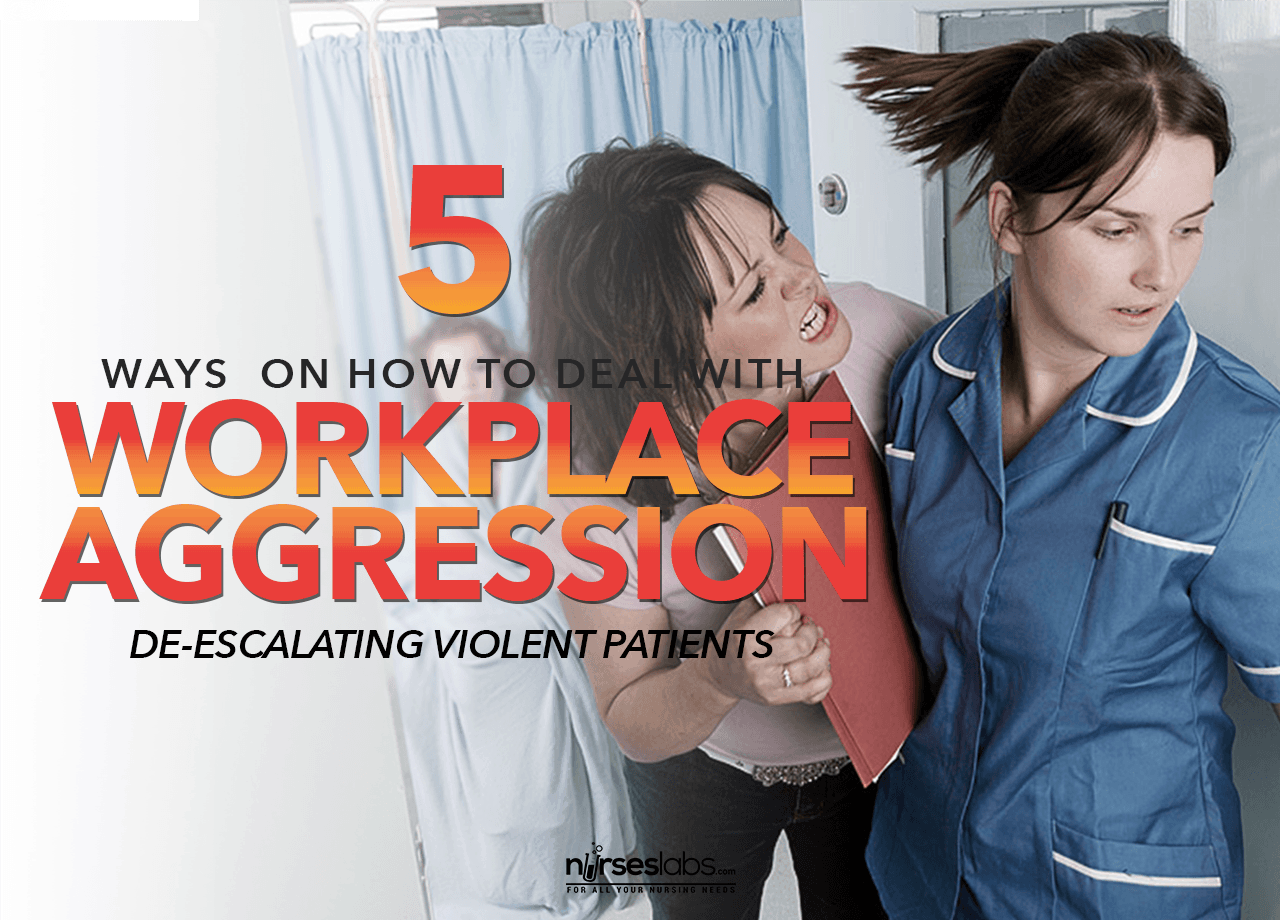
Nurses are the most likely to be first in line when patients or their relatives become aggressive and possibly violent. Because anger is usually an expression of loss of control over one’s circumstances, potentially violent behavior happens mostly where patients are mentally unstable and in ER Departments where the family finds itself in crisis as well as being in a strange environment.
Every nurse should develop skills in verbal de-escalation, from both a caring perspective and for their own protection. When in the firing line there is not always time to call a trained responder. A 5-minute de-escalation is also far preferable to the use of physical restraint, where staff members are also at greater risk of being injured in the process.
Statistics provided by the US Department of Labor showed that 45% of workplace assaults leading to loss of work days were against nurses. Workplace violence is seen by the American Nurses’ Association as the most significant occupational hazard faced by nurses and an issue that should be addressed as a priority with adequate workplace policy as well as skills training for all nurses.

When faced with potential violence the instinctive human response is fight or flight, but neither of these two actions is suitable for the healthcare setting where nurses have a duty to care. Using the following techniques to deal with aggressive behavior can usually turn the situation around and reduce the need for a crisis team. Learning and practicing these skills will also give you self-confidence in handling any crisis.
Keep in mind that whatever you do might successfully de-escalate the situation, make it worse or have no effect on the person’s behavior. Be aware of the person’s reaction all the time – if he seems to be calming down, carry on in the same way but try something else if the situation appears to be getting worse. Physical restraint and drugs should only be used as a last resort if the aggressive person poses a danger to himself or others.
1. Find a safe environment
If possible, try to move the person away from other people to an environment where he or she can feel safe and which is also safe for you.
2. Position yourself correctly
Stand in a position of safety – usually between the person and the doorway, but not directly in front of the door so that the individual also has an escape route. Our first reaction as nurses is to move towards patients, offering a comforting touch. However, respect for personal space is vital when dealing with aggressive behavior as the invasion of this space can increase the level of anxiety. Stay at least two arms’ lengths away from the person. This also puts you out of reach of assault by either hitting or kicking and gives you space to evade or ward off an actual attack.
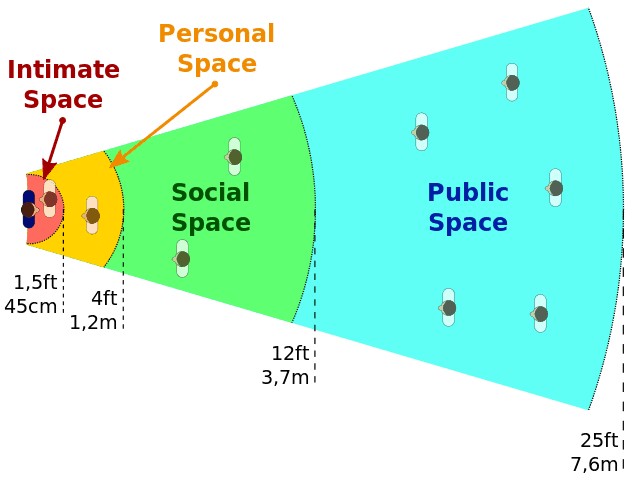
Avoid facing of the person in a full frontal position because this is an aggressive stance and might be interpreted as confrontation. Stand slightly to the side and at an angle. Adopt a relaxed posture, arms at your sides with hands open and facing the person.
3. Be calm and respectful

The aggressive person who has lost control over rational thought is more tuned it to non-verbal cues than to what you might be saying. Even though, on the inside, you might feel terrified or ready to lash out you must maintain a calm appearance in your gestures, facial expressions, movements and tone of voice. Through eye contact and non-threatening body language demonstrate that you are giving the person your full attention and are interested in his or her problem. Here’s also a list if things you shouldn’t say to your patients.
4. Use principles of therapeutic communication
This is the time to consciously and actively put into practice everything you have learned about therapeutic communication.
Listen intently to what the person is saying, including interpreting what the real reason for the individual’s behavior might be. Listen to the feelings behind what the person is actually complaining about. A relative might lash out against staff because of underlying fear and concern for a loved one. If possible, allow verbal venting as this is often when the actual issue becomes evident.
Validate the person’s feelings by demonstrating through your response that you understand how he feels. “I understand that you are really frustrated that your wife has not been attended to yet and are concerned that her condition might get worse.” Show non-judgmental acceptance and respect. Although you might believe that the person’s feelings are not valid, they are very real to him. Allow silences because this will reduce confrontation to a lower level as well as enable the person to think about his or her response.
Reflect the communication by summarizing and expressing what you believe the person has said and then allowing him to confirm or explain further. This shows that you want to understand the situation so that the problem can be addressed.
Ignore challenges against the health care institution or you personally, such as “Who do you think you are to tell me that”. Responding defensively to challenges will only lead to arguments. Lead the conversation back to the central issue at hand.
Once the situation has been defused and the person is calmer, rational communication will be possible, and the next step would be to try and find an acceptable resolution to the problem. Set clear limits, provide necessary information concisely and, where possible, offer choices which will give the person some sense of control over the situation. “You can’t be in the cubicle while the staff is examining your boyfriend but you can join him as soon as we are finished. That will be in about half-an-hour. You can sit in the waiting room and have a cup of coffee from the dispenser or maybe you would like to get some coffee and something to eat in the hospital’s coffee bar.”
5. Practice the skills
Using these principles effectively to de-escalate aggressive behavior and preventing violence when you are in the middle of a crisis is a skill. As with any skill, practice is necessary to gain competence and confidence. You could practice role-playing with friends and colleagues and even try to use the steps consciously during confrontations in your daily life. De-escalation techniques can be suggested as a topic for in-service training using role play, preferably with videotaping and feedback, as a teaching method. There are also some companies that offer de-escalation training as well as many YouTube demonstration video.

































Leave a Comment