the urethra closed when the urine is not being passed.
- External urethral sphincter. A second sphincter, the external urethral sphincter, is fashioned by skeletal muscle as the urethra passes through the pelvic floor and is voluntarily controlled.
- Female urethra. The female urethra is about 3 to 4 cm (1 1/2 inches) long, and its external orifice, or opening, lies anteriorly to the vaginal opening.
- Male urethra. In me, the urethra is approximately 20 cm (8 inches) long and has three named regions: the prostatic, membranous, and spongy (penile) urethrae; it opens at the tip of the penis after traveling down its length.
Physiology of the Urinary System
Every day, the kidneys filter gallons of fluid from the bloodstream. The normal physiology that takes place in the urinary system is as follows:
Urine Formation
Urine formation is a result of three processes:
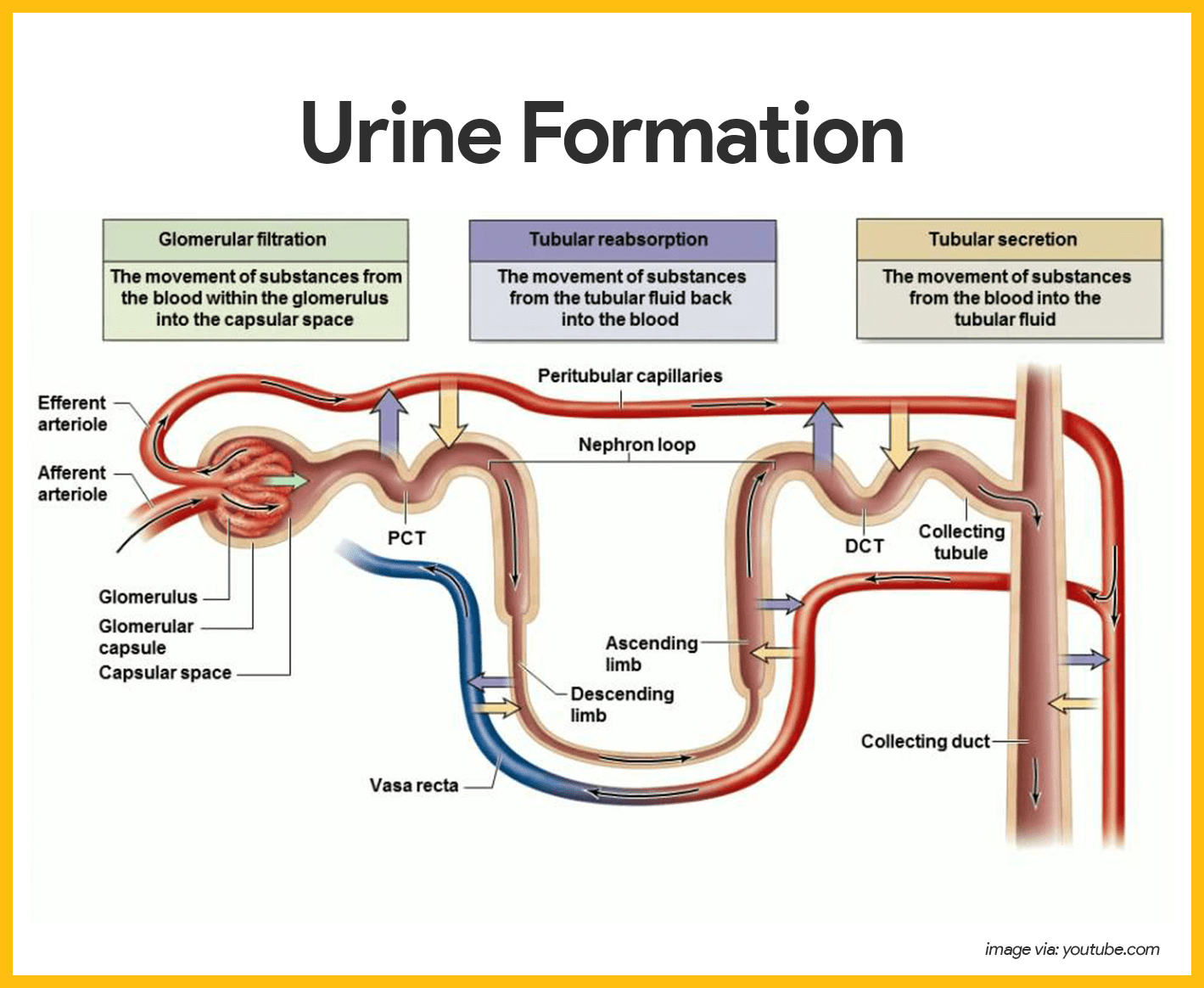
- Glomerular filtration. Water and solutes smaller than proteins are forced through the capillary walls and pores of the glomerular capsule into the renal tubule.
- Tubular reabsorption. Water, glucose, amino acids, and needed ions are transported out of the filtrate into the tubule cells and then enter the capillary blood.
- Tubular secretion. Hydrogen, potassium, creatinine, and drugs are removed from the peritubular blood and secreted by the tubule cells into the filtrate.
Characteristics of Urine
In 24 hours, the marvelously complex kidneys filter some 150 to 180 liters of blood plasma through their glomeruli into the tubules.
- Daily volume. In 24 hours, only about 1.0 to 1.8 liters of urine are produced.
- Components. Urine contains nitrogenous wastes and unneeded substances.
- Color. Freshly voided urine is generally clear and pale to deep yellow.
- Odor. When formed, urine is sterile and slightly aromatic, but if allowed to stand, it takes on an ammonia odor caused by the action of bacteria on the urine solutes.
- pH. Urine pH is usually slightly acidic (around 6), but changes in body metabolism and certain foods may cause it to be much more acidic or basic.
- Specific gravity. Whereas the specific gravity of pure water is 1.0, the specific gravity of urine usually ranges from 1.001 to 1.035.
- Solutes. Solutes normally found in urine include sodium and potassium ions, urea, uric acid, creatinine, ammonia, bicarbonate ions, and various other ions.
Micturition
Micturition or voiding is the act of emptying the bladder.
- Accumulation. Ordinarily, the bladder continues to collect urine until about 200 ml have accumulated.
- Activation. At about this point, stretching of the bladder wall activates stretch receptors.
- Transmission. Impulses transmitted to the sacral region of the spinal cord and then back to the bladder via the pelvic splanchnic nerves cause the bladder to go into reflex contractions.
- Passage. As the contractions become stronger, stored urine is forced past the internal urethral sphincter into the upper part of the urethra.
- External sphincter. Because the lower external sphincter is skeletal muscle and voluntarily controlled, we can choose to keep it closed or it can be relaxed so that urine is flushed from the body.
Age-Related Physiological Changes in the Urinary System
The function of the kidney decreases with age but is still able to carry out excretory functions unless a disease process intervenes. Waste products may be filtered and excreted more slowly. Therefore, nurses must include in their responsibility the effect of drugs that older people take to their kidneys.
Aside from the kidneys, the bladder makes more noticeable changes. Complaints of urinary urgency and frequency are common because the capacity of the bladder and its ability to completely empty diminish with age. It is important to note that urinary incontinence (UI) is never normal so the nurse must promptly investigate it, particularly when of new onset.
Good urinary function in older people can be promoted by sufficient fluid intake, reducing bladder-irritant foods in the diet (e.g. sugar, caffeine, spicy and acidic foods), and practicing pelvic muscle exercises.
See also
Don’t miss out! Dive deeper into the urinary system with these must-read posts:
- Anatomy and Physiology Nursing Test Banks
Unlock success in your nursing journey! Dive deep into the intricacies of the human body with our comprehensive Anatomy and Physiology Nursing Test Banks. Tailored for aspiring health professionals, these test banks are your key to mastering the core concepts. Don’t miss out—elevate your understanding and confidence today! - Urinary Disorders NCLEX Practice Quiz (150 Questions)
Boost your NCLEX prep! Tackle our 150-question Urinary Disorders Practice Quiz and step confidently into exam day. Sharpen your knowledge now!
Other posts you may also like:










Leave a Comment