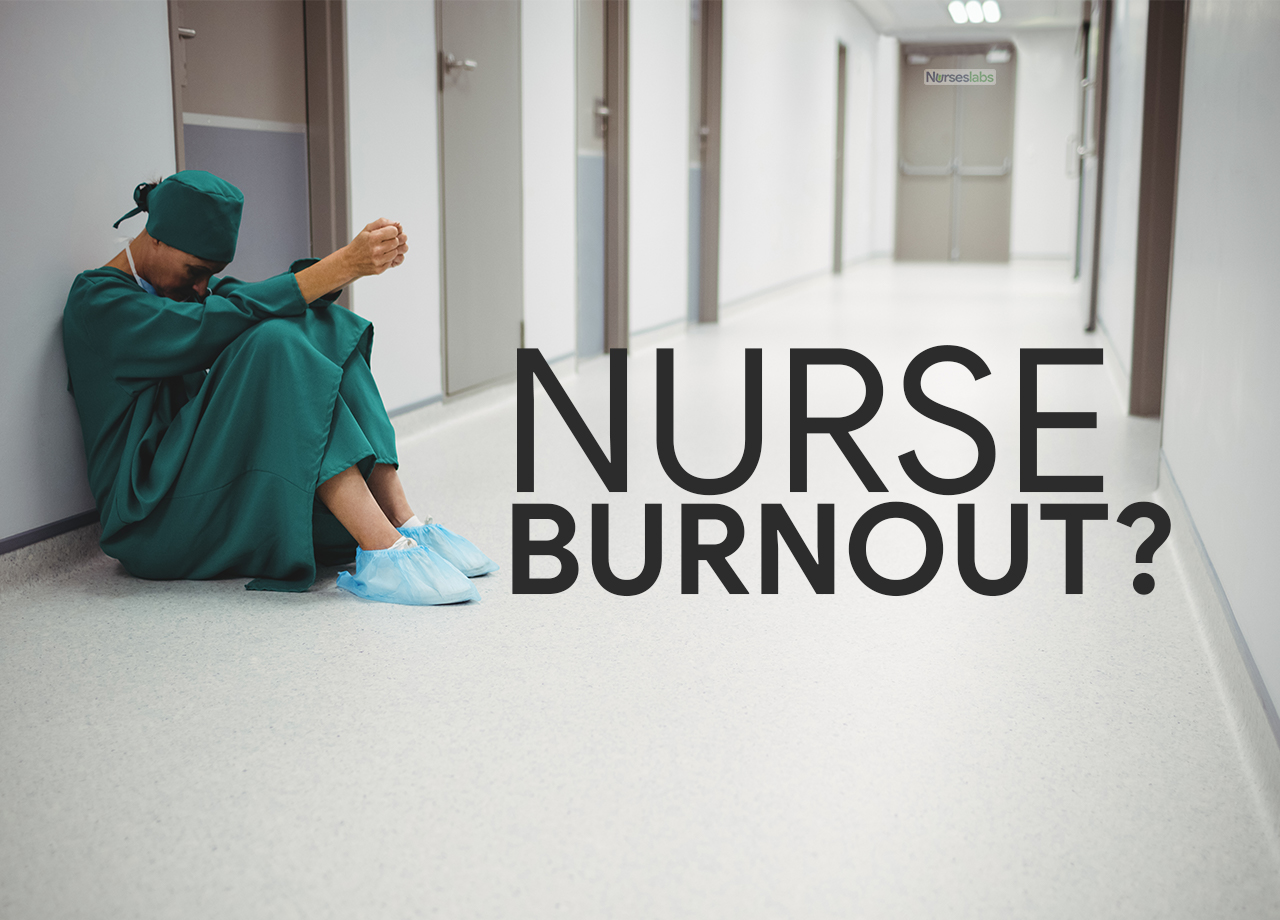
Burnout among nurses is a serious occupational syndrome resulting from unrelieved workplace stress. The World Health Organization recognizes burnout in the International Classification of Diseases (ICD-11) as an occupational phenomenon characterized by exhaustion, cynicism, and reduced professional efficacy. For frontline nurses, this isn’t just jargon – it’s the daily reality of feeling physically and emotionally depleted. This article aims to illuminate the consequences of nurse burnout and present evidence-based solutions at the personal, team, and system levels.
What is Burnout?
Burnout is a work‑related syndrome officially listed in the World Health Organization’s ICD‑11 as an occupational phenomenon, not a personal weakness. It shows up in three inter‑locking ways:
- Emotional exhaustion – feeling drained and unable to recover energy
- Depersonalization / cynicism – becoming detached, irritable, or “robotic” toward patients
- Reduced efficacy – doubting your skills and the value of your work
Among nurses, burnout is fueled by high‑acuity assignments, chronic understaffing, endless documentation, and the moral distress of wanting to give more than time or resources allow. Left unchecked, it harms nurses’ health, patients’ safety, and hospital finances.
Why Nurse Burnout Matters
Nursing burnout is more than just stress or fatigue – it is a state of sustained exhaustion that can erode one’s health, passion, and effectiveness at work. Over time, burnout leads to physical, emotional, and professional consequences for nurses.
Physically, chronic burnout can manifest as insomnia, headaches, increased illness, and hypertension. Emotionally, many nurses experience anxiety, depression, or compassion fatigue as their empathy runs dry. Professionally, burnout saps job satisfaction and engagement – at its worst, it drives nurses to quit the profession altogether. In one large U.S. survey, among nurses who left their job, 31.5% reported burnout as the reason for leaving. High levels of burnout have been reported worldwide; for example, a 2020 survey by the American Nurses Association (ANA) found almost 62% of nurses were experiencing burnout in the United States. The COVID-19 pandemic has only intensified this trend – global nursing organizations warn of a potential “mass exodus” of nurses, as 90% of national nursing associations cite heavy workloads, insufficient resources, stress and burnout as driving nurses away.
The stakes of nurse burnout extend beyond the individual nurse. Research has decisively linked nurse burnout to worse patient outcomes and safety issues. A recent systematic review and meta-analysis including 85 studies and 288,000 nurses found that burnout was associated with higher odds of medical errors, hospital-acquired infections, patient falls, and lower quality of care. Patients tend to be less satisfied with their care when their nurses are burned out, likely due to the breakdown of communication and compassion that burnout brings. In short, when nurses suffer, patients feel the impact.
“burnout was associated with higher odds of medical errors, hospital-acquired infections, patient falls, and lower quality of care.”
Furthermore, healthcare facilities pay a price: burnout fuels turnover, which can cost hospitals tens of thousands of dollars per nurse in recruitment and training. One analysis calculated that hospitals with nurse wellness programs spend about $11,600 per nurse per year on burnout-related turnover, versus $16,700 per nurse at hospitals without such support. Over time, preventing the burnout of just a few nurses can offset the entire cost of a well-being initiative. Burnout isn’t just a personal issue – it’s a patient safety and financial priority.
Multilevel Strategies to Combat Nurse Burnout
Addressing nurse burnout requires action on three levels: the individual nurse (personal level), the team or unit (interpersonal level), and the organization or system (institutional level). No single intervention is a cure-all; research suggests that a bundle of interventions is most effective. Below, we explore evidence-based strategies at each level, with practical tips for implementation. Whether you are a staff nurse looking to build resilience, a charge nurse cultivating a supportive team, or a healthcare leader reforming policies, these approaches can help rekindle purpose and protect well-being.
Personal-Level Interventions: Self-Care and Resilience for Nurses
At the individual level, self-care is not selfish – it’s survival. Remember, self-care is a skill to be learned and practiced. It’s not a one-time fix, but a continuous commitment. By prioritizing your own wellbeing, you increase your capacity to care for others. As the saying goes, you can’t pour from an empty cup. Nurses can take proactive steps to protect their own mental and physical health, building resilience against stress. Key personal strategies include:
1. Practicing Mindfulness and Relaxation
Mindfulness meditation, controlled breathing, and yoga can all curb stress and burnout: nurses who completed an eight-week mindfulness-based stress-reduction program showed lower burnout scores and improved emotional health afterward. Even micro-practices—a five-minute guided meditation before clock-in or a short yoga flow on a day off—help recharge the mind and build a buffer against daily pressures. Consider using a meditation app, joining a hospital-sponsored mindfulness class, or simply pausing for a few slow, focused breaths during breaks.
2. Healthy Routines and Emotional Hygiene
Maintaining healthy routines paired with deliberate “emotional hygiene” boosts a nurse’s resilience: prioritize sufficient sleep, balanced meals, and regular movement to raise stress tolerance, then offset psychological strain with restorative habits such as journaling about tough shifts, debriefing with a trusted friend, engaging in prayer or other spiritual practices, or immersing yourself in non-work hobbies. Protect this recovery time by drawing clear lines between job and home life—say, by silencing work email on days off—so your mind can fully rest and reset.
3. Finding Meaning and Purpose
When burnout blurs the purpose that drew you to nursing, deliberately reconnecting with that sense of meaning can counter cynicism: a qualitative study of critical-care clinicians identified “finding meaning in work”—recalling the positive impact on patients’ lives—as a key resilience habit, so revisit patient success stories, save thank-you notes from families, or note how adversity has fueled your professional growth; by framing nursing as a calling rather than just a job, daily stressors become easier to carry.
4. Personal Learning and Growth
Continual learning fortifies resilience: pursue continuing education on stress management or dive into specialties that spark your curiosity—communication-skills workshops, for instance, can lower burnout by strengthening workplace relationships. Mastering cognitive-behavioral strategies or sharper time-management techniques further equips you to handle demanding shifts, and if your hospital offers an employee assistance program or counseling, take advantage of it; talking with a therapist can provide fresh coping tools and keep small frustrations from snowballing into full burnout.
Team-Level Interventions: Fostering Support and Communication on the Unit
Burnout can’t be solved by individuals alone – the culture of the team or unit in which a nurse works plays a huge role in either exacerbating or alleviating stress. Frontline nurses and nurse managers together can cultivate a supportive environment through the following strategies:
1. Strengthen Teamwork and Communication
- A cohesive team can act as a buffer against burnout. When nurses feel they have each other’s backs, the work is less overwhelming. Interventions that improve teamwork have demonstrated positive impacts on burnout rates. Units might adopt team training programs (e.g., TeamSTEPPS) to enhance communication during shifts and handoffs.
- Regular brief huddles can be used to share workload concerns and voice if someone needs a hand. Likewise, encouraging open communication – where nurses can speak up about fatigue or safety issues without fear of stigma – is critical.
- Simple practices like a short debrief after challenging cases or “buddy checks” (pairing up nurses to informally monitor each other’s stress levels) promote a culture of mutual support.
2. Peer Support and Debriefing
- Nursing is emotionally intense, and having a safe outlet to process those emotions is essential. Hospitals have begun implementing peer support programs and moderated debriefing sessions (for example, after a code or traumatic incident) to help staff cope. These sessions allow nurses to share experiences, vent frustrations, and normalize the feelings of stress, thereby preventing isolation.
- Research on interventions in oncology and trauma units finds that social support and opportunities to discuss feelings can reduce compassion fatigue and burnout.
- If your workplace doesn’t have formal support groups or Schwartz Rounds, consider starting a informal “coffee chat” support circle among colleagues or mentoring pairs where a more experienced nurse checks in with a newer nurse. Sometimes just knowing you’re not alone in feeling burned out can reduce its power over you.
3. Positive Leadership and Recognition
- The role of nurse managers and team leaders is pivotal in burnout prevention. Supportive leadership can directly reduce burnout risk. Nurses who feel valued by their supervisors and included in decision-making report higher morale and lower burnout.
- Nurse leaders should strive for an open-door policy, actively solicit feedback on workloads, and intervene early when staff are struggling. Simple acts of recognition – like acknowledging a job well done in front of the team, or sending a thank-you note – help replenish a nurse’s sense of purpose.
- One study described “nurturing interpersonal connections” and feeling that “every team member’s contributions matter” as key factors that renew nurses’ inner strength. In practice, this could involve implementing a buddy system for new nurses, celebrating team successes, or organizing periodic team-building retreats (Lambert & Stewart, 2007, demonstrated a retreat could rejuvenate oncology nurses).
- Unit leaders should also guard against negative behaviors like bullying or incivility, which fast-track burnout; a zero-tolerance stance on lateral violence helps create psychological safety for the team.
4. Workload Sharing and Flexibility
- Within a unit, equitable distribution of workload and flexibility in scheduling can mitigate burnout. Cross-training staff so that nurses can rotate out of extremely high-stress assignments (like rotating between ICU and step-down, if trained for both) may provide mental breaks. If a particular shift is short-staffed or handling a heavy caseload, proactive adjustments (calling in float staff, redistributing patients) should be done rather than expecting nurses to just “push through”.
- Encouraging nurses to speak up when they are overloaded – and responding supportively when they do – is a team norm that can prevent errors and burnout.
- Participatory problem-solving, where staff are invited to propose solutions for unit challenges (such as how to streamline admissions or improve documentation flow), gives nurses a sense of control and can reduce the frustration that fuels burnout. In essence, a well-functioning team acts as a safety net: catching each other’s stress before it leads to burnout.
System-Level Interventions: Organizational and Policy Changes
Ultimately, burnout is not just an individual or team issue, but a system problem rooted in workplace conditions. Healthcare organizations and policymakers must take responsibility for creating environments where nurses can thrive. Evidence-based strategies at the organizational or system level include:
1. Adequate Staffing and Scheduling
- Safe staffing ratios and reasonable work hours are foundational to preventing burnout. Chronic short-staffing and forced overtime create a cycle of exhaustion and error. Research consistently shows that high nurse-to-patient ratios are associated with higher burnout levels and even increased patient mortality. Hospitals should abide by or exceed any mandated staffing regulations and use data-driven tools to predict and meet staffing needs.
- Moreover, offering flexible scheduling options can improve work-life balance – for instance, some nurses might prefer shorter shifts or self-scheduling options to accommodate their personal lives. Limiting excessive consecutive shifts and ensuring rest between shifts (to align with evidence on fatigue) should be standard policy.
- Administrators might consider “float pools” or incentive pay to cover for sick calls rather than pressuring an already stressed team to do more with less.
2. Investment in Nurse Wellbeing Programs
- Forward-thinking health systems are establishing comprehensive well-being initiatives to support their staff. This can range from on-site counseling services, stress reduction workshops, to providing quiet wellness spaces for staff to recharge. Importantly, such programs must be sustained and well-integrated into the workplace culture (and not just token yoga sessions during Nurses Week!). Successful examples include resilience training programs like the THRIVE© program for oncology nurses, which taught self-care strategies and significantly improved participants’ emotional health (Blackburn et al., 2020).
- Similarly, some hospitals have instituted “Schwartz Center Rounds” (interdisciplinary forums to discuss the emotional side of caregiving) or employed mental health professionals specifically to support staff (as was done in many hospitals during COVID-19 surges). The evidence suggests that hospitals do see a return on investment from these efforts – as one study noted, organizations with robust burnout prevention programs saved about $5,000 per nurse each year in turnover costs and had nurses who stayed in their jobs 20% longer. Healthcare leaders should champion these resources and encourage staff to utilize them without stigma.
3. Healthy Work Environment Standards
- Addressing burnout at the system level often means creating a workplace where well-being is baked into the culture. This can follow established frameworks like the American Association of Critical-Care Nurses (AACN) Healthy Work Environment standards, which include skilled communication, true collaboration, effective decision-making, adequate staffing, meaningful recognition, and authentic leadership. Policies and practices should align with these principles. For example, involving direct-care nurses in hospital committees and decision-making (shared governance) gives nurses a voice and increases job control, which correlates with lower burnout.
- Providing opportunities for professional development and career advancement can counter the stagnation that some nurses feel. Even physical environment enhancements – like break rooms with comfortable chairs, healthy snacks in vending machines, or safe spaces to rest – send a message that the organization cares about nurse welfare.
- At a higher level, nursing associations and policymakers are advocating for systemic changes such as enforceable nurse-to-patient ratio laws, limits on mandatory overtime, and funding for nurse mental health services. These broader policy efforts complement unit-level changes by ensuring baseline protections for all nurses.
4. Leadership Training and Accountability
- Often, the adage holds true: “people don’t quit jobs, they quit managers.” Health systems should ensure that those in supervisory roles – from charge nurses to executives – are trained in supportive leadership and held accountable for staff well-being metrics. Leadership development programs can train managers in emotional intelligence, conflict resolution, and burnout recognition. Some hospitals now include staff engagement and burnout levels as key performance indicators for units, meaning leaders must track and address these issues just as they would infection rates or budget targets.
- Creating a just culture where errors are treated as system issues rather than personal failures can also reduce the shame and stress that feed burnout.
- Ultimately, when leadership prioritizes a culture of safety, respect, and support, it empowers nurses to thrive. As the National Academy of Medicine (2019) report on clinician burnout emphasized, systemic commitment from the top is required to truly fix the workplace factors driving burnout.
Measuring Burnout: Validated Assessment Tools
Nurse leaders can pulse‑survey units every 6–12 months to spot hotspots and track progress. Individual nurses can self‑assess (CBI or ProQOL are free) and bring results to a wellness coach, EAP counselor, or supervisor to plan next steps. Re‑testing after interventions helps show what’s working.
| Tool | What It Measures | Format / Time | Cost & Access |
|---|---|---|---|
| Maslach Burnout Inventory (MBI) | Emotional exhaustion, depersonalization, reduced personal accomplishment | 22 items; Likert scale; ≈ 10 min | Paid license (≈ US $15–20 per user) |
| Copenhagen Burnout Inventory (CBI) | Personal, work‑related, and client‑related burnout | 19 items; Likert; ≈ 7 min | Free, open‑access (Creative Commons) |
| Professional Quality of Life Scale (ProQOL v5) | Compassion satisfaction, burnout, secondary traumatic stress | 30 items; 5‑point Likert; ≈ 10 min | Free, open‑access |
Combating Burnout
Nurse burnout is a complex, multi-faceted problem – but it is not a hopeless one. Physical exhaustion, emotional turmoil, and the desire to leave the profession are red flags that we must not ignore. The well-being of nurses is inextricably linked to the quality and safety of patient care. Therefore, tackling burnout is not only about compassion for caregivers; it is about safeguarding our healthcare system’s capacity to deliver excellent care.
For the individual nurse reading this: your health and happiness matter. Paying attention to your own burnout warning signs – and taking proactive steps like those outlined above – is an act of professionalism. It enables you to continue doing the work you love with the empathy and excellence your patients deserve.
your health and happiness matter.
For nursing teams and managers: recognize that no nurse is an island. Creating a supportive team climate and watching out for each other can turn the tide on burnout in your unit. Small acts of kindness and understanding, combined with structured team practices, make a tangible difference in morale.
As for organizational leaders and policymakers: it’s time to treat nurse burnout as the public health crisis that it is. This means committing resources and policy changes to fix systemic issues such as understaffing, punishing workloads, and lack of support. The solutions may require investment, but the payoff – in retained staff, reduced errors, and human sustainability – is well worth it.
In the end, preventing and recovering from nurse burnout is a shared responsibility. Just as quality patient care relies on teamwork, so does nurse well-being. By combining personal resilience-building with compassionate team cultures and enlightened leadership, we can begin to turn burnout into a thing of the past. Nurses have an astounding capacity for dedication – with the right support, that dedication can burn bright without burning out.
Reference
- Alexander, G. K., Rollins, K., Walker, D., Wong, L., & Pennings, J. (2015). Yoga for self-care and burnout prevention among nurses. Workplace Health & Safety, 63(10), 462–470. https://doi.org/10.1177/2165079915596102
- Aryankhesal, A., Mohammadibakhsh, R., Hamidi, Y., Alidoost, S., Behzadifar, M., Sohrabi, R., & Farhadi, Z. (2019). Interventions on reducing burnout in physicians and nurses: A systematic review. Medical Journal of the Islamic Republic of Iran, 33, 77. https://doi.org/10.34171/mjiri.33.77
- Blackburn, L. M., Thompson, K., Frankenfield, R., Harding, A., & Lindsey, A. (2020). The THRIVE© program: Building oncology nurse resilience through self-care strategies. Oncology Nursing Forum, 47(1), E25–E34. https://doi.org/10.1188/20.ONF.E25-E34
- International Council of Nurses (ICN). (2021). The global nursing shortage and nurse retention – ICN policy brief. Geneva: ICN. Retrieved from https://www.icn.ch/system/files/documents/2021-07/ICN%20Policy%20Brief_Nurse%20Shortage%20and%20Retention_0.pdf
- Li, L. Z., Yang, P., Singer, S. J., Pfeffer, J., Mathur, M. B., & Shanafelt, T. D. (2024). Nurse burnout and patient safety, satisfaction, and quality of care: A systematic review and meta-analysis. JAMA Network Open, 7(11), e2443059. https://doi.org/10.1001/jamanetworkopen.2024.43059
- Maslach, C. (1998). A multidimensional theory of burnout. In C. L. Cooper (Ed.), Theories of Organizational Stress (pp. 68–85). Oxford University Press. (No DOI)
- Muir, J. K., Wanchek, T. N., Lobo, J. M., & Keim-Malpass, J. (2022). Evaluating the costs of nurse burnout-attributed turnover: A Markov modeling approach. Journal of Patient Safety, 18(4), 358–364. https://doi.org/10.1097/PTS.0000000000000942
- Shah, M. K., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469. https://doi.org/10.1001/jamanetworkopen.2020.36469
- Suñer-Soler, R., Grau-Martín, A., Flichtentrei, D., Prats, M., Braga, F., Font-Mayolas, S., & Gras, M. E. (2014). The consequences of burnout syndrome among healthcare professionals in Spain and Spanish-speaking Latin American countries. Burnout Research, 1(2), 82–89. https://doi.org/10.1016/j.burn.2014.07.004
- World Health Organization (WHO). (2019, May 28). Burn-out an “occupational phenomenon”: International Classification of Diseases. Retrieved from https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
- Wei, H., Kifner, H., Dawes, M. E., Wei, T. L., & Boyd, J. M. (2020). Self-care strategies to combat burnout among pediatric critical care nurses and physicians. Critical Care Nurse, 40(2), 44–53. https://doi.org/10.4037/ccn2020621
- Westermann, C., Kozak, A., Harling, M., & Nienhaus, A. (2014). Burnout intervention studies for inpatient elderly care nursing staff: Systematic literature review. International Journal of Nursing Studies, 51(1), 63–71. https://doi.org/10.1016/j.ijnurstu.2012.12.001








Leave a Comment