Kris, a 9-year old, loves dancing. She is a famous dancer at school, and a good one too. In between classes and dance lessons is her love for juices and carbonated drinks. She love it so much that even when everyone’s asleep she would sneak a pack of powdered juice and mix it inside her bedroom, and drank the whole pitcher by herself. You see, diabetes mellitus runs in Kris’ family, and it did not take long enough for her parents to found out that she has one too.
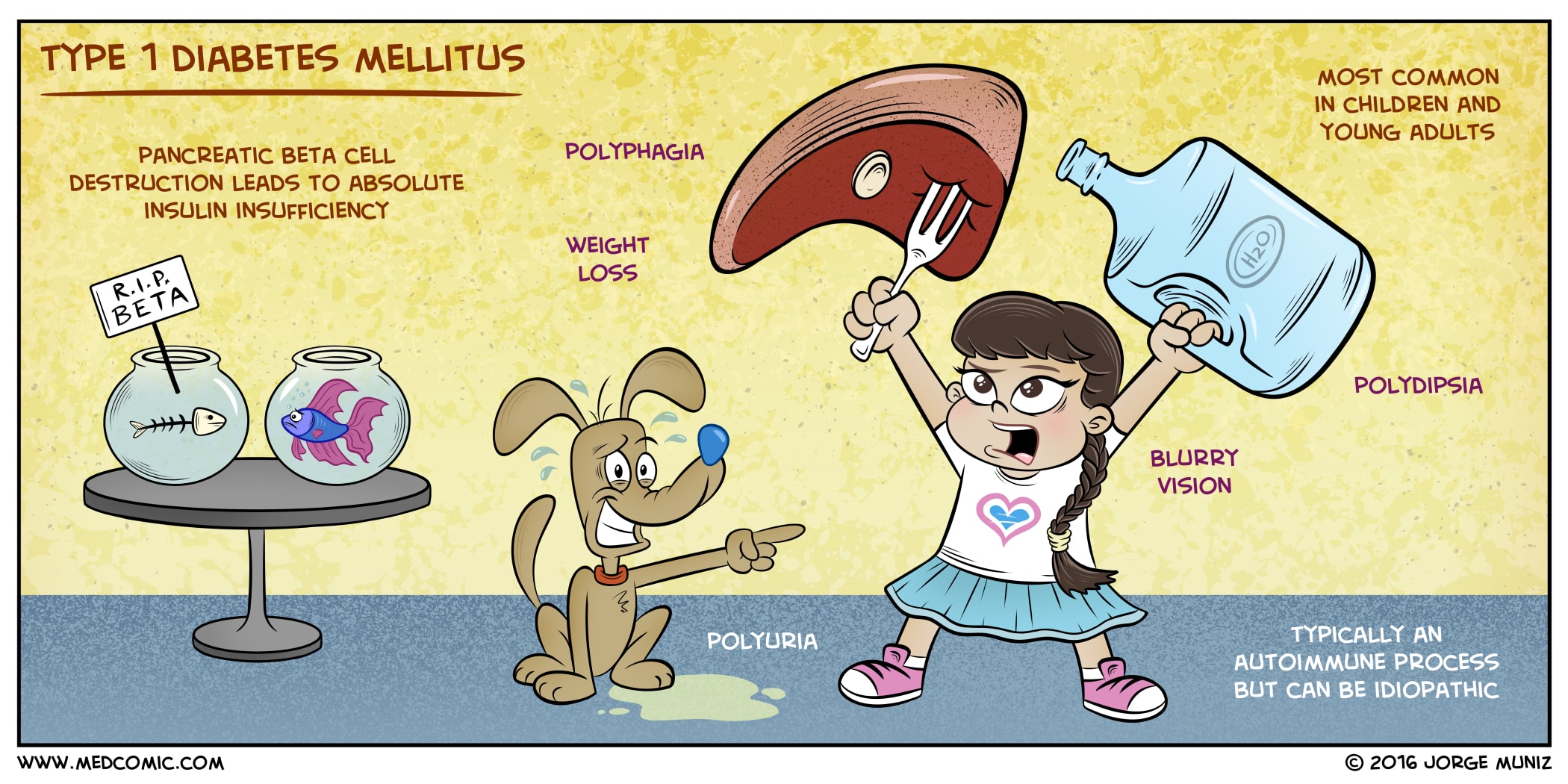
Diabetes Mellitus type 1, often referred to as type 1 diabetes, is a chronic autoimmune disorder that affects the body’s ability to produce insulin. Unlike type 2 diabetes, which is linked to insulin resistance, type 1 diabetes occurs when the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This results in an absolute deficiency of insulin, leading to high levels of glucose in the bloodstream.
Type 1 diabetes is typically diagnosed in children, adolescents, and young adults, and it requires lifelong insulin therapy for proper blood sugar management.
What is Type 1 Diabetes Mellitus?
Most pediatric patients with diabetes have type 1 diabetes mellitus (T1DM) and a lifetime dependence on exogenous insulin.
- Diabetes mellitus (DM) is a chronic metabolic disorder caused by an absolute or relative deficiency of insulin, an anabolic hormone.
- Type 1 diabetes (also known as insulin-dependent diabetes mellitus (IDDM) and juvenile diabetes mellitus) is a chronic illness characterized by the body’s inability to produce insulin due to the autoimmune destruction of the beta cells in the pancreas.
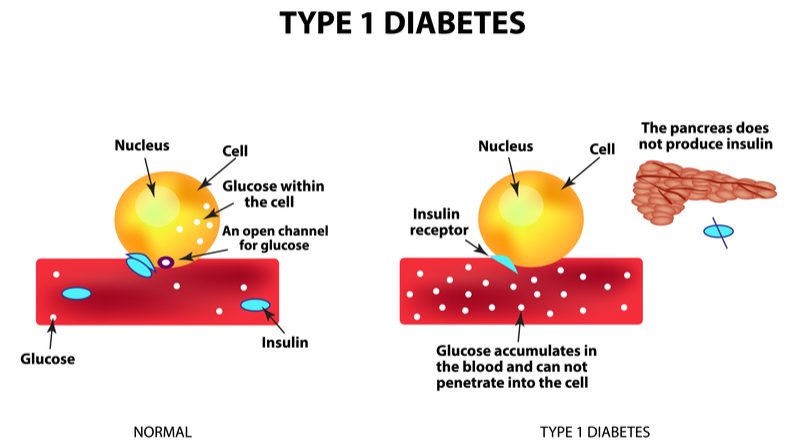
- Insulin is produced by the beta cells of the islets of Langerhans located in the pancreas, and the absence, destruction, or other loss of these cells results in type 1 diabetes (insulin-dependent diabetes mellitus [IDDM]).
- Diabetes mellitus is often considered an adult disease, but at least 5% of cases begin in childhood, usually at about 6 years of age or around the time of puberty.
Pathophysiology
A possible mechanism for the development of type 1 diabetes is as follows:
- Insulin is essential to process carbohydrates, fat, and protein; it reduces blood glucose levels by allowing glucose to enter muscle cells and by stimulating the conversion of glucose to glycogen (glycogenesis) as a carbohydrate store; it also inhibits the release of stored glucose from liver glycogen (glycogenolysis) and slows the breakdown of fat to triglycerides, free fatty acids, and ketones; it stimulates fat storage; additionally, insulin inhibits the breakdown of protein and fat for glucose production (gluconeogenesis) in the liver and kidneys.
- Hyperglycemia (ie, random blood glucose concentration of more than 200 mg/dL or 11 mmol/L) results when insulin deficiency leads to uninhibited gluconeogenesis and prevents the use and storage of circulating glucose.
- The kidneys cannot reabsorb the excess glucose load, causing glycosuria, osmotic diuresis, thirst, and dehydration; increased fat and protein breakdown leads to ketone production and weight loss.
- The brain depends on glucose as a fuel; as glucose levels drop below 65 mg/dL (3.2 mmol/L) counterregulatory hormones (eg, glucagon, cortisol, epinephrine) are released, and symptoms of hypoglycemia develop.
- The glucose level at which symptoms develop varies greatly from individual to individual (and from time to time in the same individual), depending in part on the duration of diabetes, the frequency of hypoglycemic episodes, the rate of fall of glycemia, and overall control.
Statistics and Incidences
The occurrence of diabetes mellitus type 1 in the United States and worldwide are as follows:
- The overall annual incidence of diabetes mellitus is about 24.3 cases per 100,000 person-years.
- Although most new diabetes cases are type 1 (approximately 15,000 annually), increasing numbers of older children are being diagnosed with type 2 diabetes mellitus, especially among minority groups (3700 annually).
- A study by Mayer-Davis et al indicated that between 2002 and 2012, the incidence of type 1 and type 2 diabetes mellitus saw a significant rise among youths in the United States; according to the report, after the figures were adjusted for age, sex, and race or ethnic group, the incidence of type 1 (in patients aged 0-19 years) and type 2 diabetes mellitus (in patients aged 10-19 years) during this period underwent a relative annual increase of 1.8% and 4.8%, respectively.
- Type 1 diabetes mellitus has wide geographic variation in incidence and prevalence.
- Annual incidence varies from 0.61 cases per 100,000 population in China to 41.4 cases per 100,000 population in Finland.
- Whites have the highest reported incidence, whereas Chinese individuals have the lowest.
- Type 1 diabetes mellitus is 1.5 times more likely to develop in American whites than in American blacks or Hispanics.
- Males are at greater risk in regions of high incidence, particularly older males, whose incidence rates often show seasonal variation; females appear to be at a greater risk in low-incidence regions.
- Onset in the first year of life, although unusual, can occur, so type 1 diabetes mellitus must be considered in any infant or toddler because these children have the greatest risk for mortality if the diagnosis is delayed.
Clinical Manifestations
The most easily recognized symptoms of type 1 diabetes mellitus (T1DM) are secondary to hyperglycemia, glycosuria, and DKA.
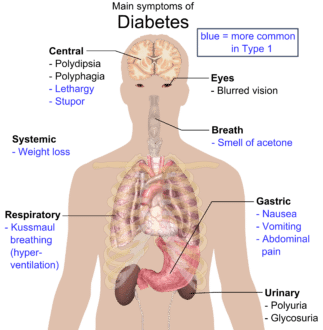
- Hyperglycemia. Hyperglycemia alone may not cause obvious symptoms, although some children report general malaise, headache, and weakness; children may also appear irritable and become ill-tempered.
- Glycosuria. This condition leads to increased urinary frequency and volume (eg, polyuria), which is particularly troublesome at night (eg, nocturia) and often leads to enuresis in a previously continent child.
- Polydipsia. Increased thirst, which may be insatiable, is secondary to the osmotic diuresis causing dehydration.
- Polyuria. There is a dramatic increase in urinary output, probably with enuresis.
- Polyphagia. There is an increase in hunger and food consumption.
- Weight loss. Insulin deficiency leads to uninhibited gluconeogenesis, causing breakdown of protein and fat; weight loss may be dramatic, although the child’s appetite usually remains good; failure to thrive and wasting may be the first symptoms noted in an infant or toddler and may precede frank hyperglycemia.
- Nonspecific malaise. Although this condition may be present before symptoms of hyperglycemia or as a separate symptom of hyperglycemia, it is often only retrospectively recognized.
- Diabetic ketoacidosis (DKA). DKA is characterized by drowsiness, dry skin, flushed cheeks, and cherry-red lips, acetone breath with a fruity smell, and Kussmaul breathing.
Assessment and Diagnostic Findings
Early detection and control are critical in postponing or minimizing later complications of diabetes.
- Fingerstick glucose test. Children with a family history of diabetes should be monitored for glucose using a fingerstick glucose test.
- Urine dipstick test. For ketones in the urine, the child should be tested using urine dipstick test.
- Fasting blood sugar (FBS). If the blood glucose level is elevated or ketonuria is present, a fasting blood sugar is performed; an FBS result of 200 mg/dl or higher almost certainly is diagnostic for diabetes when other signs are present.
- Lipid profile. Lipid profiles are usually abnormal at diagnosis because of increased circulating triglycerides caused by gluconeogenesis.
- Glycated hemoglobin. Glycosylated hemoglobin derivatives (HbA1a, HbA1b, HbA1c) are the result of a nonenzymatic reaction between glucose and hemoglobin; a strong correlation exists between average blood glucose concentrations over an 8- to 10-week period and the proportion of glycated hemoglobin.
- Microalbuminuria. Microalbuminuria is the first evidence of nephropathy; the exact definition varies slightly between nations, but an increased AER is commonly defined as a ratio of first morning-void urinary albumin levels to creatinine levels that exceed 10 mg/mmol, or as a timed, overnight AER of more than 20 mcg/min but less than 200 mcg/min.
Medical Management
Management of type 1 diabetes in children includes insulin therapy and a meal and exercise plan.
- Insulin therapy. Insulin therapy is an essential part of the treatment of diabetes in children; the dosage of insulin is adjusted according to blood glucose levels so that the levels are maintained near normal; many children are prescribed an insulin regimen given two times during the day: one before breakfast and the second before the evening meal.
- Diet. Current dietary management of diabetes emphasizes a healthy, balanced diet that is high in carbohydrates and fiber and low in fat.
- Activity. Type 1 diabetes mellitus requires no restrictions on activity; exercise has real benefits for a child with diabetes; current guidelines are increasingly sophisticated and allow children to compete at the highest levels in sports.
- Continuous glucose monitoring. The American Diabetes Association’s Standards of Medical Care in Diabetes-2018 recommend consideration of continuous glucose monitoring for children and adolescents with type 1 diabetes, whether they are using injections or continuous subcutaneous insulin infusion, to aid in glycemic control.
Pharmacologic Management
Insulin is always required to treat type 1 diabetes mellitus; these agents are used for the treatment of type 1 diabetes mellitus, as well as for type 2 diabetes mellitus that is unresponsive to treatment with diet and/or oral hypoglycemics.
- Insulin aspart. Rapid-acting insulin; insulin aspart is approved by the FDA for use in children aged >2 y with type 1 DM for SC daily injections and for SC continuous infusion by external insulin pump; however, it has not been studied in pediatric patients with type 2 DM; onset of action is 10-30 minutes, peak activity is 1-2 h, and duration of action is 3-6 h.
- Insulin glulisine. Rapid-acting insulin; the safety and effectiveness of SC injections of insulin glulisine have been established in pediatric patients (aged 4-17 y) with type 1 DM; however, it has not been studied in pediatric patients with type 2 DM; onset of action is 20-30 minutes, peak activity is 1 h, and duration of action is 5 h.
- Insulin lispro. Rapid-acting insulin; only lispro U-100 is approved by the FDA to improve glycemic control in children aged >3 y with type 1 DM; however, it has not been studied in children with type 2 DM; onset of action is 10-30 minutes, peak activity is 1-2 h, and duration of action is 2-4 h.
- Regular insulin. Short-acting insulin. Novolin R has been approved by the FDA to improve glycemic control in pediatric patients aged 2-18 y with type 1 DM; however, it has not been studied in pediatric patients with type 2 DM; Humulin R is indicated to improve glycemic control in pediatric patients with diabetes mellitus requiring more than 200 units of insulin per day; however, there are no well-controlled studies of use of concentrated Humulin R U-500 in children.
- Insulin NPH. Intermediate-acting insulin; it is indicated to improve glycemic control in pediatric patients with type 1 diabetes mellitus; onset of action is 3-4 h, peak effect is in 8-14 h, and usual duration of action is 16-24 h.
- Insulin glargine. Long-acting insulin; the safety and effectiveness of glargine U-100 have been established in pediatric patients (6-15 y) with type 1 DM; however, it has not been studied in pediatric patients with type 2 DM.
- Insulin detemir. Long-acting insulin. Insulin detemir is indicated for once- or twice-daily SC administration for the treatment of pediatric patients (aged 6-17 years) with type 1 DM; however, detemir has not been studied in pediatric patients with type 2 DM; onset of action is 3-4 h, peak activity is 6-8 h, and duration of action ranges from 5.7 h (low dose) to 23.2 h (high dose).
- Insulin degludec. Ultra-long-acting insulin; insulin degludec is approved by the FDA to improve glycemic control in pediatric patients aged >1 y with type 1 or type 2 DM; it usually takes 3-4 days for insulin degludec to reach steady state, peak plasma time is 9 h and the durations of action is at least 42 h; it is highly protein bound, and following SC, the protein-binding provides a depot effect.
Nursing Management
Nursing care for a patient with diabetes mellitus type 1 includes the following:
Nursing Assessment
Nursing assessment for patients with diabetes mellitus type 1 involves:
- History. When collecting data, ask the caregiver about the child’s symptoms leading up to the present illness; ask about the child’s appetite, weight loss or gain, evidence of polyuria or enuresis in a previously toilet-trained child, polydipsia, dehydration, irritability and fatigue; include the child in the interview and encourage him or her to contribute information.
- Physical exam. Measure the height and weight and examine the skin for evidence of dryness or slowly healing sores; note signs of hyperglycemia, record vital signs, and collect a urine specimen; perform a blood glucose level determination using a bedside glucose monitor.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses for diabetes mellitus type 1 are:
- Imbalanced nutrition: less than body requirements related to insufficient caloric intake to meet growth and development needs and the inability of the body to use nutrients.
- Risk for impaired skin integrity related to slow healing process and decreased circulation.
- Risk for infection related to elevated glucose levels.
- Deficient knowledge related to complications of hypoglycemia and hyperglycemia.
- Deficient knowledge related to appropriate exercise and activity.
Nursing Care Planning and Goals
Main Article 4 Diabetes Mellitus Type 1 (Juvenile Diabetes) Nursing Care Plans
The major nursing care planning goals for diabetes mellitus type 1 include:
- Maintaining adequate nutrition.
- Promoting skin integrity.
- Preventing infection.
- Regulating glucose levels.
- Learning to adjust to having a chronic disease.
- Learning about and managing hypoglycemia and hyperglycemia, insulin administration, and exercise needs for the child.
Nursing Interventions
Nursing interventions for diabetes mellitus type 1 are:
- Ensure adequate and appropriate nutrition. The child with diabetes needs a sound nutritional program that provides adequate nutrition for normal growth while maintaining the blood glucose at near normal levels; the food plan should be well balanced with foods that take into consideration the child’s food preferences, cultural customs, and lifestyle; if a particular meal is going to be late, the child should have a complex carbohydrate and protein snack.
- Prevent skin breakdown. Teach the caregiver and child to inspect the skin daily and promptly treat even small breaks in the skin; encourage daily bathing; teach the child and caregiver to dry the skin well after bathing, and give careful attention to any area where skin touches the skin, such as the groin, axilla, or other skin folds; emphasize good foot care.
- Prevent skin infection. Diabetic children may be more susceptible to urinary tract and upper respiratory infections; teach the child and caregiver to be alert for signs of urinary tract infection; instruct them to report signs of urinary tract or upper respiratory tract infections to the care provider; insulin should never be skipped during illness; fluids need to be increased.
- Regulate glucose levels. The child’s blood glucose levels must be monitored to maintain it within normal limits; determine the blood glucose level at least twice a day, before breakfast and before the evening meal; offer encouragement and support, helping the child to express fears and acknowledging that the fingerstick does hurt and it is acceptable to dislike it.
- Provide child and family teaching in the management of hypoglycemia and hyperglycemia. If the blood glucose is higher than 240mg/dl, the urine may be tested for ketones; be aware of the most likely times for an increase or decrease in the blood glucose level in relation to the insulin the child is receiving; and teach the child and family to recognize the signs of both hypoglycemia and hyperglycemia.
Evaluation
Goals are met as evidenced by:
The child/ caregiver:
- Maintained adequate nutrition.
- Promoted skin integrity.
- Prevented infection.
- Regulated glucose levels.
- Learned to adjust to having a chronic disease.
- Learned about managing hypoglycemia and hyperglycemia, insulin administration, and exercise needs for the child.
Documentation Guidelines
Documentation in a child with diabetes mellitus type 1 includes:
- Individual findings include factors affecting, interactions, the nature of social exchanges, and specifics of individual behavior.
- Intake and output.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.






























Leave a Comment