The major sources of the glucose that circulates in the blood are through the absorption of ingested food in the gastrointestinal tract and formation of glucose by the liver from food substances.
- Diabetes mellitus is a group of metabolic diseases that occurs with increased levels of glucose in the blood.
- Diabetes mellitus most often results in defects in insulin secretion, insulin action, or even both.
Classification
The classification system of diabetes mellitus is unique because research findings suggest many differences among individuals within each category, and patients can even move from one category to another, except for patients with type 1 diabetes.
- Diabetes has major classifications that include type 1 diabetes, type 2 diabetes, gestational diabetes, and diabetes mellitus associated with other conditions.
- The two types of diabetes mellitus are differentiated based on their causative factors, clinical course, and management.
Pathophysiology
Diabetes Mellitus has different courses of pathophysiology because of it has several types
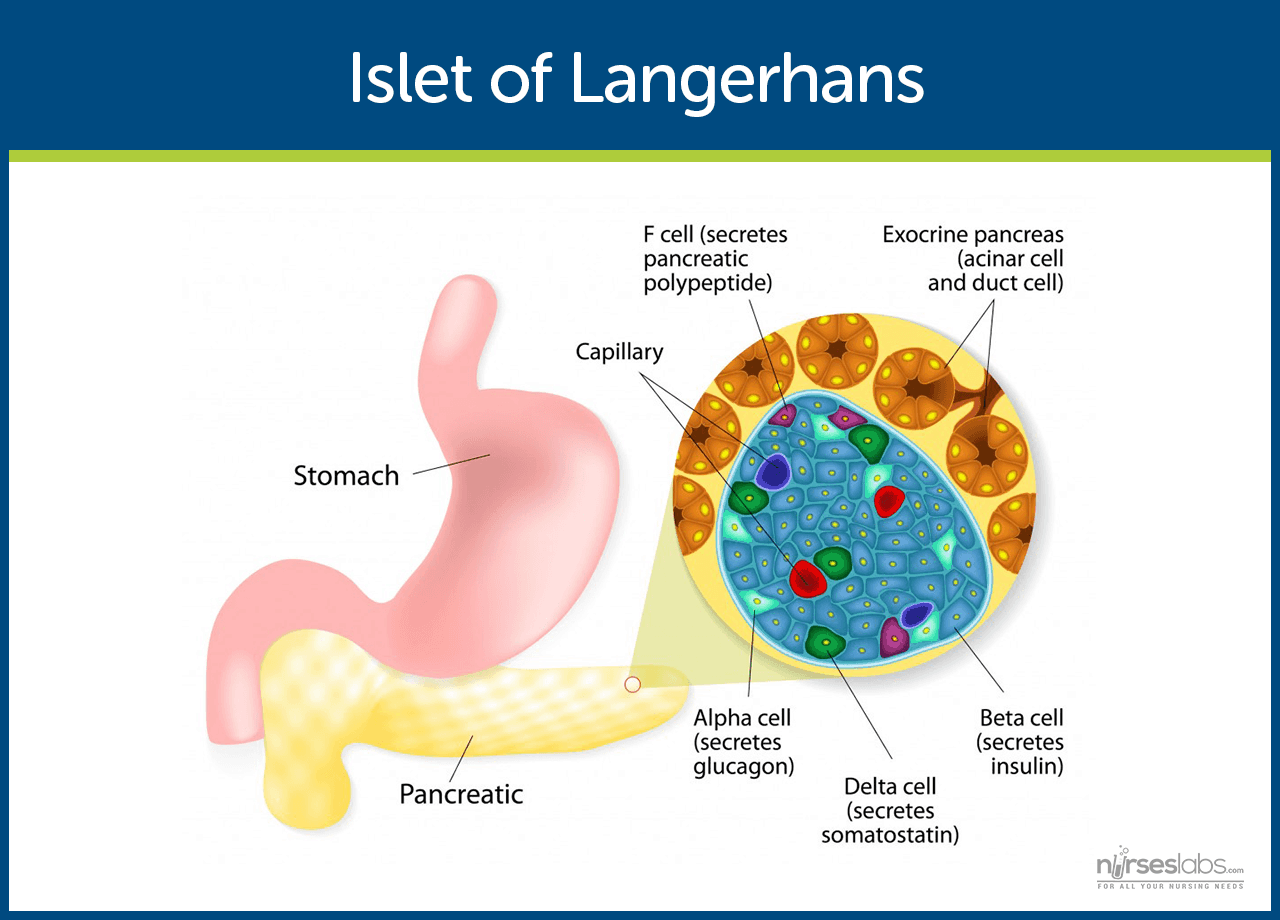
- Insulin is secreted by beta cells in the pancreas and it is an anabolic hormone.
- When we consume food, insulin moves glucose from blood to muscle, liver, and fat cells as insulin level increases.
- The functions of insulin include the transport and metabolism of glucose for energy, stimulation of storage of glucose in the liver and muscle, serves as the signal of the liver to stop releasing glucose, enhancement of the storage of dietary fat in adipose tissue, and acceleration of the transport of amino acid into cells.
- Insulin and glucagon maintain a constant level of glucose in the blood by stimulating the release of glucose from the liver.
Type 1 Diabetes Mellitus
- Type 1 diabetes mellitus is characterized by destruction of the pancreatic beta cells.
- A common underlying factor in the development of type 1 diabetes is a genetic susceptibility.
- Destruction of beta cells leads to a decrease in insulin production, unchecked glucose production by the liver and fasting hyperglycemia.
- Glucose taken from food cannot be stored in the liver anymore but remains in the blood stream.
- The kidneys will not reabsorb the glucose once it has exceeded the renal threshold, so it will appear in the urine and be called glycosuria.
- Excessive loss of fluids is accompanied by excessive excretion of glucose in the urine leading to osmotic diuresis.
- There is fat breakdown which results in ketone production, the by-product of fat breakdown.
Type 2 Diabetes Mellitus
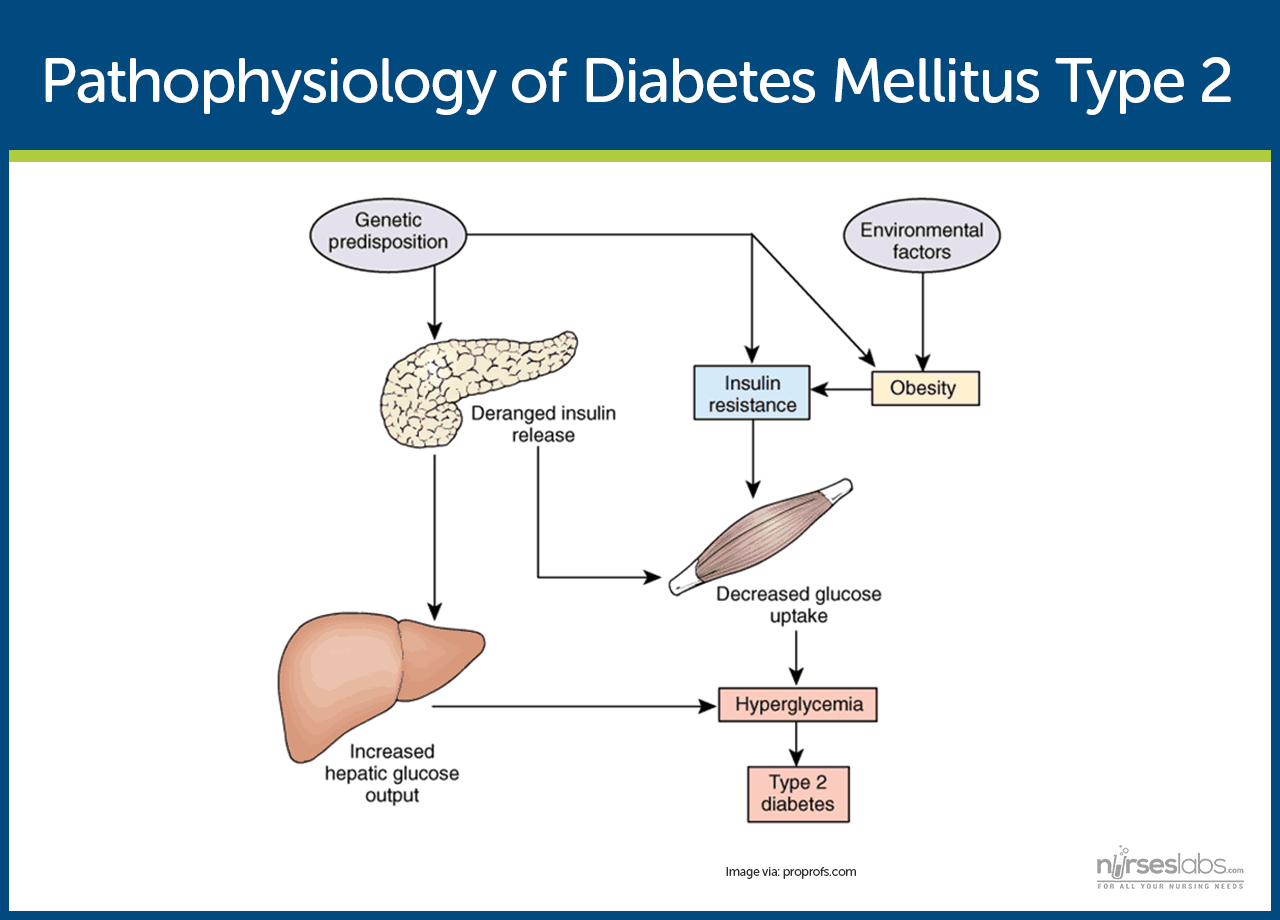
- Type 2 diabetes mellitus has major problems of insulin resistance and impaired insulin secretion.
- Insulin could not bind with the special receptors so insulin becomes less effective at stimulating glucose uptake and at regulating the glucose release.
- There must be increased amounts of insulin to maintain glucose level at a normal or slightly elevated level.
- However, there is enough insulin to prevent the breakdown of fats and production of ketones.
- Uncontrolled type 2 diabetes could lead to hyperglycemic, hyperosmolar nonketotic syndrome.
- The usual symptoms that the patient may feel are polyuria, polydipsia, polyphagia, fatigue, irritability, poorly healing skin wounds, vaginal infections, or blurred vision.
Gestational Diabetes Mellitus
- With gestational diabetes mellitus (GDM), the pregnant woman experiences any degree of glucose intolerance with the onset of pregnancy.
- The secretion of placental hormones causes insulin resistance, leading to hyperglycemia.
- After delivery, blood glucose levels in women with GDM usually return to normal or later on develop type 2 diabetes.
Epidemiology
Diabetes mellitus is now one of the most common disease all over the world. Here are some quick facts and numbers on diabetes mellitus.
- More than 23 million people in the United States have diabetes, yet almost one-third are undiagnosed.
- By 2030, the number of cases is expected to increase more than 30 million.
- Diabetes is especially prevalent in the elderly; 50% of people older than 65 years old have some degree of glucose intolerance.
- People who are 65 years and older account for 40% of people with diabetes.
- African-Americans and members of other racial and ethnic groups are more likely to develop diabetes.
- In the United States, diabetes is the leading cause of non-traumatic amputations, blindness in working-age adults, and end-stage renal disease.
- Diabetes is the third leading cause of death from disease.
- Costs related to diabetes are estimated to be almost $174 billion annually.
Causes
The exact cause of diabetes mellitus is actually unknown, yet there are factors that contribute to the development of the disease.
Type 1 Diabetes Mellitus
- Genetics. Genetics may have played a role in the destruction of the beta cells in type 1 DM.
- Environmental factors. Exposure to some environmental factors like viruses can cause the destruction of the beta cells.
Type 2 Diabetes Mellitus
- Weight. Excessive weight or obesity is one of the factors that contribute to type 2 DM because it causes insulin resistance.
- Inactivity. Lack of exercise and a sedentary lifestyle can also cause insulin resistance and impaired insulin secretion.
Gestational Diabetes Mellitus
- Weight. If you are overweight before pregnancy and added extra weight, it makes it hard for the body to use insulin.
- Genetics. If you have a parent or a sibling who has type 2 DM, you are most likely predisposed to GDM.
Clinical Manifestations
Clinical manifestations depend on the level of the patient’s hyperglycemia.
- Polyuria or increased urination. Polyuria occurs because the kidneys remove excess sugar from the blood, resulting in a higher urine production.
- Polydipsia or increased thirst. Polydipsia is present because the body loses more water as polyuria happens, triggering an increase in the patient’s thirst.
- Polyphagia or increased appetite. Although the patient may consume a lot of food but glucose could not enter the cells because of insulin resistance or lack of insulin production.
- Fatigue and weakness. The body does not receive enough energy from the food that the patient is ingesting.
- Sudden vision changes.The body pulls away fluid from the eye in an attempt to compensate the loss of fluid in the blood, resulting in trouble in focusing the vision.
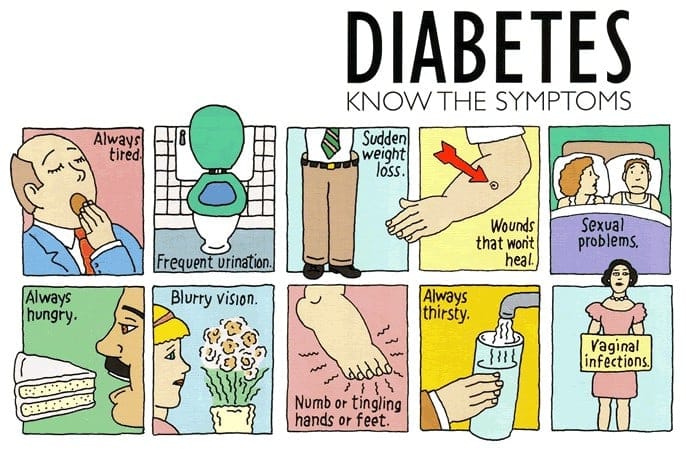
- Tingling or numbness in hands or feet. Tingling and numbness occur due to a decrease in glucose in the cells.
- Dry skin. Because of polyuria, the skin becomes dehydrated.
- Skin lesions or wounds that are slow to heal. Instead of entering the cells, glucose crowds inside blood vessels, hindering the passage of white blood cells which are needed for wound healing.
- Recurrent infections. Due to the high concentration of glucose, bacteria thrives easily.
Prevention
Appropriate management of lifestyle can effectively prevent the development of diabetes mellitus.
- Standard lifestyle recommendations, metformin, and placebo are given to people who are at high risk for type 2 diabetes.
- The 16-lesson curriculum of the intensive program of lifestyle modifications focused on weight reduction of greater than 7% of initial body weight and physical activity of moderate intensity.
- It also included behavior modification strategies that can help patients achieve their weight reduction goals and participate in exercise.
Complications
If diabetes mellitus is left untreated, several complications may arise from the disease
- Hypoglycemia. Hypoglycemia occurs when the blood glucose falls to less than 50 to 60 mg/dL because of too much insulin or oral hypoglycemic agents, too little food, or excessive physical activity.
- Diabetic Ketoacidosis. DKA is caused by an absence or markedly inadequate amounts of insulin and has three major features of hyperglycemia, dehydration and electrolyte loss, and acidosis.
- Hyperglycemic Hyperosmolar Nonketotic Syndrome. HHNS is a serious condition in which hyperosmolarity and hyperglycemia predominate with alteration in the sense of awareness.
Assessment and Diagnostic Findings
Hypoglycemia may occur suddenly in a patient considered hyperglycemic because their blood glucose levels may fall rapidly to 120 mg/dL or even less.
- Serum glucose: Increased 200–1000 mg/dL or more.
- Serum acetone (ketones): Strongly positive.
- Fatty acids: Lipids, triglycerides, and cholesterol level elevated.
- Serum osmolality: Elevated but usually less than 330 mOsm/L.
- Glucagon: Elevated level is associated with conditions that produce (1) actual hypoglycemia, (2) relative lack of glucose (e.g., trauma, infection), or (3) lack of insulin. Therefore, glucagon may be elevated with severe DKA despite hyperglycemia.
- Glycosylated hemoglobin (HbA1C): Evaluates glucose control during past 8–12 wk with the previous 2 wk most heavily weighted. Useful in differentiating inadequate control versus incident-related DKA (e.g., current upper respiratory infection [URI]). A result greater than 8% represents an average blood glucose of 200 mg/dL and signals a need for changes in treatment.
- Serum insulin: May be decreased/absent (type 1) or normal to high (type 2), indicating insulin insufficiency/improper utilization (endogenous/exogenous). Insulin resistance may develop secondary to formation of antibodies.
- Electrolytes:
- Sodium: May be normal, elevated, or decreased.
- Potassium: Normal or falsely elevated (cellular shifts), then markedly decreased.
- Phosphorus: Frequently decreased.
- Arterial blood gases (ABGs): Usually reflects low pH and decreased HCO3 (metabolic acidosis) with compensatory respiratory alkalosis.
- CBC: Hct may be elevated (dehydration); leukocytosis suggest hemoconcentration, response to stress or infection.
- BUN: May be normal or elevated (dehydration/decreased renal perfusion).
- Serum amylase: May be elevated, indicating acute pancreatitis as cause of DKA.
- Thyroid function tests: Increased thyroid activity can increase blood glucose and insulin needs.
- Urine: Positive for glucose and ketones; specific gravity and osmolality may be elevated.
- Cultures and sensitivities: Possible UTI, respiratory or wound infections.
Medical Management
Here are some medical interventions that are performed to manage diabetes mellitus.
- Normalize insulin activity. This is the main goal of diabetes treatment — normalization of blood glucose levels to reduce the development of vascular and neuropathic complications.
- Intensive treatment. Intensive treatment is three to four insulin injections per day or continuous subcutaneous insulin infusion, insulin pump therapy plus frequent blood glucose monitoring and weekly contacts with diabetes educators.
- Exercise caution with intensive treatment. Intensive therapy must be done with caution and must be accompanied by thorough education of the patient and family and by responsible behavior of patient.
- Diabetes management has five components and involves constant assessment and modification of the treatment plan by healthcare professionals and daily adjustments in therapy by the patient.
Nutritional Management
- The foundations. Nutrition, meal planning, and weight control are the foundations of diabetes management.
- Consult a professional. A registered dietitian who understands diabetes management has the major responsibility for designing and teaching this aspect of the therapeutic plan.
- Healthcare team should have the knowledge. Nurses and other health care members of the team must be knowledgeable about nutritional therapy and supportive of patients who need to implement nutritional and lifestyle changes.
- Weight loss. This is the key treatment for obese patients with type 2 diabetes.
- How much weight to lose? A weight loss of as small as 5% to 10% of the total body weight may significantly improve blood glucose levels.
- Other options for diabetes management. Diet education, behavioral therapy, group support, and ongoing nutritional counselling should be encouraged.
Meal Planning
- Criteria in meal planning. The meal plan must consider the patient’s food preferences, lifestyle, usual eating times, and ethnic and cultural background.
- Managing hypoglycemia through meals. To help prevent hypoglycemic reactions and maintain overall blood glucose control, there should be consistency in the approximate time intervals between meals with the addition of snacks as needed.
- Assessment is still necessary. The patient’s diet history should be thoroughly reviewed to identify his or her eating habits and lifestyle.
- Educate the patient. Health education should include the importance of consistent eating habits, the relationship of food and insulin, and the provision of an individualized meal plan.
- The nurse‘s role. The nurse plays an important role in communicating pertinent information to the dietitian and reinforcing the patients for better understanding.
Other Dietary Concerns
- Alcohol consumption. Patients with diabetes do not need to give up alcoholic beverages entirely, but they must be aware of the potential adverse of alcohol specific to diabetes.
- If a patient with diabetes consumes alcohol on an empty stomach, there is an increased likelihood of hypoglycemia.
- Reducing hypoglycemia. The patient must be cautioned to consume food along with alcohol, however, carbohydrate consumed with alcohol may raise blood glucose.
- How much alcohol intake? Moderate intake is considered to be one alcoholic beverage per day for women and two alcoholic beverages per day for men.
- Artificial sweeteners. Use of artificial sweeteners is acceptable, and there are two types of sweeteners: nutritive and nonnutritive.
- Types of sweeteners. Nutritive sweeteners include all of which provides calories in amounts similar to sucrose while nonnutritive have minimal or no calories.
- Exercise. Exercise lowers blood glucose levels by increasing the uptake of glucose by body muscles and by improving insulin utilization.
- A person with diabetes should exercise at the same time and for the same amount each day or regularly.
- A slow, gradual increase in the exercise period is encouraged.
Using a Continuous Glucose Monitoring System
- A continuous glucose monitoring system is inserted subcutaneously in the abdomen and connected to the device worn on a belt.
- This can be used to determine whether treatment is adequate over a 24-hour period.
- Blood glucose readings are analyzed after 72 hours when the data has been downloaded from the device.
Testing for Glycated Hemoglobin
- Glycated hemoglobin or glycosylated hemoglobin, HgbA1C, or A1C reflects the average blood glucose levels over a period of approximately 2 to 3 months.
- The longer the amount of glucose in the blood remains above normal, the more glucose binds to hemoglobin and the higher the glycated hemoglobin becomes.
- Normal values typically range from 4% to 6% and indicate consistently near-normal blood glucose concentrations.
Pharmacologic Therapy
- Exogenous insulin. In type 1 diabetes, exogenous insulin must be administered for life because the body loses the ability to produce insulin.
- Insulin in type 2 diabetes. In type 2 diabetes, insulin may be necessary on a long-term basis to control glucose levels if meal planning and oral agents are ineffective.
- Self-Monitoring Blood Glucose (SMBG). This is the cornerstone of insulin therapy because accurate monitoring is essential.
- Human insulin. Human insulin preparations have a shorter duration of action because the presence of animal proteins triggers an immune response that results in the binding of animal insulin.
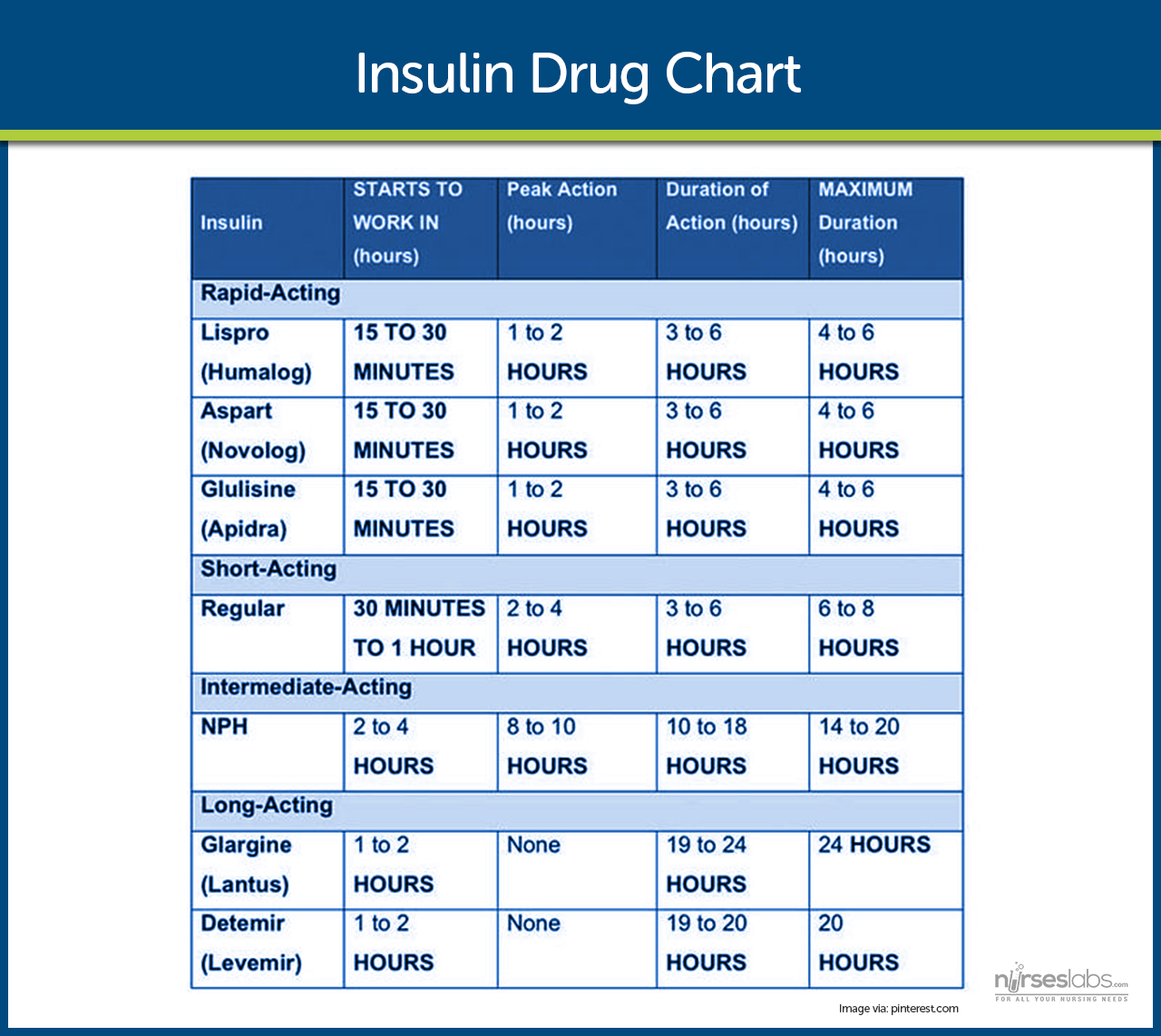
- Rapid-acting insulin. Rapid-acting insulins produce a more rapid effect that is of shorter duration than regular insulin.
- Short-acting insulin. Short-acting insulins or regular insulin should be administered 20-30 minutes before a meal, either alone or in combination with a longer-acting insulin.
- Intermediate-acting insulin. Intermediate-acting insulins or NPH or Lente insulin appear white and cloudy and should be administered with food around the time of the onset and peak of these insulins.
- The rapid-acting and short-acting insulins are expected to cover the increase in blood glucose levels after meals; immediately after the injection.
- Intermediate-acting insulins are expected to cover subsequent meals, and long-acting insulins provide a relatively constant level of insulin and act as a basal insulin.
- Approaches to insulin therapy. There are two general approaches to insulin therapy: conventional and intensive.
- Conventional regimen. Conventional regimen is a simplified regimen wherein the patient should not vary meal patterns and activity levels.
- Intensive regimen. Intensive regimen uses a more complex insulin regimen to achieve as much control over blood glucose levels as is safe and practical.
- A more complex insulin regimen allows the patient more flexibility to change the insulin doses from day to day in accordance with changes in eating and activity patterns.
- Methods of insulin delivery. Methods of insulin delivery include traditional subcutaneous injections, insulin pens, jet injectors, and insulin pumps.
- Insulin pens use small prefilled insulin cartridges that are loaded into a pen-like holder.
- Insulin is delivered by dialing in a dose or pushing a button for every 1- or 2-unit increment administered.
- Jet injectors deliver insulin through the skin under pressure in an extremely fine stream.
- Insulin pumps involve continuous subcutaneous insulin infusion with the use of small, externally worn devices that closely mimic the function of the pancreas.
- Oral antidiabetic agents may be effective for patients who have type 2 diabetes that cannot be treated by MNT and exercise alone.
- Oral antidiabetic agents. Oral antidiabetic agents include sulfonylureas, biguanides, alpha-glucosidase inhibitors, thiazolidinediones, and dipeptidyl-peptidase-4.
- Half of all the patients who used oral antidiabetic agents eventually require insulin, and this is called secondary failure.
- Primary failure occurs when the blood glucose level remains high 1 month after initial medication use.
Nursing Management
Nurses should provide accurate and up-to-date information about the patient’s condition so that the healthcare team can come up with appropriate interventions and management.
For the complete and comprehensive nursing care plan and management of patients with diabetes, please visit 20 Diabetes Mellitus Nursing Care Plans
Practice Quiz: Diabetes Mellitus
For our diabetes mellitus practice quiz, please do visit our nursing test bank for diabetes:

Humbled by the content I read here.. this is absolutely exceptional..work made easier
please can you give me your opinion on this weather is “Diabetes- only progression or can be regressed”
Perfect notes
Lesson is extremely explicit and easy to grasp
Hi Jennifer, Awesome to hear the lesson on diabetes mellitus was clear and easy to get! 😊 Anything in particular you found really helpful or any other topics you’re keen to explore?
Very good
Very effective