Congenital Talipes Equinovarus, commonly known as clubfoot, is a congenital musculoskeletal deformity affecting the foot and ankle, present at birth. This condition is characterized by an inward and downward twisting of the foot, causing it to appear turned inwards and pointed downwards. Clubfoot can affect one or both feet and occurs due to abnormal development of the foot’s bones, tendons, and ligaments during fetal development.
This nursing note tackles Congenital Talipes Equinovarus, exploring its causes, clinical manifestations, diagnostic findings, management, and nursing interventions applicable to the affected infants.
Table of Contents
- What is Congenital Talipes Equinovarus?
- Pathophysiology
- Causes
- Statistics and Incidences
- Clinical Manifestations
- Assessment and Diagnostic Findings
- Medical Management
- Surgical Management
- Nursing Management
What is Congenital Talipes Equinovarus?
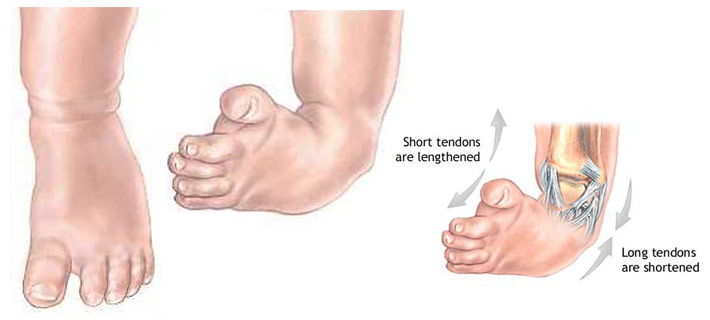
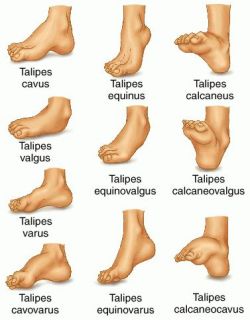
Congenital talipes equinovarus or clubfoot is usually evident at birth. It is a deformity in which the entire foot is inverted, the heel is drawn up, and the forefoot is adducted.
- The Latin talus, meaning ankle, and pes, meaning foot, make up the word talipes, which is used in connection with many foot deformities.
- Clubfoot was depicted in Egyptian hieroglyphs and was described by Hippocrates around 400 bc; he advised treatment with manipulation and bandages, ‘manipulate the foot as if holding a wax model, not by force, but gently’.
- The Pirani, Goldner, Diméglio, Hospital for Joint Diseases (HJD), and Walker classifications have been published, but no classification system is universally used.
Pathophysiology
Various theories of the pathogenesis of clubfoot have been advanced.

- With respect to neurogenic factors, histochemical abnormalities have been found in posteromedial and peroneal muscle groups of patients with clubfeet.
- This is postulated to be due to innervation changes in intrauterine life secondary to a neurologic event, such as a stroke leading to mild hemiparesis or paraparesis.
- Retracting fibrosis (or myofibrosis) may occur secondary to increased fibrous tissue in muscles and ligaments.
- In fetal and cadaveric studies, Ponseti also found the collagen in all of the ligamentous and tendinous structures (except the Achilles [calcaneal] tendon), and it was very loosely crimped and could be stretched.
- The Achilles tendon, on the other hand, was made up of tightly crimped collagen and was resistant to stretching; Zimny et al found myoblasts in medial fascia on electron microscopy and postulated that they cause medial contracture.
Causes
The true etiology of congenital clubfoot is unknown.
- Extrinsic factors. Extrinsic associations include teratogenic agents (e.g., sodium aminopterin), oligohydramnios, and congenital constriction rings.
- Genetic factors. Genetic associations include Mendelian inheritance (eg, diastrophic dwarfism; autosomal recessive pattern of clubfoot inheritance).
- Cytogenic factors. Cytogenetic abnormalities (e.g., congenital talipes equinovarus [CTEV]) can be seen in syndromes involving chromosomal deletion; it has been proposed that idiopathic CTEV in otherwise healthy infants is the result of a multifactorial system of inheritance.
Statistics and Incidences
The incidence of clubfoot differs among ethnicities.

- The incidence of clubfoot is approximately 1 case per 1000 live births in the United States.
- The male-to-female ratio has been reported to be 2:1; bilateral involvement is found in 30-50% of cases; a 2017 study by Zionts et al found that severity did not differ significantly by either sex or bilaterality, though patients with bilateral clubfoot had a wider range of severity.
- There is a 10% chance of a subsequent child being affected if the parents already have a child with clubfoot.

- Parker et al pooled data from several birth defects surveillance programs (6139 cases of clubfoot) to better estimate the prevalence of clubfoot and investigate its risk factors; the overall prevalence of clubfoot was 1.29 per 1000 live births, with figures of 1.38 among non-Hispanic whites, 1.30 among Hispanics, and 1.14 among non-Hispanic blacks or African Americans.
- Maternal age, parity, education, and marital status were significantly associated with clubfoot, along with maternal smoking and diabetes.
Clinical Manifestations
Most infants who have clubfoot have no identifiable genetic, syndromal, or extrinsic cause.
- Foot abnormality. The ankle is in equinus, and the foot is supinated (varus) and adducted (a normal infant foot usually can be dorsiflexed and everted, so that the foot touches the anterior tibia).
- Bone displacement. The navicular is displaced medially, as is the cuboid.
- Contractures. Contractures of the medial plantar soft tissues are present; not only is the calcaneus in a position of equinus, but also the anterior aspect is rotated medially and the posterior aspect laterally.
- Empty heel. The heel is small and empty; the heel feels soft to the touch (akin to the feel of the cheeks); as the treatment progresses, it fills in and develops a firmer feel (akin to the feel of the nose or of the chin).
Assessment and Diagnostic Findings

Occasionally, radiographs are necessary to diagnose clubfeet associated with tibial hemimelia.
- Radiographs. Talocalcaneal parallelism is the radiographic feature of clubfeet; the anteroposterior (AP) view is taken with the foot in 30° of plantarflexion and the tube at 30° from vertical. The lateral view is taken with the foot in 30° of plantarflexion.
Medical Management
The aims of medical therapy for clubfoot are to correct the deformity early and fully and to maintain the correction until growth stops.
- The Pirani scoring system. The Pirani scoring system, devised by Shafiq Pirani, MD, of Vancouver, BC, consists of six categories, three in the hindfoot and three in the midfoot; the Pirani scoring system can be used to identify the severity of the clubfoot and to monitor the correction.
- Traditional nonoperative treatment. With traditional nonoperative treatment, splintage begins at 2-3 days after birth; merely bring the foot to the best position obtainable, and maintain this position either by strapping every few days or by changing casting weekly until either full correction is obtained or correction is halted by some irresistible force.
- The Ponseti method. This method was developed by Ignacio Ponseti, MD, of the University of Iowa; the premise of the method is based on Ponseti’s cadaveric and clinical observations; a 2014 Cochrane review found this approach to yield significantly better results than either the Kite method or a traditional approach, though it noted that the quality of the evidence was not high; a study by Dragoni et al suggested that this approach may be effective for treatment of rigid residual deformity of congenital clubfoot after walking age.
Surgical Management
Although it is sometimes recommended that idiopathic clubfoot is treated as soon as possible, this condition does not constitute an orthopedic emergency.

- Surgical clubfoot release. In the past, clubfoot surgery was performed in a way that did not differentiate severity; the same procedure was performed for all patients; Bensahel proposed a more individualized approach (ie, addressing only the structures that are required are released); the surgery is tailored to the deformity.
Nursing Management
Nursing care of an infant with clubfoot include the following:
Nursing Assessment
Assessment of a child with clubfoot include:
- History. Seek a detailed family history of clubfoot or neuromuscular disorders, and perform a general examination to identify any other abnormalities.
- Physical exam. Examine the feet with the child prone, with the plantar aspect of the feet visualized, and supine to evaluate internal rotation and varus; if the child can stand, determine whether the foot is plantigrade, whether the heel is bearing weight, and whether it is in varus, valgus, or neutral.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses are:
- Disturbed body image related to permanent alteration in structure and/or function.
- Deficient knowledge related to the condition, prognosis, treatment, self-care, and discharge needs.
- Risk for peripheral neurovascular dysfunction related to mechanical compression (cast or brace).
- Risk for impaired skin integrity related to cast application, traction or surgery.
- Risk for impaired parenting related to maladaptive coping strategies secondary to diagnosis of talipes deformity.
Nursing Care Planning and Goals
The major nursing care planning goals for patients with congenital talipes equinovarus (clubfoot) are:
- Parents verbalize acceptance of self in the situation
- Family/SO discuss about situation and changes that would have occurred.
- Parents develop realistic goals/plans for the future.
- Parents explain disease state, recognizes the need for medications and understands treatments.
- Parents demonstrate how to incorporate new health regimen into lifestyle.
- Parents exhibit ability to deal with health situation and remain in control of life.
- Parents demonstrate an understanding of plan to heal tissue and prevent injury.
- Parents describe measures to protect and heal the tissue, including wound care.
Nursing Interventions
Nursing interventions for the child are:
- Protect skin integrity. Monitor site of impaired tissue integrity at least once daily for color changes, redness, swelling, warmth, pain, or other signs of infection; monitor patient’s skin care practices, noting type of soap or other cleansing agents used, temperature of water, and frequency of skin cleansing; and provide gloves or clip the nails if necessary to avoid damaging the skin with scratches.
- Promote acceptance of body image. Acknowledge and accept an expression of feelings of frustration, dependency, anger, grief, and hostility; support verbalization of positive or negative feelings about the actual or perceived loss; and be realistic and positive during treatments, in health teaching, and in setting goals within limitations.
- Provide health education. Include the parents in creating the teaching plan, beginning with establishing objectives and goals for learning at the beginning of the session; provide clear, thorough, and understandable explanations and demonstrations; and render positive, constructive reinforcement of learning.
Evaluation
Goals are met as evidenced by:
- Parents verbalized acceptance of self in situation
- Family/SO discussed about situation and changes that would have occurred.
- Parents developed realistic goals/plans for the future.
- Parents explained disease state, recognizes need for medications, and understands treatments.
- Parents demonstrated how to incorporate new health regimen into lifestyle.
- Parents exhibited ability to deal with health situation and remain in control of life.
- Parents demonstrated an understanding of plan to heal tissue and prevent injury.
- Parents described measures to protect and heal the tissue, including wound care.
Documentation Guidelines
Documentation in a child with clubfoot include:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Characteristics of the skin.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.