The Nurse Licensure Compact (NLC) is an agreement that allows nurses to hold one multi-state license and practice in any participating compact state without obtaining separate licenses for each state. In other words, a nurse’s license issued in their home state (primary state of residence) can grant privilege to practice in dozens of other states under the NLC.
This guide provides a detailed, up-to-date overview of the NLC for nursing professionals. We’ll explore the history and evolution of the compact (from the original NLC to the enhanced eNLC), explain how it works and how to get a multistate license, clarify rules for moving between states, and discuss the compact’s impact on nursing shortages, telehealth, and travel nursing. We’ll also give the latest status of state participation (as of 2024–2025) and explain the separate APRN Compact for advanced practice nurses. Finally, we offer tips for nurses who want to support compact legislation in their own states.
What is the Nurse Licensure Compact (NLC)?
The Nurse Licensure Compact (NLC) is an interstate agreement that permits registered nurses (RNs) and licensed practical/vocational nurses (LPN/VNs) to practice in all member states with one multistate license. Under the compact, a nurse’s license issued by their home state (state of primary residence) is recognized by every other compact state, allowing seamless practice across state lines. If a nurse wants to practice (in person or via telehealth) in another compact state, they do not need to apply for a separate license or pay additional fees for that state. This flexibility benefits nurses who travel, work telehealth or remote positions, or live near state borders. It also benefits employers and patients by improving access to nursing care, especially in underserved areas.
Importantly, the NLC applies only to RNs and LPN/LVNs. It does not automatically cover Advanced Practice Registered Nurses (APRNs) like nurse practitioners – the APRN Compact is a separate agreement discussed later. Every state still retains the authority to regulate nursing practice within its borders, meaning nurses must adhere to each state’s nursing laws and rules when practicing there (for example, scope of practice or specific regulations) even if they are practicing on a multistate license. The NLC increases mobility while maintaining public protection: all compact nurses must meet a set of uniform requirements (including background checks), and states share disciplinary and investigatory information to ensure patient safety.
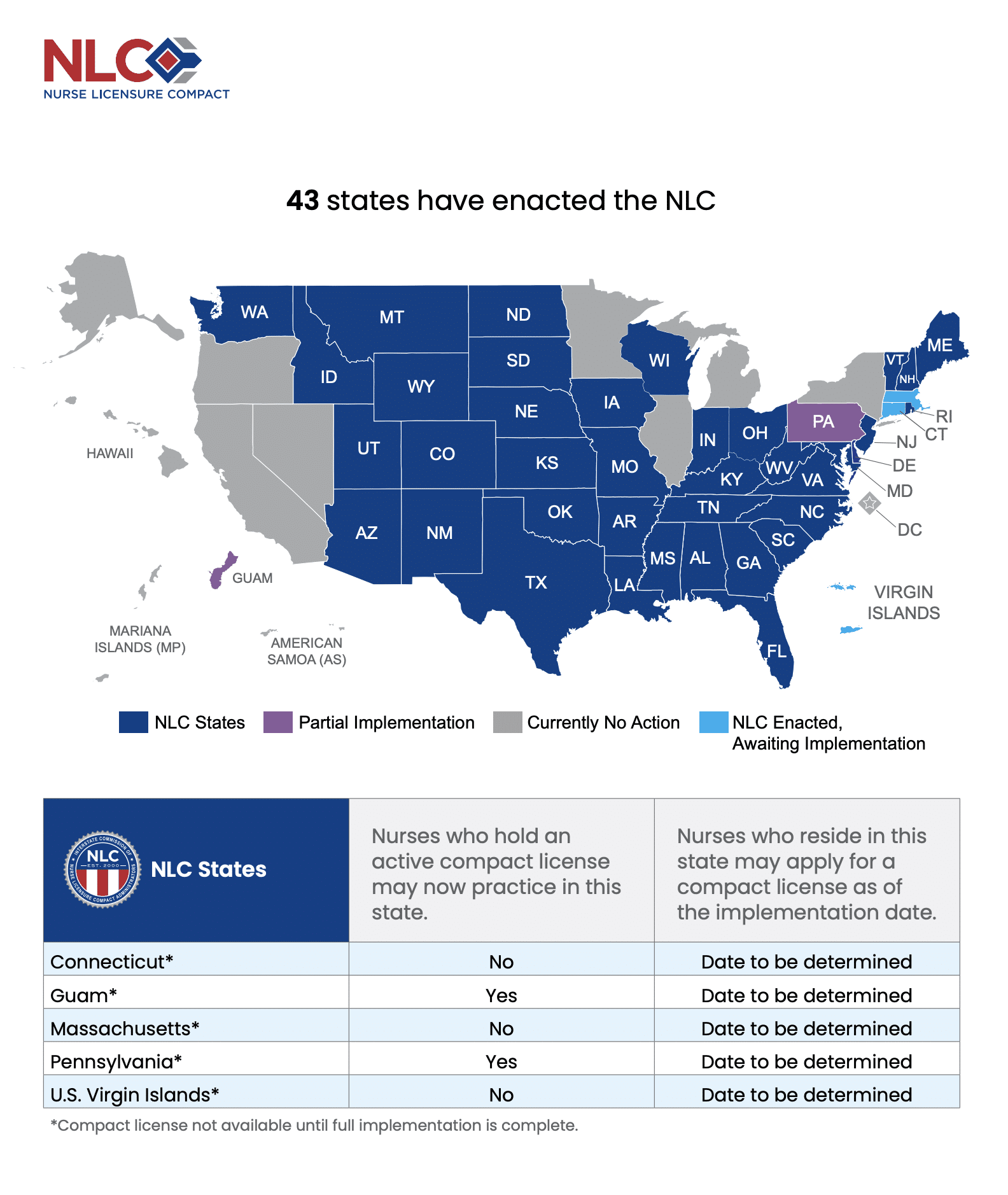
Today the NLC has become widely adopted. As of early 2025, 43 U.S. jurisdictions (including states and territories) have enacted the compact. In practical terms, this means the vast majority of states are either already compact members or in the process of implementing the NLC. Nurses living in those states can potentially practice in a broad multi-state region (currently spanning dozens of states) on a single license. By contrast, the few states that are not in the compact still require nurses to obtain a separate license to practice there. In the sections below, we’ll delve into the evolution of the compact, how to obtain a multistate license, and what happens if you move or practice across states.
History and Evolution: From Original NLC to eNLC
The concept of mutual recognition for nurse licensure isn’t brand new – it has been developing for over two decades. The original Nurse Licensure Compact was launched in 2000, when a handful of pioneer states (Maryland, Texas, Utah, and Wisconsin) enacted the compact into law. In the early 2000s, up to 25 states joined that first version of the NLC. This allowed many nurses to start practicing across state lines more easily. However, not all states were eager to join initially. There were concerns from some nurses and associations about differences in licensing standards and the absence of certain safeguards (such as universal background checks). As a result, after the initial wave, membership growth plateaued and several states remained outside the compact.
To address these concerns, the enhanced Nurse Licensure Compact (eNLC) was developed. In 2015, the National Council of State Boards of Nursing (NCSBN) and state boards drafted a modernized compact with stronger uniform requirements. This “enhanced” compact introduced key improvements: all participating states agreed to a set of Uniform Licensure Requirements (ULRs), including mandatory federal fingerprint-based criminal background checks and uniform eligibility standards for license applicants. It also formalized information-sharing and disciplinary actions across state lines to improve public safety. Essentially, the eNLC ensured that every compact state upholds the same baseline licensure criteria, addressing earlier criticisms about inconsistent standards.
By mid-2017, enough states had enacted the new eNLC for it to launch. The eNLC was officially implemented on January 19, 2018, replacing the old compact. Nurses with existing multistate licenses from the old compact were grandfathered in (except in states that chose not to join the new compact). A few states that had been in the original NLC needed to pass new legislation to join the eNLC. For example, Rhode Island had been part of the original compact but did not immediately join the enhanced version; it later re-joined in 2023 after passing updated legislation. Since 2018, the enhanced NLC (often just called “the NLC” now) has continued to grow steadily each year as more states adopt it.
In the years following eNLC implementation, dozens of states enacted the compact. By 2021, about 34–35 states were members, including almost all of the South and Midwest. On the NLC’s 20th anniversary (2020), the momentum was still building. Notably, in 2021 the NLC saw big holdouts like New Jersey and Ohio enact compact legislation (Ohio’s NLC became effective in 2023). Two U.S. territories, Guam and the U.S. Virgin Islands, also enacted the compact in 2021, extending multistate privileges to those jurisdictions (though they have faced some implementation delays). In 2023 and 2024, even more states joined: Washington State enacted the NLC in April 2023 (40th jurisdiction), Rhode Island re-enacted it in June 2023 (41st), Connecticut signed on in May 2024 (42nd), and Massachusetts passed the NLC in November 2024, becoming the 43rd member state. This trajectory underscores a broad trend toward licensure portability – by the NLC’s 25th anniversary in 2025, nearly all U.S. states had at least considered joining.
Despite this growth, a few large states remain outside the compact as of 2025. California and New York, for instance, have long resisted the NLC, largely due to stakeholder concerns (we’ll discuss those in a later section). Other non-compact states include Alaska, Illinois, Hawaii, Michigan, Minnesota, Nevada, Oregon, and the District of Columbia, though many of these have seen bills introduced and active debates about joining. In fact, by late 2024, almost every state except Nevada and Oregon had either joined or had pending NLC legislation in their legislature. The overall trend is clear: the NLC has evolved from a small coalition in 2000 to a near-national system in 2025, as states respond to an increasingly mobile nursing workforce and the need for flexible healthcare delivery.
How the NLC Works: Key Principles and Requirements
Under the NLC, a nurse holds one active license in their primary state of residence (PSOR), but gains a “multistate privilege” to practice in all other compact member states. Let’s break down how this works and what is required:
Primary State of Residence (PSOR)
Your PSOR is basically your home state – where you live and legally reside (typically evidenced by your driver’s license, voter registration, etc.). You can only hold a multistate license in your primary state of residence. For example, if you live in Texas (a compact state), the Texas Board of Nursing can issue you a multistate license. That license allows practice in all other compact states. You cannot hold two multistate licenses at the same time. If you move and change your primary residence to a different compact state, you’ll need to transfer your license to the new state (details on moving are in the next section).
Uniform Licensure Requirements (ULRs)
To get a multistate license, a nurse must meet the NLC’s uniform requirements, which help ensure all nurses practicing under compact privilege meet high standards. These requirements include holding an unencumbered active RN or LPN license (no active discipline) in your home state, graduating from an approved nursing program, passing the NCLEX–RN or NCLEX-PN exam, undergoing an FBI fingerprint criminal background check, and meeting any applicable state requirements such as English proficiency for international graduates. The background check and other criteria became mandatory with the enhanced compact to promote patient safety and trust between states. If a nurse does not meet the multistate license criteria (for example, due to a past felony conviction or not meeting the ULR standards), they may still be eligible for a single-state license in that state, but not a multistate license.
Applying for a Multistate License
Nurses apply for licensure through their state Board of Nursing as usual. If your state is a compact member and you meet all the ULR, you can apply for a multistate license (often this is part of the initial exam application or by endorsement if you’re moving in). For instance, a new graduate in Florida (compact state) who meets the criteria will be issued a multistate RN license by Florida. An experienced nurse relocating to Florida from a non-compact state would apply by license endorsement and, upon meeting the requirements (including the background check), Florida can issue a multistate license. State boards typically have a checkbox or separate application for obtaining the multistate privilege when eligible. If you’re already licensed in a compact state but aren’t sure if your license is multistate, you can verify your license status via the Nursys database, which will indicate if it’s multistate or single-state.
Practice Privileges Across States
Once you have a multistate license, you can practice in any other NLC member state without further paperwork. “Practice” includes not only physically working in that state, but also providing telehealth nursing care remotely to patients located in other compact states. For example, a telephonic triage nurse in Arizona can counsel a patient in Colorado under the compact privilege, and a travel nurse with a Texas multistate license can take an assignment in Ohio without applying for an Ohio license. If you want to work in a non-compact state, however, you must obtain a license for that state by the traditional process – the compact does not cover non-member states.
State Laws and Disciplinary Authority
When practicing in a remote state (not your home state) under a compact privilege, you must follow the nurse practice act and regulations of that state. The remote state has the authority to regulate your practice within its borders. For example, if a nurse with a multistate license from North Carolina is working in Missouri, Missouri’s scope of practice rules and standards apply to that nurse’s practice there. If a potential violation or complaint arises, the remote state can take action on the nurse’s privilege to practice in that state (such as suspending the privilege or disciplining the nurse for violations of that state’s laws).
Serious disciplinary actions are communicated through the compact mechanism: a significant action against a multistate license (like a suspension or revocation by the home state) will automatically affect the nurse’s ability to practice in all compact states. In short, all the member boards of nursing coordinate to ensure public protection, sharing investigatory information and upholding any sanctions across state lines. This cooperative regulation is a cornerstone of the NLC.
NLC and Nurse Educators
It’s worth noting that the NLC benefits not only bedside nurses but also nurse educators and faculty who teach across state lines. Many nursing programs (especially online programs) have students located in multiple states. Most states require faculty to be licensed in the state where students are located. A multistate license allows a nurse educator to teach students in any compact state without needing multiple licenses. Similarly, a nurse in a compact state can serve as a preceptor for a student from another compact state or provide consulting services remotely without extra licenses.

The NLC framework significantly streamlines licensure for nurses and removes redundant bureaucracy. It’s often compared to a driver’s license model – your state driver’s license lets you drive in any other state, but you must obey the local traffic laws. Likewise, your multistate nursing license lets you practice in other member states, while you follow each state’s nursing laws. For nurses, this means less paperwork and cost when taking jobs in new states or engaging in telehealth. For employers and healthcare systems, it means they can more quickly recruit qualified nurses from out of state when needed. And for patients, it increases the availability of nurses, whether locally or via telehealth, especially in times of high demand or disaster response.
Compact vs. Non-Compact States: Where Can You Practice?
One of the most common questions about the NLC is, “Which states are in the compact?” and conversely, which are not. As of 2025, the majority of states are compact members. To put it in numbers, 43 states and U.S. territories have enacted the NLC, though not all are fully implemented yet. In practice, about 38-40 states are actively issuing multistate licenses or recognizing them, with a few having passed laws that are pending implementation.
You may also access their Nurse Licensure Guidance tool to help you learn where you can practice based on where you live or plan to live.
Current List and Status of Each State
For a current list, it’s always best to check the official NCSBN compact map or resources like NurseCompact.com, but here is an overview:
| State / Territory | NLC Status (May 2025) |
|---|---|
| Alabama | Member – Implemented |
| Alaska | Legislation Pending – HB 131 / SB 124 (2025) |
| Arizona | Member – Implemented |
| Arkansas | Member – Implemented |
| California | No Action (prior bill AB 3232 died 2024) |
| Colorado | Member – Implemented |
| Connecticut | Enacted; takes effect Oct 1 2025 |
| Delaware | Member – Implemented |
| Florida | Member – Implemented |
| Georgia | Member – Implemented |
| Hawaii | Legislation Pending – HB 897 (2025) |
| Idaho | Member – Implemented |
| Illinois | Legislation Pending – HB 1706 (2025) |
| Indiana | Member – Implemented |
| Iowa | Member – Implemented |
| Kansas | Member – Implemented |
| Kentucky | Member – Implemented |
| Louisiana | Member – Implemented |
| Maine | Member – Implemented |
| Maryland | Member – Implemented |
| Massachusetts | Enacted Nov 20 2024; implementation in progress |
| Michigan | Legislation Pending – HB 4246 (2025) |
| Minnesota | Legislation Pending – HF 1925 / SF 2608 (2025) |
| Mississippi | Member – Implemented |
| Missouri | Member – Implemented |
| Montana | Member – Implemented |
| Nebraska | Member – Implemented |
| Nevada | Legislation Pending – SB 34 (2025) |
| New Hampshire | Member – Implemented |
| New Jersey | Member – Implemented |
| New Mexico | Member – Implemented |
| New York | Legislation Pending – SB 3916 / AB 3007 (2025) |
| North Carolina | Member – Implemented |
| North Dakota | Member – Implemented |
| Ohio | Member – Implemented |
| Oklahoma | Member – Implemented |
| Oregon | Legislation Pending – SB 966 (2025) |
| Pennsylvania | Partial Implementation – visiting multistate nurses allowed (since Sept 5 2023) |
| Rhode Island | Member – Implemented (re-joined Jan 1 2024) |
| South Carolina | Member – Implemented |
| South Dakota | Member – Implemented |
| Tennessee | Member – Implemented |
| Texas | Member – Implemented |
| Utah | Member – Implemented |
| Vermont | Member – Implemented (since Feb 1 2022) |
| Virginia | Member – Implemented |
| Washington | Member – Implemented (home-state issuance July 2024) |
| West Virginia | Member – Implemented |
| Wisconsin | Member – Implemented |
| Wyoming | Member – Implemented |
| District of Columbia | Legislation Pending – Council Bill 26-0069 (2025) |
| American Samoa | No Action |
| Guam | Partial Implementation – visiting multistate nurses allowed |
| Northern Mariana Islands | No Action |
| Puerto Rico | Not Eligible (associate NCSBN member) |
| U.S. Virgin Islands | Enacted Dec 6 2021; implementation pending |
Compact Member States (Active)
These include almost all of the South (e.g. Texas, Florida, Georgia, Tennessee, both Carolinas, etc.), most of the Midwest (e.g. Ohio, Indiana, Missouri, Iowa, Kansas, etc.), and a growing number of Western and New England states (e.g. Arizona, Idaho, Utah, Colorado, Montana, New Hampshire, Maine). Notably, states like Washington, Oregon’s neighbor Idaho, and Pennsylvania (pending implementation) are members or soon to be.
By January 2024, there were 37 states fully implementing the NLC, and that number has continued to climb with Connecticut and Massachusetts joining in 2024. Some states have partial or delayed implementations: for example, Washington State joined in mid-2023 and began recognizing multistate licenses from elsewhere that year, but only started issuing its own multistate licenses to Washington nurses in 2024. Rhode Island rejoined the compact effective January 1, 2024. Pennsylvania enacted the NLC back in 2021 but, due to administrative delays, has not yet implemented it as of 2024; it is expected to go live once systems are in place. Guam (a U.S. territory) enacted the NLC but has “partial implementation” status, likely pending full integration of the required systems. The U.S. Virgin Islands also enacted it and is awaiting implementation. These nuances mean that a few places have passed the compact but nurses can’t get a multistate license there quite yet. Always double-check if a state is “compact in effect” or just “compact enacted, pending” if you plan to work there soon.
Below is an at-a-glance snapshot of every U.S. state + the District of Columbia and the five U.S. territories, showing exactly where each jurisdiction stands in the Nurse Licensure Compact (NLC) as of May 27 2025. The NLC has reached 38 fully-operational member states; three more states and two territories have enacted—but not finished implementing—the pact; two jurisdictions (Pennsylvania and Guam) are in a hybrid “partial-implementation” phase; another nine states and D.C. have active bills; and only California plus two Pacific territories (American Samoa and the Commonwealth of the Northern Mariana Islands) have taken no legislative action so far. (Vivian Health, Vivian Health)
States Pending Legislation
Several states that were historically non-compact have shown movement by introducing bills. According to recent data, states with active or pending NLC legislation include Alaska, California, Hawaii, Illinois, Massachusetts, Michigan, Minnesota, New York, and Washington D.C.. (Massachusetts, of course, passed its legislation in late 2024 and is now working on implementation.) “Pending” means a bill has been proposed or is being debated, but not yet signed into law. For example, Illinois saw an NLC bill introduced in 2023, though it hadn’t passed as of the last update. Alaska’s Board of Nursing has been studying the compact and providing information to legislators, and bills have been discussed. New York had legislative proposals as well, especially after witnessing many nurses leave for travel assignments elsewhere during COVID-19, but it faces opposition from certain unions. California saw a bill (AB 3232) introduced in 2022–2023 to join the compact, but it did not advance; the debate there continues, largely centered on labor unions’ concerns and potential impacts on state-specific nursing regulations. Hawaii and Michigan have also had bills introduced in recent sessions. The District of Columbia (D.C.) has a council bill under consideration to join the NLC.
States Not in the Compact (No Current Action)
As of the latest data, only Nevada and Oregon had neither joined nor had active legislation in play. These two states thus remain completely outside the compact with no immediate plans to join. If you plan to practice in Nevada or Oregon, you must go through their standard licensing process. In all other states, either the compact is already in effect or there’s ongoing discussion about it.
For nurses, the practical difference between compact vs non-compact states is huge. If you live in or hold a license from a compact state, you have tremendous flexibility to take jobs or assignments in other compact states without delay. If you live in a non-compact state (or plan to work in one), you’ll need to budget time and money for additional state licenses. Many travel nurses, for instance, try to maintain a compact license as their home license (for broad coverage) and then perhaps a couple of single-state licenses for key non-compact states they want to work in (like maintaining a CA or NY license).
It’s also worth mentioning that even within compact states, not everyone automatically has a multistate license. If a nurse didn’t opt in or provide fingerprints when their state joined the NLC, they might still only have a single-state license until they take action. For example, when New Jersey implemented the compact in 2021, nurses who wanted multistate privileges had to undergo a background check and upgrade their license. So, just being in a compact state doesn’t magically make your license multistate – you have to meet the requirements and likely apply or opt in through the state board. New grads in those states, however, will get the multistate if eligible from the start.
In summary, compact states offer a driver’s-license-style reciprocity for nursing, whereas non-compact states require the traditional approach of applying to each state where you wish to work. The landscape has been rapidly shifting in favor of the compact, and nurses should keep an eye on legislative changes. It’s quite possible that in a few more years, nearly all states will have joined, given the trends.
Obtaining and Maintaining a Multistate License
If you reside in a compact state, obtaining a multistate license is usually part of the normal licensure or endorsement process, with a few additional steps (mostly the background check). Here’s a step-by-step overview for different scenarios:
New Graduates in a Compact State
When you graduate from a nursing program and apply for your RN or LPN license in a compact state, you will typically be given the option of a multistate license. Ensure you complete the fingerprinting and background check as required. If you meet all eligibility criteria (see the ULRs above) and your state is issuing multistate licenses, you should receive a license with multistate status. This will be indicated on your license card or the online registry. From day one, that license is valid in all other compact states. Just remember that if you ever move to another state, you may need to transfer it (more on that below).
Existing Licensed Nurses (License by Endorsement)
If you are already an RN/LPN in one state and want to obtain a license in another state, you’ll use the endorsement process.
The steps differ depending on whether you are moving from a non-compact state or a compact state:
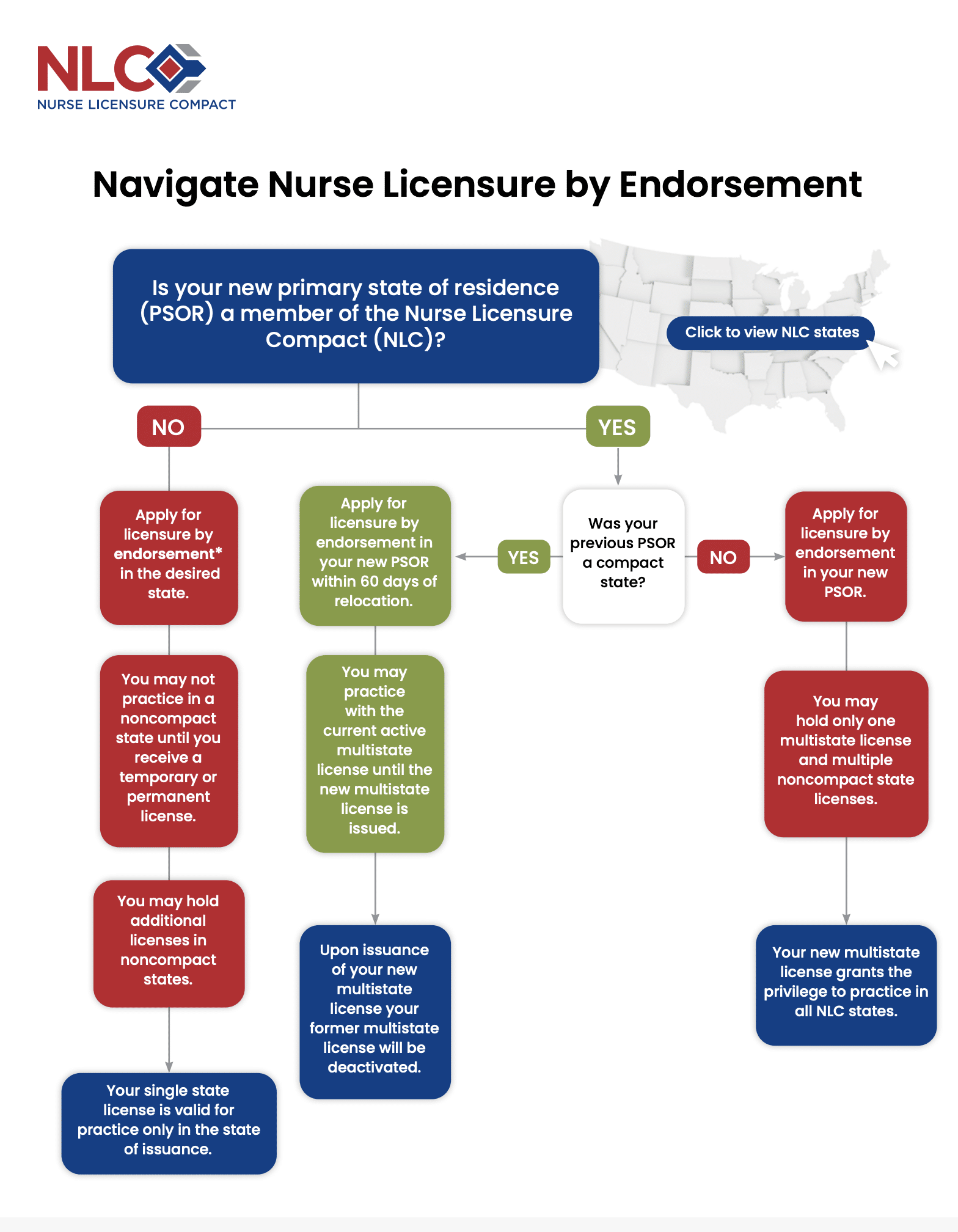
Moving from a Non-Compact State into a Compact State
Suppose you live in a non-compact state (say, California) and get a job in a compact state (say, Colorado). You’ll need to apply for licensure by endorsement in Colorado. You can usually start this process before or immediately after you move. Colorado will require you to meet the multistate license criteria (including that you declare Colorado as your new primary state residence and complete the background check). Once you receive your Colorado multistate license, you can use it to work not just in Colorado but in any NLC state.
Keep in mind, your California license remains valid only for California; it does not turn into a multistate license because California isn’t in the compact. In fact, many nurses coming from non-compact states are excited to get their first multistate license when moving into a compact state.
Moving from a Compact State to a Non-Compact State
If you move from a compact member state to a state that is not in the NLC, you will have to apply for a license in the new state (by endorsement) just as you would for any single-state license. For example, a nurse with a Texas multistate license who relocates to California must apply for a California RN license. Here’s a crucial point: once you change your primary residence to a non-compact state, your multistate license essentially loses its multistate status. It “reverts” to a single-state license valid only in the former home state. In the example, once the nurse becomes a California resident, their Texas multistate license can no longer be used to practice in other states (because the NLC requires your home to be in a member state). It’s wise to keep the old license active if you plan to return or use it in that state, but it won’t confer any multi-state privilege while you reside in a non-compact state.
Moving from one Compact State to another Compact State
If you’re relocating from one NLC state to a different NLC state, you will transfer your multistate license to the new state’s jurisdiction. The process again involves applying for licensure by endorsement in the new state and declaring it as your primary residence. The good news is you don’t have to maintain multiple licenses – once you get the new multistate license, it will cover you in all compact states (just like the old one did).
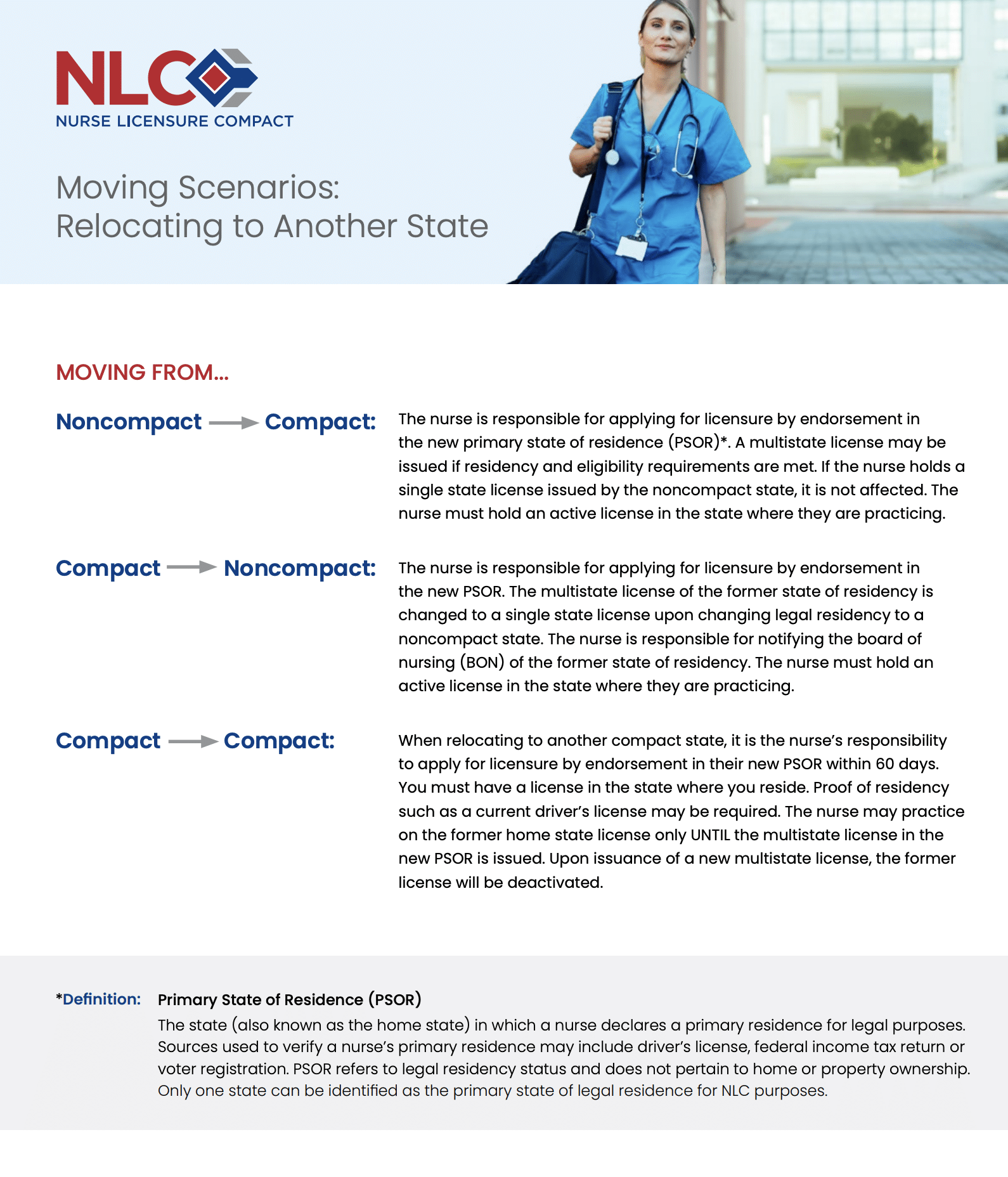
The timing is important: As of 2024, a new NLC rule requires that when you move to a new compact state, you must apply for licensure in that state within 60 days of moving. You are allowed to practice on your former home state license for a limited time (up to 60 days, effectively) while your new license is being processed, but you shouldn’t delay. Under this rule (effective Jan 2, 2024), once 60 days have passed, you would be out of compliance if you haven’t obtained the new state license. In practice, it’s best to apply as soon as you move (or even slightly before, if the state allows). Once your new multistate license is issued, your old one will be inactivated – you’ll then exclusively hold the license from your new home state (and again have multistate privileges everywhere). This 60-day rule was added to clarify expectations and ensure that nurses properly transfer their license when relocating, preventing a scenario where someone indefinitely works in a new state on an old license without ever transferring their home state designation.
Maintaining Your Multistate License
From a day-to-day perspective, maintaining a multistate license is not much different than maintaining a single-state license. You must renew it periodically (typically every 2 years, depending on state), complete any required continuing education for your home state, and of course, remain in good standing (no serious discipline).
If your license becomes encumbered (suspended, restricted, or otherwise disciplined) in your home state, your multistate privileges will likely be limited or paused in other states as well until the issue is resolved, as all member states honor those encumbrances. Another consideration is if you change your primary residence: always update your address with your state board. If you move to another compact state, you’ll need to transfer as described. If you move to a non-compact state, you should inform your board – you may end up needing to change that multistate license to a single-state license (some boards will do this automatically when they get wind of the address change). Also, keep an eye on communications from your board of nursing, especially if your state newly joins the NLC; there may be steps you need to take. For example, when states like Pennsylvania or Massachusetts enact the compact and implement it, their boards may ask existing nurses to opt in or provide proof of meeting requirements to obtain multistate privileges once available.
Working in Multiple States Frequently
If you regularly practice in several states (for instance, you’re a travel nurse rotating through different hospitals nationwide), a multistate license greatly simplifies your life. You won’t need to juggle separate renewal dates and fees for each state’s license. However, remember to follow each state’s scope of practice and rules where you are working. Also, if you maintain any separate single-state licenses for non-compact states (say you keep a New York license for assignments there), you’ll need to renew those and fulfill their CE requirements separately. The NLC doesn’t merge those, so some multi-state travelers still manage a couple of licenses: one multistate license covering the majority of states, and one or two single-state licenses for any holdout states they frequent.
Check Nursys
If you’re unsure about your current license status, use the Nursys online verification system (provided by NCSBN). It will display whether your license is single-state or multistate. If you only have a single-state license but your state is in the compact and you think you qualify, you can usually apply for an “upgrade” to multistate through your board (often this involves submitting fingerprints and paying a fee for the background check if not already done). Many boards have a specific application for current licensees to obtain multistate privileges now that the state is part of the NLC.
Changing States of Residence: Navigating a Move as a Compact Nurse
Changing your primary state of residence is one of the most important scenarios to understand under the NLC. We touched on it above, but here we’ll clearly spell out what a nurse should do in different moving situations:
Scenario 1: Non-Compact State → Compact State.
Example: You live in Oregon (not a compact state) and are moving to Idaho (compact state).
What to do: Apply for an Idaho nursing license by endorsement. You can initiate the application before your move or after; Idaho may issue a temporary permit if needed while paperwork is in process. Once you prove Idaho is now your primary residence and you meet all NLC requirements, the Idaho Board will issue you a multistate license. At that point, you can let your Oregon license lapse at the next expiration (unless you plan to return or keep it active as a single-state license for Oregon specifically). With your new Idaho multistate license, you are free to work in any of the compact states (currently 40+ jurisdictions). This is a big change if you were used to Oregon’s single-state license – it opens up a lot of mobility.
Scenario 2: Compact State → Non-Compact State.
Example: You live in Missouri (compact state, multistate license) and take a new job in California (non-compact).
What to do: Apply for a California RN license by endorsement (since CA isn’t in the NLC, no multistate aspect there). You might apply as soon as you accept the job, as California’s process can take some time. You could technically begin working on your Missouri license if you haven’t established California residency yet – but note that legally, once you’ve moved your permanent home to California, your multistate privilege for other states ends. Essentially, the moment you become a CA resident, your Missouri license acts like a Missouri-only license. You cannot practice in California on your Missouri license (because CA isn’t a party to the compact), and you also shouldn’t continue practicing in other compact states as a CA resident unless you maintain a residence back in a compact state. In other words, after moving, quickly obtain the California license and understand that your multistate is no longer in effect since your home is now non-compact. Many nurses maintain their previous compact license as a single-state license (e.g., keep it active in Missouri) in case they return or do telehealth for patients in that state, but again, it grants no multi-state privileges while your domicile is in California.
Scenario 3: Compact State → Compact State.
Example: You move from Georgia (compact state) to North Carolina (compact state).
What to do: This is where the new 60-day rule (2024) comes into play. You must apply for a North Carolina license by endorsement and designate NC as your primary state. Under the updated NLC rules, you should do this within 60 days of moving. Practically, you can continue working under your Georgia multistate license for up to 60 days after you become an NC resident. North Carolina will process your application and, once they issue your new license, your Georgia license’s multistate status will be turned off (Georgia will inactivate it, though you might be allowed to keep a Georgia single-state license if you still need one for some reason). If for some reason your new license is delayed, you might be in a gray area after 60 days, so it’s best not to push the time limit. This new rule ensures that everyone updates their licensure promptly when relocating. It also helps boards keep track of where nurses are residing and ensures background checks are up to date in the new state. Prior to this rule, a nurse could theoretically live in a new state and work on the old license for some time; now there’s a clearer expectation and timeline to transfer. Bottom line: start the endorsement as soon as you move (or slightly before, if allowed), and you’ll likely have the new license well within 60 days.
Scenario 4: Military Spouses and Others with Temporary Moves.
Special consideration is given to military families. If you’re the spouse of an active-duty military member and you move due to orders to a new state, the NLC is extremely helpful. You can start working immediately in the new state on your existing multistate license while you transition. You’ll still need to get the new state’s license if the new state is compact (since your residence changed), but military spouses are often familiar with frequent moves and the compact saves a lot of hassle of relicensing from scratch for every relocation. Many states expedite military spouse licensure anyway, but the NLC adds even more convenience. If the new state is non-compact, unfortunately you’ll have to go through that state’s process, but many states have laws to fast-track military spouse licensing.
In all cases of moving, it’s wise to check the Board of Nursing website of your new state for any guidance on NLC transfers. Some states might have a specific link or form for “Moving to our state with a multistate license? Here’s what to do.” Typically, it mirrors what we described: apply by endorsement, get fingerprints done if not already on file, and declare the new state as your primary residence. Remember to also update your address officially with your old state board so they know you’ve left (they will then update your license status accordingly).
If your new state has not yet joined the compact but is in the process, you’ll have to get a license there as usual. Keep an eye out, though – if that state joins later, you might then become part of the compact automatically or have the option to convert. For instance, a nurse who moved to Pennsylvania in 2022 had to get a PA license (since PA’s NLC implementation was delayed), but once Pennsylvania implements the compact fully, that nurse could receive multistate privileges through PA at that time. Always stay informed via your board’s announcements in such cases.
Benefits of the NLC: Impact on Nurses, Healthcare Systems, and Patients
Why is the Nurse Licensure Compact grabbing so much attention? The answer is straightforward: the NLC delivers tangible payoffs. It unlocks wider job prospects for nurses while cutting licensure bureaucracy, and it helps hospitals and clinics ease workforce shortages in an era of tight staffing.
Expanded Job Opportunities
With a multistate license, a nurse can cast a much wider net for employment. You can easily apply for positions in any compact state without worrying about license barriers. This is ideal for travel nurses and per diem nurses who work short-term assignments in various states. It’s also great for nurses living near state lines or in multi-state metro areas (imagine living in Kansas City, KS but taking shifts in Missouri – compact licensure makes that seamless). According to one industry analysis, nurses in compact states can “take advantage of finding work in another state in the NLC with very little paperwork”. That flexibility can also translate to higher earning potential, as you’re not limited to your home state’s job market.
Saves Time and Money
Obtaining and renewing multiple single-state licenses can be costly and time-consuming. Each license might require an application fee, license verification, transcripts, fingerprinting, and continuing education requirements, not to mention renewal fees every few years. A compact license consolidates that to one state board. You pay one renewal fee, meet one set of renewal requirements, and you’re done. If a nurse relocates, they just have to pay for a new license in the new home state once, instead of maintaining two or more licenses. Over a career with multiple moves or travel assignments, this could save hundreds or thousands of dollars and countless hours of paperwork.
Remote and Telehealth Work
The explosion of telehealth in recent years, accelerated by the COVID-19 pandemic, has made multi-state practice privileges even more vital. Nurses can now work remotely for telehealth services, telephone triage, remote monitoring, case management, and more. The NLC allows a nurse in an NLC state to care for patients in any other compact state via telehealth without additional licenses. For example, a telehealth diabetes educator in Missouri can follow up with patients in Iowa and Arkansas (both compact states) freely. This opens up employment options like working from home for a healthcare company that serves patients nationwide. It also enables innovative care models, such as centralized teleICU nurses or remote hospice coordinators, improving patient access to specialized nursing skills regardless of geographic location.
Streamlined Disaster/Emergency Response
Nurses with a compact license can more rapidly respond to emergencies across state lines. During natural disasters or public health crises, a state in need can quickly import nurses from other compact states without emergency waivers or bureaucratic delays. We saw this concept in action during the COVID-19 pandemic, when states issued emergency orders to let out-of-state health professionals work in overstretched hospitals. The NLC provides a permanent framework for that kind of rapid response. A compact state can receive help from any other member state instantly – nurses just travel and start working, since their license is already valid. As one summary noted, in disasters a compact “can send the appropriate amount of nurses to areas that need them the most” more efficiently. This not only helps the disaster-stricken area but also provides valuable experience and opportunities for the responding nurses.
Maintaining Skills and Career Flexibility
Nurses often face life changes (family moves, spousal job relocations, etc.). The NLC makes it easier to continue one’s career uninterrupted by a move. Military spouse nurses, for example, have significantly benefited – they can transfer their license quickly wherever their family is stationed, reducing career disruption. Even for civilian nurses, the psychological benefit of knowing “I won’t have to jump through hoops to move for my dream job or personal life reason” can be huge. It encourages mobility and maybe even encourages nurses to venture into areas of high need (rural or understaffed states) because one major barrier is removed.
Easing Nurse Shortages
The United States has been grappling with nursing shortages in many regions. While the causes of these shortages are complex (including aging workforce, burnout, educational bottlenecks, etc.), the NLC offers one piece of the solution by redistributing available nurses more efficiently. If one state is experiencing a severe shortage, being part of the compact allows it to recruit nurses from a larger pool of talent across other states. For example, a hospital in Washington (which recently joined the NLC) can now more easily hire a qualified nurse from Texas or Ohio without waiting for a new license, which might make Washington a more attractive destination especially since it has high nurse wages. An NCSBN official noted that states see the NLC as part of “broader workforce discussions” to shore up their nurse supply and stay competitive in recruiting. In other words, states are starting to realize that if they don’t join, they may be at a disadvantage because nurses might prefer moving to or taking assignments in compact states where licensure is simpler.
Improving Patient Access in Underserved Areas
Rural communities and small hospitals often struggle to recruit enough nurses or certain specialists. The NLC can help by not limiting hiring to local-license nurses. A rural hospital in Wyoming (compact state) can more readily hire remote telehealth nurses or temporary staff from other states as needed. Home health and hospice agencies can serve patients across a wider geographic area by employing nurses from neighboring states. Also, patients in rural or underserved areas can access telehealth nursing services (like remote care management, lactation consulting, mental health nursing, etc.) from nurses located in other states, as long as both states are in the compact. This can dramatically improve access to care for populations that traditionally have shortages of providers.
Continuity of Care Across State Lines
For patients who live near state borders or travel seasonally (think “snowbirds” who spend winters in the south), the NLC facilitates better continuity. A patient with a complex condition who summers in Wisconsin and winters in Arizona could have the same telehealth nurse case-manager follow up with them year-round, since both states are compact. Or a home health nurse in Kansas can temporarily cross into Missouri to see a patient if needed without legal issues. Health systems that operate in multiple states (increasingly common as hospital networks merge) also benefit – they can deploy their nursing workforce fluidly to meet demand at different facilities. It reduces administrative overhead for hospitals needing to ensure all their staff are licensed in the correct jurisdictions.
Educational and Collaborative Opportunities
The NLC also allows for more fluid academic and training collaborations. Nursing faculty and preceptors can work with students across states without extra licenses. Healthcare organizations can set up regional float pools or resource teams that cover multiple states. All of this fosters a more integrated healthcare delivery approach, which is especially important as telehealth blurs traditional state boundaries in care delivery.
Public Safety Mechanisms
From a regulatory standpoint, the compact’s information-sharing increases public protection. By knowing that every compact nurse had a federal background check and meets a high standard, states can be assured of baseline quality. The sharing of discipline data means a nurse with a history of serious violations cannot hide that by moving states – their privilege can be swiftly curtailed if needed across all member states. This arguably makes the public safer than the old system, where a nurse could be revoked in one state but still hold licenses in others that might not immediately know about the issue. A nursing commission executive in Washington noted that the compact enhances public protection through coordinated efforts of all member boards and FBI background checks for all multistate licensees. The upshot is that the compact boosts both flexibility and safety when properly implemented.
Examples and Data
Surveys and Research
Surveys of nurses have generally shown support for the NLC. In one recent multi-state survey project, over 66,000 nurses across several states shared their views on the compact. While detailed results aren’t described here, the fact that so many participated indicates high interest. Many nurses cite the benefits of easier mobility and license cost savings. However, some also express concerns (like fear of increased competition for local jobs or potential dilution of state standards). On the employer side, hospital associations and large health systems have been among the biggest proponents of the NLC, often lobbying state legislatures to join because they see firsthand how licensure bottlenecks can delay hiring critical staff.
Workforce Impact
It’s difficult to measure exactly how much the NLC alone has alleviated nursing shortages, since many factors are at play. Some opponents note that compact membership by itself doesn’t guarantee more nurses will suddenly move to your state – for example, one analysis by a nursing union suggested that being in the compact had “little impact on nurse staffing levels at hospitals” and that issues like wages and working conditions are the true determinants of nurse supply. This is a fair point: a state won’t solve a shortage just by joining the compact if it doesn’t also address why nurses are leaving (e.g. burnout or low pay). However, the NLC certainly removes a barrier to staffing. It makes it easier and faster for willing nurses to go where jobs are available. During COVID surges, for instance, states in the compact could deploy traveling nurses faster. NCSBN and other proponents view the NLC as “one tool in the toolbox” to help ease workforce challenges – not a silver bullet, but a valuable mechanism among other strategies (like increasing nursing school capacity, improving workplace conditions, etc.).
Numbers of Multistate Nurses
Over two million nurses live in states that are part of the compact and therefore have the opportunity to obtain a multistate license. This stat (from NCSBN a few years ago) highlights the scale: literally millions of nurses are either already holding multistate licenses or eligible to get one. Each year, as more states join, that number grows. For example, after a large state like Pennsylvania or Massachusetts implements the compact, tens of thousands more nurses will become part of the compact system. This growing network of compact nurses creates a more flexible national workforce. We’ve also seen increased enrollment in nurse licensure compact privilege usage for telehealth companies, travel nurse agencies, and telenursing education. Essentially, the compact has enabled a new era of interstate nursing practice that was not possible a generation ago.
The NLC’s impact can be summarized as improving mobility for nurses, flexibility for health services, and potentially access to care for patients, all while keeping safeguards in place. It is a response to the modern reality that healthcare delivery and nurse careers are no longer neatly confined to one state at a time. Nurses value it for the career freedom it provides, and many healthcare leaders value it for helping address staffing needs and expanding care reach.
The APRN Compact
The APRN Compact is a proposed interstate agreement that would let advanced practice nurses—NPs, CNSs, CNMs, and CRNAs—hold one multistate license and provide care (in person or via telehealth) in every member state. The National Council of State Boards of Nursing finalized the current compact in 2020, but it will not take effect until at least seven states enact it. So far only Delaware, North Dakota, South Dakota, and Utah have signed on, leaving APRNs still needing separate licenses in each state where they practice.
Modeled on the RN/LPN Nurse Licensure Compact, the APRN version has extra safeguards. Applicants must hold an unencumbered RN license, graduate from an accredited APRN program, earn national certification in their role and population focus, pass an FBI background check, and log 2,080 clinical hours of APRN practice. Once active, the home state would issue the license, but APRNs would still follow each remote state’s scope-of-practice laws, and disciplinary actions would be shared across states.
Supporters say a multistate APRN license would widen telehealth reach, speed disaster response, cut red tape for military families, and trim duplicative licensing costs. Adoption has been slow, however, partly because some professional groups disagree with the 2,080-hour requirement and want stronger APRN input in compact governance. If three more states enact the compact, it will launch—likely prompting others to follow and greatly boosting APRN mobility. Until then, advocacy through state legislatures and professional associations remains the path forward.
Supporting NLC Legislation in Your State: Advocacy Tips for Nurses
If your state has not yet joined the Nurse Licensure Compact (or if it has enacted but not implemented it yet), you might be interested in helping make it a reality. Nurses can be powerful advocates for licensure compacts, as seen in states like Massachusetts where years of persistent advocacy finally led to success. Here are some ways you, as a nursing professional, can support compact legislation:
Stay Informed and Educate Others
Start by educating yourself on the facts about the NLC. Read official resources from NCSBN and your state board. Understand the pros (and cons) that are being discussed. Then, educate your peers and employer. Misconceptions about the compact (e.g., “it will lower standards” or “flood our state with outsiders”) can stall legislation. By sharing accurate information and real-world examples of how the compact helps nurses and patients, you can shift opinions. Consider hosting a short info session at your workplace or writing a piece for your state nursing association newsletter. The NCSBN’s NLC Toolkit and FAQs are useful for addressing common questions. Emphasize how the NLC maintains safety (with FBI background checks and uniform requirements) while offering flexibility. Sometimes nurses fear change – hearing from fellow nurses who have benefited (like travel nurses or military spouses) can personalize the issue.
Engage with Your State Nurses Association and Other Stakeholders
Find out your state nursing association’s stance on the NLC. In some states (e.g., Massachusetts, New York, California), the dominant nurses’ unions or associations had historical reservations. But there are often other groups, like specialty nursing associations or hospital associations, that strongly support it. Join the conversation. If your nurses association supports the compact, lend your voice – you might volunteer for their legislative committee or help with testimony. If they oppose it, respectfully raise the question of reconsidering, armed with data and examples. Sometimes opposition is based on outdated concerns (for instance, worrying about standards which have since been addressed by the eNLC). Additionally, engage with healthcare consumer groups, patient advocates, and physician organizations in your state – many will support the compact because of the access to care benefits. A “diverse range of stakeholders” coming together was key in Massachusetts’ passage, including hospitals, long-term care providers, veterans groups, and nurses.
Contact Your Legislators
This is critical. Lawmakers respond to constituents. Find out if a compact bill exists in the current session. If yes, write or call the sponsors to express your support and offer any personal anecdotes of why it’s needed. Also contact your own state representative and senator to urge them to vote yes. Be professional and succinct: explain who you are (“I’m an RN in your district with X years of experience”) and why the compact matters (maybe share how you faced licensing hassles, or how during COVID you wished you could easily volunteer in another state).
NCSBN’s Take Action tool can simplify this – it provides an online form to send a message to your legislators about supporting the NLC. This tool often pre-fills a message which you can personalize. Even if a bill isn’t introduced yet, reaching out to lawmakers to put it on their radar is helpful. Some states took years of repeated bills before one passed – persistence matters.
Provide Testimony or Letters of Support
When a compact bill gets a hearing in the legislature, lawmakers invite public testimony. You can testify in person or submit written testimony. This is a chance to counter any opposition’s arguments. For instance, if a nurses’ union leader testifies that “NLC won’t solve our staffing,” you might testify how the NLC would have helped you fill a staffing gap or how it would make your life easier as a bedside nurse. Or if opponents worry about loss of licensing revenue for the state, you could point out how the state will save administrative costs long-term, etc.
Come prepared with facts (maybe cite a study or example from another state). Even a short, heartfelt testimony from a working nurse can leave an impression on lawmakers. Remember to highlight patient impact too – e.g., “My elderly patient moved to another state to live with family, and I wished I could continue to care for them via telehealth but licensing made it impossible. The NLC would remove that barrier.” Personal stories stick.
Collaborate with Employers and Healthcare Leaders
Hospitals and health systems are often champions of the compact because it helps with staffing and recruitment. See if your employer is already advocating for it; if not, encourage them to do so. Administrators can provide valuable data, like how many positions went unfilled or how many days of care were delayed due to licensing issues.
If you’re in a nursing leadership role, consider drafting a letter of support on behalf of your organization. Many state hospital associations actively lobby for the NLC – nurses can join these efforts to provide the clinical perspective. Also, nursing faculty can highlight how it helps education and clinical placements.
Grassroots Mobilization
Sometimes, simple grassroots efforts can make a difference. This could be a petition among nurses in your state supporting the compact, delivered to the legislature. Or a social media campaign sharing “Compact Facts” and using a hashtag to raise public awareness.
In today’s world, consider a quick video of nurses talking about why the NLC matters, directed at policymakers. Town hall meetings or community forums are opportunities to bring it up – frame it as an access to care issue for constituents. Nurses are consistently one of the most trusted professions, so your voice carries weight in public discourse.
Be Patient but Persistent
In many states, NLC legislation took multiple attempts. For example, it took over a decade of advocacy in Massachusetts to overcome opposition and pass the bill. Each year, more education was done, more stakeholders got on board, and data from other states (like how the compact didn’t cause harm in those states) helped alleviate fears. If your state doesn’t pass it this year, don’t be discouraged – keep the conversation going, as momentum can build over time. The landscape can shift suddenly (sometimes a new governor or a healthcare crisis can tip the scales). Keep yourself updated with any changes in legislation and continue to rally support.
APRN Compact Advocacy
If you’re an APRN, the above advice applies to supporting the APRN Compact too. That one may face even more debate, so APRNs should educate colleagues on what it truly entails. Engage with both nursing and physician groups to find common ground. Highlight the potential to improve patient access especially in primary care and mental health. As an APRN, you might emphasize that the compact doesn’t override state scope laws – it’s licensure, not changing practice authority directly. Address the concerns around the 2,080-hour requirement by discussing whether a compromise or future amendment could address it. Show that you’re open to fine-tuning but that the overall concept is sound.
Official Resources
Utilize official channels for advocacy. The NurseCompact.com website (by NCSBN) has a “Take Action” section with resources and even template letters. The APRNcompact.com site similarly encourages contacting legislators. Sharing links to these sites with colleagues or on social media can help others easily voice their support.












Leave a Comment