Insulin is a drug that is used to control glucose in patients with diabetes mellitus. It is the only parenteral antidiabetic agent available for exogenous replacement of low levels of insulin.
Insulin is the hormone produced by the pancreatic beta cells of the islets of Langerhans. It is released into circulation when the levels of glucose around the cells arise. Insulin circulates through the body and reacts with specific insulin receptor sites to stimulate the transport of glucose into cells to be used for energy (facilitated diffusion).
Originally prepared from pork and beef pancreas, virtually all insulin is prepared by recombinant DNA technology now. This is a purer form of insulin and is not associated with sensitivity problems that many patients developed with the animal products.
Disease Spotlight: Diabetes Mellitus
- Diabetes Mellitus (literally, “honey urine”) is a condition wherein there is a complex disturbance in the metabolism of carbohydrates, proteins, and fats. This alteration results in thickening of the layer below the endothelial lining of the blood vessels. This, in turn, causes narrowing, vessel remodeling, and decreased blood flow through vessels.
- Most frequent clinical signs include hyperglycemia (fasting blood sugar of >106 mg/dL) and the presence of sugar in the urine (glycosuria).
- Diabetes is classified into two: type 1 and type 2. Type 1 diabetes is common in younger people and is connected with cases of viral destruction of beta cells of the pancreas. On the other hand, type 2 is adult-onset and is associated with not enough insulin to maintain glucose control.
- Hyperglycemia (high blood sugar) results when there is an increase in glucose in the blood. Clinical signs and symptoms include fatigue, lethargy, irritation, glycosuria, polyphagia, polydipsia, and itchy skin (from the accumulation of wastes that liver cannot clear).
- Hypoglycemia is a blood glucose concentration lower than 40 mg/dL and can occur in many clinical situations like starvation and overtreatment of hyperglycemia. Manifestations include headache, paresthesias, hunger, and diaphoresis.
Therapeutic Action
The desired and beneficial action of insulin is:
- Insulin replaces endogenous insulin. It is the only parenteral antidiabetic agent available for exogenous replacement of low levels of insulin. It reacts with the receptors of the cells to facilitate transport of various metabolites and ions across cell membranes and stimulates the synthesis of glycogen from glucose, of fats from lipids, and of proteins from amino acids.
Indications
Insulin is indicated for the following medical conditions:
- Treatment of type 1 diabetes
- Treatment of type 2 diabetes when other agents have failed
- Short-term treatment of type 2 diabetes during periods of stress
- Management of diabetic ketoacidosis, hyperkalemia, and marked insulin resistance
Pharmacokinetics
Here are the characteristic interactions of insulin and the body in terms of absorption, distribution, metabolism, and excretion:
| Route | Onset | Peak | Duration |
|---|---|---|---|
| Regular | 30-60 min | 2-4 h | 6-12 h |
| NPH (Humulin N) | 1-1.5 h | 4-12 h | 24 h |
| Ultralente (Humulin Ultralente) | 4-8 h | 10-30 h | 20-36 h |
| Lispro (Humalog) | <15 min | 30-90 min | 2-5 h |
| Aspart (Novolog) | 10-20 min | 1-3 h | 3-5 h |
| Glargine (Lantus) | 60-70 min | None | 24 h |
| Glulisine (Apidra) | 2-5 min | 30-90 min | 2 h |
| Detemir (Levemir) | 1-2 h | 3-6 h | 5.7-23.3 h |
| Half-life (T1/2) | Metabolism | Excretion |
|---|---|---|
| Varies with each preparation | Cellular level | – |
Contraindications and Cautions
The following are contraindications and cautions for the use of insulin:
- No contraindications as it is a replacement hormone. However, close monitoring is needed among pregnant and lactating women to adjust the dose accordingly. It is the drug of choice for management of diabetes during pregnancy.
- Insulin does enter breast milk but it is destroyed in the GI tract and does not affect the nursing infant.
- Insulin-dependent mothers may have inhibited milk production because of insulin’s effects on fat and protein metabolism.
Adverse Effects
Use of insulin may result in these adverse effects:
- hypoglycemia and ketoacidosis
- local reactions at the injection site (lipodystrophy).
Interactions
The following are drug-drug interactions involved in the use of insulin:
- MAOIs, beta blockers, salicylates, alcohol. Increased glucose reduction
- Beta blockers. Blocking the SNS also blocks many of the signs and symptoms of hypoglycemia, hindering the patient’s ability to recognize problems.
- Various herbal therapies (juniper berries, ginseng, garlic, fenugreek, coriander, dandelion root, celery). Increased risk of developing hypoglycemia.
Nursing Considerations
Here are important nursing considerations when administering insulin:
Nursing Assessment
These are the important things the nurse should include in conducting assessment, history taking, and examination:
- Assess for contraindications or cautions (e.g. history of allergy, pregnancy, etc.) so that appropriate monitoring and dose adjustments can be completed.
- Perform a physical assessment to establish a baseline before beginning therapy.
- Assess skin lesions; orientation and reflexes; blood pressure, pulse, respiration and adventitious breath sounds which could indicate a response to high or low glucose levels and potential risk factors in giving insulin.
- Inspect skin areas that will be used for injection; note any areas that are bruised, thickened, or scarred, which could interfere with insulin absorption and alter anticipated response to insulin therapy.
- Obtain blood glucose levels as ordered to monitor response to insulin.
- Assess activity level, including amount and degree of exercise which can alter serum glucose levels and need for these drugs.
- Monitor the results of laboratory tests, including urinalysis, for evidence of glucosuria.
Nursing Diagnoses and Care Planning
Here are some of the nursing diagnoses that can be formulated in the use of this drug for therapy:
- Risk for unstable blood glucose related to ineffective dosing of antidiabetic agents
- Imbalanced nutrition: less than body requirements related to the use of insulin and underlying disease process
- Risk for infection related to glucose levels
Nursing Implementation with Rationale
These are vital nursing interventions done in patients who are taking insulin:
- Ensure that patient has dietary and exercise regimen and using good hygiene practices to improve the effectiveness of the insulin and decrease adverse effects of the disease.
- Monitor nutritional status to provide nutritional consultation as needed.
- Gently rotate the vial containing the agent and avoid vigorous shaking to ensure uniform suspension of insulin.
- Rotate injection sites to avoid damage to muscles and to prevent subcutaneous atrophy.
- Monitor response carefully to avoid adverse effects.
- Always verify the name of the insulin being given because each insulin has a different peak and duration, and the names can be confused.
- Use caution when mixing types of insulin; administer mixtures of regular and NPH insulins within 15 minutes after combining them to ensure appropriate suspension and therapeutic effect.
- Store insulin in a cool place away from direct sunlight to ensure effectiveness. Predrawn syringes are stable for 1 week if refrigerated.
- Monitor patient’s food intake and exercise and activities to ensure therapeutic effect and avoid hypoglycemia.
- Monitor patient’s sensory losses to incorporate his or her needs into safety issues, as well as potential problems in drawing up and administering insulin.
- Provide good skin care and foot care, to prevent the development of serious infections and changes in therapeutic insulin doses.
- Provide comfort measures to help patient cope with drug effects.
- Provide patient education about drug effects and warning signs to report to enhance patient knowledge and to promote compliance.
Evaluation
Here are aspects of care that should be evaluated to determine the effectiveness of drug therapy:
- Monitor patient response to therapy (stabilization of blood glucose levels).
- Monitor for adverse effects (hypoglycemia, ketoacidosis, injection-site irritation).
- Evaluate patient understanding on drug therapy by asking the patient to name the drug, its indication, and adverse effects to watch for.
- Monitor patient compliance to drug therapy.
Recommended Resources
Our recommended nursing pharmacology resources and books:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase which will help support us. Thank you! For more information, check out our privacy policy.
Pharm Phlash! Pharmacology Flash Cards #1 BEST SELLER!
Test-yourself review cards put critical clinical information for nearly 400 of the top generic medications at your fingertips. And, you can count on them for accuracy, because each card is based on content from Davis’s Drug Guide for Nurses. Increase your test scores in pharmacology class.

Focus on Pharmacology (8th Edition)
Focus on Nursing Pharmacology makes challenging concepts more approachable. Engaging learning features cultivate your clinical application, critical thinking and patient education capabilities. This updated 8th edition builds on your knowledge of physiology, chemistry and nursing fundamentals to help you conceptualize need-to-know information about each group of drugs.

Pharmacology Made Incredibly Easy (Incredibly Easy! Series®)
Nursing pharmacology guide offers step-by-step guidance so you can grasp the fundamentals in enjoyable Incredibly Easy style. This is the perfect supplement to class materials, offering solid preparation for NCLEX® as well as a handy refresher for experienced nurses. Colorfully illustrated chapters offer clear, concise descriptions of crucial nursing pharmacology concepts and procedures.
Lehne’s Pharmacology for Nursing Care (11th Edition)
The Eleventh Edition of Lehne’s Pharmacology for Nursing Care provides a thorough understanding of key drugs and their implications for nursing care. This text, written by renowned nursing educators, helps you comprehend and apply pharmacology principles. A clear and engaging writing style simplifies complex concepts, making even the most challenging pharmacology content enjoyable. We recommend this book if you want a comprehensive nursing pharmacology guide.

Nursing Drug Handbook
Nursing2023 Drug Handbook delivers evidence-based, nursing-focused drug monographs for nearly 3700 generic, brand-name, and combination drugs. With a tabbed, alphabetical organization and a “New Drugs” section, NDH2023 makes it easy to check drug facts on the spot.

Pharmacology and the Nursing Process
The 10th edition of Pharmacology and the Nursing Process offers practical, user-friendly pharmacology information. The photo atlas contains over 100 unique illustrations and photographs depicting drug administration techniques. Updated drug content reflects the most recent FDA drug approvals, withdrawals, and therapeutic uses.

Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, and Memory Aids for Nurses
The 6th edition of Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, & Memory Aids for Nurses incorporates illustrations and humor to make studying easier and more enjoyable. This unique pharmacology review can be utilized as a spiral-bound notebook or as individual flashcards, making it ideal for mobile study.

See Also
Here are other nursing pharmacology study guides:
- Nursing Pharmacology – Study Guide for Nurses
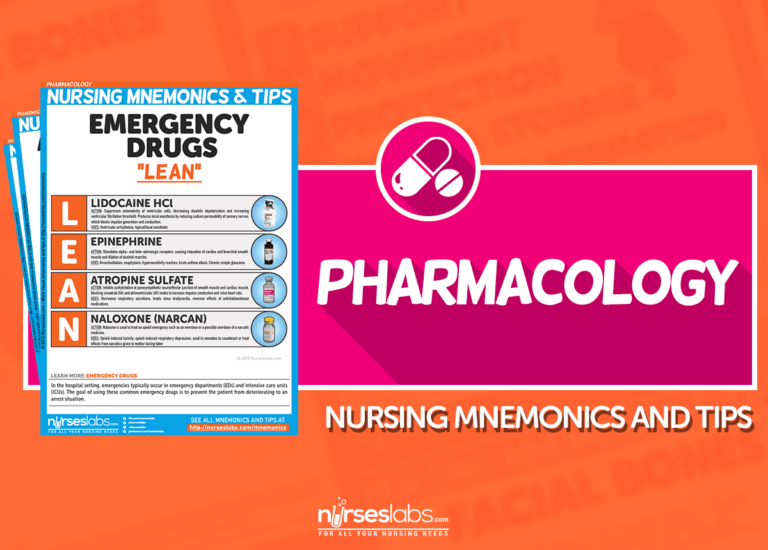
Our collection of topics related to nursing pharmacology - Pharmacology Nursing Mnemonics & Tips
These nursing mnemonics aim to simplify the concepts of pharmacology through the use of a simple, concise guide. - Generic Drug Name Stems Cheat Sheet
Learn about these generic drug name stems to help you make sense of drugs easier! - Common Drugs and Their Antidotes
A guide to drug antidotes that nurses should be familiar about. - IV Fluids and Solutions Guide & Cheat Sheet
Get to know the different types of intravenous solutions or IV fluids in this guide and cheat sheet. - Drug Dosage Calculations NCLEX Practice Questions (100+ Items)
Care to take the challenge? This quiz aims to help students and registered nurses alike grasp and master the concepts of medication calculation.
We have a pill for that…
Drug Guides NEW!
Individual drug guides and nursing considerations for the most common medications used in nursing pharmacology:
- Acetaminophen (Tylenol)
- Aspirin
- Atorvastatin (Lipitor)
- Enoxaparin (Lovenox)
- Furosemide (Lasix)
- Gabapentin
- Hydromorphone (Dilaudid)
- Lisinopril
- Metoprolol
- Morphine
Gastrointestinal System Drugs
Respiratory System Drugs
- Antihistamines
- Bronchodilators and Antiasthmatics
- Decongestants
- Expectorants and Mucolytics
- Inhaled Steroids
- Lung Surfactants
Endocrine System Drugs
- Adrenocortical Agents
- Antidiabetic Agents
- Glucose-Elevating Agents
- Hypothalamic Agents
- Insulin
- Parathyroid Agents: Bisphosphonates, Calcitonins
- Pituitary Drugs
- Sulfonylureas
- Thyroid Agents
Autonomic Nervous System Drugs
- Adrenergic Agonists (Sympathomimetics)
- Adrenergic Antagonists (Sympatholytics)
- Anticholinergics (Parasympatholytics)
- Cholinergic Agonists (Parasympathomimetics)
Immune System Drugs
Chemotherapeutic Agents
- Anthelmintics
- Anti-Infective Drugs
- Antibiotics
- Antifungals
- Antineoplastic Agents
- Antiprotozoal Drugs
- Antiviral Drugs
Reproductive System Drugs
Nervous System Drugs
- Antidepressants
- Antiparkinsonism Drugs
- Antiseizure Drugs
- Anxiolytics and Hypnotic Drugs
- General and Local Anesthetics
- Muscle Relaxants
- Narcotics, Narcotic Agonists, and Antimigraine Agents
- Neuromuscular Junction Blocking Agents
- Psychotherapeutic Drugs
Cardiovascular System Drugs
References and Sources
References and sources for this pharmacology guide for Insulin:
- Karch, A. M., & Karch. (2011). Focus on nursing pharmacology. Wolters Kluwer Health/Lippincott Williams & Wilkins. [Link]
- Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
- Lehne, R. A., Moore, L. A., Crosby, L. J., & Hamilton, D. B. (2004). Pharmacology for nursing care.
- Smeltzer, S. C., & Bare, B. G. (1992). Brunner & Suddarth’s textbook of medical-surgical nursing. Philadelphia: JB Lippincott.





![Furosemide Nursing Considerations and Patient Teaching [Drug Guide]](https://nurseslabs.com/wp-content/uploads/2023/07/Furosemide-480x360.jpg)
![Lisinopril Nursing Considerations and Patient Teaching [Drug Guide]](https://nurseslabs.com/wp-content/uploads/2023/03/Lisinopril-480x360.jpg)



Leave a Comment