Ida Jean Orlando was a nurse theorist who developed the Deliberative Nursing Process Theory. Learn about Ida Jean Orlando’s biography, major concepts of her nursing theory, and its application to nursing in this study guide.
Biography of Ida Jean Orlando
Ida Jean Orlando-Pelletier (August 12, 1926 – November 28, 2007) was an internationally known psychiatric health nurse, theorist, and researcher who developed the “Deliberative Nursing Process Theory.” Her theory allows nurses to create an effective nursing care plan that can also be easily adapted when and if any complications arise with the patient.
Early Life
Ida Jean Orlando was a first-generation Irish American born on August 12, 1926. She dedicated her life to studying nursing and graduated in 1947 and received a Bachelor of Science degree in public health nursing in 1951. In 1954, she completed her Master of Arts in Mental Health consultation. While studying, she also worked intermittently and sometimes concurrently as a staff nurse in OB, MS, ER, as a general hospital supervisor, and as an assistant director and a teacher of several courses. And in 1961, she was married to Robert Pelletier and lived in the Boston area.
Education

Being a respectable and credible role-model, Orlando was well educated with many advanced nursing degrees.
In 1947, she received a nursing diploma from the Flower Fifth Avenue Hospital School of Nursing in New York. In 1951, she received a Bachelor of Science degree in public health nursing from St. John’s University in Brooklyn, New York. And in 1954, Orlando received her Master of Arts degree in mental health consultation from Teachers College, Columbia University.
Career and Appointments
Ida Jean Orlando had a diverse career, working as a practitioner, consultant, researcher, and educator in nursing. Orlando devoted her life to mental health and psychiatric nursing, working as a clinical nurse and researcher.
After receiving her master’s degree in 1954, Orlando went to the Yale University School of Nursing in New Haven, Connecticut as an associate professor of mental health and psychiatric nursing for eight years. She was awarded a federal grant and became a research associate and the principal project investigator of a National Institute of Mental health Institute of the United States Public Health Service’s grant entitled “Integration of Mental Health Concepts in a Basic Curriculum.” The project sought to identify those factors relevant to integrating psychiatric-mental health principles into the nursing curriculum.

During 1958-1961, Orlando, as an associate professor and the director of the graduate program in mental health and psychiatric nursing at Yale University, used her proposed conceptual nursing model as the foundation for the program’s curriculum. From 1962-1972, Orlando served as a clinical nurse consultant at Mclean Hospital in Belmont, Massachusetts. In this position, she studied the interactions of nurses with clients, other nurses, and other staff members and how these interactions affected the nurse’s help to clients. Orlando convinced the administration that an educational program for nurses was needed, whereupon Mclean Hospital initiated an educational program based on her nursing model.

From 1972 to 1984, she also served on the Harvard Community Health Plan board in Boston, Massachusetts.
In 1981, Orlando became an educator at Boston University School of Nursing and held administrative positions from 1984 to 1987 at Metropolitan State Hospital in Waltham, Massachusetts. In September 1987, she became the Assistant Director of Nursing for Education and Research at the said institution. She was also a project consultant for the Mental Health Project for Associate Degree Faculties created by the New England Board of Higher Education. Finally, in 1992, Orlando retired and received the Nursing Living Legend award from the Massachusetts Registered Nurse Association.
Deliberative Nursing Process Theory
Ida Jean Orlando developed her theory from a study conducted at the Yale University School of Nursing, integrating mental health concepts into a basic nursing curriculum. She proposed that “patients have their own meanings and interpretations of situations and therefore nurses must validate their inferences and analyses with patients before concluding.”
The theory was published in The Dynamic Nurse-Patient Relationship: Function, Process, and Principles (NLN Classics in Nursing Theory) in 1961. Her book proposed a contribution to concern about the nurse-patient relationship, the nurse’s professional role and identity, and the knowledge development distinct to nursing.
Orlando’s nursing theory stresses the reciprocal relationship between patient and nurse. What the nurse and the patient say and do affects them both. She views nursing’s professional function as finding out and meeting the patient’s immediate need for help.

She also described her model as revolving around the following five major interrelated concepts: the function of professional nursing, presenting behavior, immediate reaction, nursing process discipline, and improvement. The function of professional nursing is the organizing principle. Presenting behavior is the patient’s problematic situation. The immediate reaction is the internal response. The nursing process discipline is the investigation into the patient’s needs. And lastly, improvement is the resolution to the patient’s situation.
The Deliberative Nursing Process has five stages: assessment, diagnosis, planning, implementation, and evaluation. Nurses use the standard nursing process in Orlando’s Nursing Process Discipline Theory to produce positive outcomes or patient improvement. Orlando’s key focus was the definition of the function of nursing. The model provides a framework for nursing, but her theory does not exclude nurses from using other nursing theories while caring for patients.
Ida Jean Orlando’s nursing theory is discussed further below.
Works
After working as a researcher, she wrote a book on her findings from Yale, entitled “The Dynamic Nurse-Patient Relationship: Function, Process, and Principles.” Her book was published in 1961. A year later, she also continued her research studies published her second book, “The Discipline and Teaching of Nursing Process,” in 1972.
Awards and Honors
Ida Jean Orlando retired from nursing in 1992. After becoming well-educated, researching over 2,000 nurse-patient interactions, and coming up with a theory that changed nursing, she was recognized as a “Nursing Living Legend” by the Massachusetts Registered Nurse Association.
Death
Ida Jean Orlando died on November 28, 2007, at the age of 81.
Orlando’s Deliberative Nursing Process Theory
One important thing that nurses do is converse with the patients and let them know what the plan of care will be. However, regardless of how well thought out a nursing care plan is for a patient, unexpected problems to the patient’s recovery may arise at any time. With these, the nurse’s job is to know how to deal with those problems so the patient can continue to get back and reclaim his or her well-being. Ida Jean Orlando developed her Deliberative Nursing Process that allows nurses to formulate an effective nursing care plan that can also be easily adapted when and if any complexity comes up with the patient.
Ida Jean Orlando’s nursing theory stresses the reciprocal relationship between patient and nurse. It emphasizes the critical importance of the patient’s participation in the nursing process. Orlando also considered nursing as a distinct profession. He separated it from medicine, where nurses determining nursing action rather than being prompted by physician’s orders, organizational needs, and past personal experiences. She believed that the physician’s orders are for patients and not for nurses.
She proposed that “patients have their own meanings and interpretations of situations and therefore nurses must validate their inferences and analyses with patients before concluding.”
Goal
Ida Jean Orlando’s goal is to develop a theory of effective nursing practice. The theory explains that the nurse’s role is to find out and meet the patient’s immediate needs for help. According to the theory, all patient behavior can be a cry for help. Through these, the nurse’s job is to determine the nature of the patient’s distress and provide the help he or she needs.
Assumptions
Ida Jean Orlando’s model of nursing makes the following assumptions:
- When patients cannot cope with their needs on their own, they become distressed by feelings of helplessness.
- In its professional character, nursing adds to the distress of the patient.
- Patients are unique and individual in how they respond.
- Nursing offers mothering and nursing analogous to an adult who mothers and nurtures a child.
- The practice of nursing deals with people, the environment, and health.
- Patients need help communicating their needs; they are uncomfortable and ambivalent about their dependency needs.
- People can be secretive or explicit about their needs, perceptions, thoughts, and feelings.
- The nurse-patient situation is dynamic; actions and reactions are influenced by both the nurse and the patient.
- People attach meanings to situations and actions that aren’t apparent to others.
- Patients enter into nursing care through medicine.
- The patient cannot state the nature and meaning of his or her distress without the nurse’s help or him or her first having established a helpful relationship with the patient.
- Any observation shared and observed with the patient is immediately helpful in ascertaining and meeting his or her need or finding out that he or she is not in need at that time.
- Nurses are concerned with the needs the patient is unable to meet on his or her own.
Major Concepts
The nursing metaparadigm consists of four concepts: person, environment, health, and nursing. Of the four concepts, Ida Jean Orlando only included three in her theory of Nursing Process Discipline: person, health, and nursing.
Human Being
Orlando uses the concept of human as she emphasizes individuality and the dynamic nature of the nurse-patient relationship. For her, humans in need are the focus of nursing practice.
Health
In Orlando’s theory, health is replaced by a sense of helplessness as the initiator of a necessity for nursing. She stated that nursing deals with individuals who require help.
Environment
Orlando completely disregarded the environment in her theory, only focusing on the patient’s immediate need, chiefly the relationship and actions between the nurse and the patient (only an individual in her theory; no families or groups were mentioned). The effect that the environment could have on the patient was never mentioned in Orlando’s theory.
Nursing
Orlando speaks of nursing as unique and independent in its concerns for an individual’s need for help in an immediate situation. The efforts to meet the individual’s need for help are carried out in an interactive situation and in a disciplined manner that requires proper training.
Subconcepts
Ida Jean Orlando described her model as revolving around the following five major interrelated concepts: the function of professional nursing, presenting behavior, immediate reaction, nursing process discipline, and improvement.
The function of Professional Nursing
The function of professional nursing is the organizing principle. This means finding out and meeting the patient’s immediate needs for help. According to Orlando, nursing is responsive to individuals who suffer or who anticipate a sense of helplessness. It is focused on the process of care in an immediate experience. It is concerned with providing direct assistance to a patient in whatever setting they are found to avoid, relieve, diminishing, or curing the patient’s sense of helplessness. The Nursing Process Discipline Theory labels the purpose of nursing to supply the help a patient needs for their needs to be met. If the patient has an immediate need for help, and the nurse discovers and meets that need, the purpose of nursing has been achieved.
Presenting Behavior
Presenting behavior is the patient’s problematic situation. Through the presenting behavior, the nurse finds the patient’s immediate need for help. To do this, the nurse must first recognize the situation as problematic. Regardless of how the presenting behavior appears, it may represent a cry for help from the patient. The patient’s presenting behavior, which is considered the stimulus, causes an automatic internal response in the nurse, which in turn causes a response in the patient.
Distress
The patient’s behavior reflects distress when the patient experiences a need that he cannot resolve, a sense of helplessness occurs.
Immediate Reaction
The immediate reaction is the internal response. The patient perceives objects with his or her five senses. These perceptions stimulate automatic thought, and each thought stimulates an automatic feeling, causing the patient to act. These three items are the patient’s immediate response. The immediate response reflects how the nurse experiences his or her participation in the nurse-patient relationship.
Nurse Reaction
The patient’s behavior stimulated a nurse’s reaction, which marks the nursing process discipline’s beginning.
Nurse’s Action
When the nurse acts, an action process transpires. This action process by the nurse in a nurse-patient contact is called the nursing process. The nurse’s action may be automatic or deliberative.
Automatic Nursing Actions are nursing actions decided upon for reasons other than the patient’s immediate need.
Deliberative Nursing Actions are actions decided upon after ascertaining a need and then meeting this need.
The following list identifies the criteria for deliberative actions:
- Deliberative actions result from the correct identification of patient needs by validating the nurse’s reaction to patient behavior.
- The nurse explores the meaning of the action with the patient and its relevance to meeting his need.
- The nurse validates the action’s effectiveness immediately after completing it.
- The nurse is free of stimuli unrelated to the patient’s need when she acts.
Nursing Process Discipline
The nursing process discipline is the investigation into the patient’s needs. Any observation shared and explored with the patient is immediately useful in ascertaining and meeting his or her need or finding out they have no needs at that time. The nurse cannot assume that any aspect of his or her reaction to the patient is correct, helpful, or appropriate until he or she checks its validity by exploring it with the patient. The nurse initiates this exploration to determine how the patient is affected by what they say and do. Automatic reactions are ineffective because the nurse’s action is determined for reasons other than the meaning of the patient’s behavior or the patient’s immediate need for help. When the nurse doesn’t explore the patient’s reaction with him or her, it is reasonably certain that effective communication between nurse and patient stops.
The nurse decides on appropriate action to resolve the need in cooperation with the patient. This action is evaluated after it is carried out. If the patient’s behavior improves, the action was successful, and the process is completed. If there is no change or the behavior gets worse, the process recycles with new efforts to clarify the patient’s behavior or the appropriate nursing action.
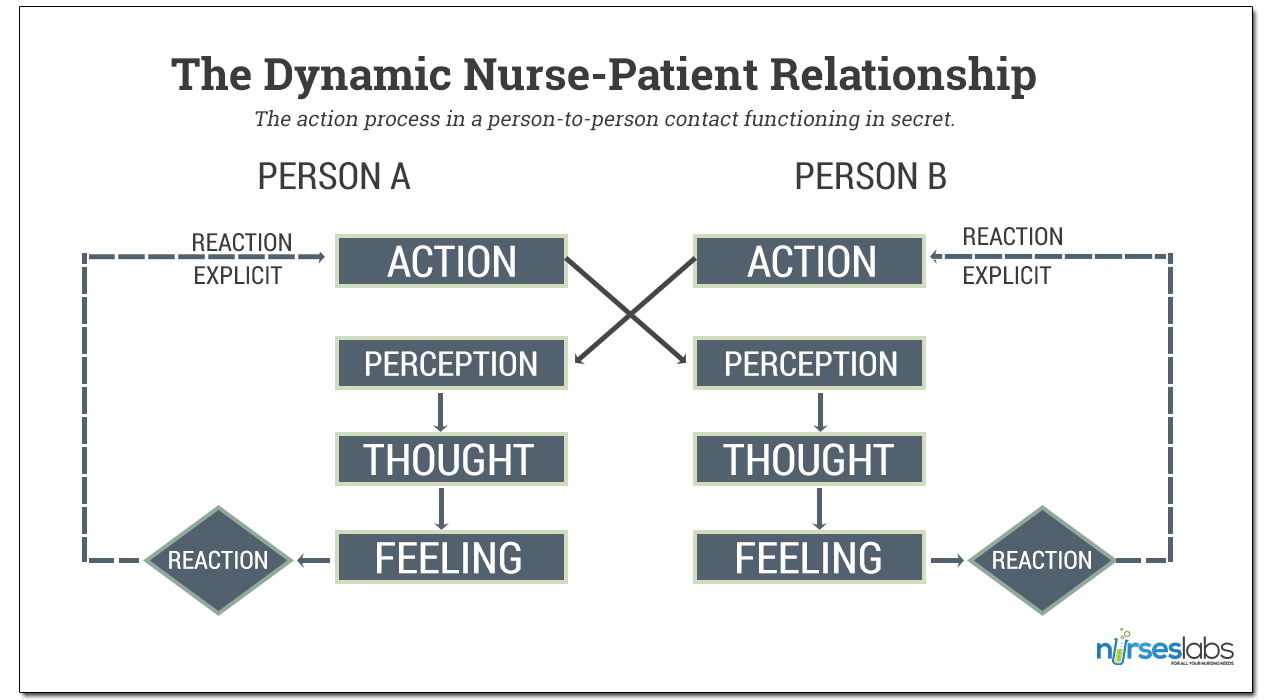
The action process in a person-to-person contact functioning in secret. The perceptions, thoughts, and feelings of each individual are not directly available to the other individual’s perception through the observable action.
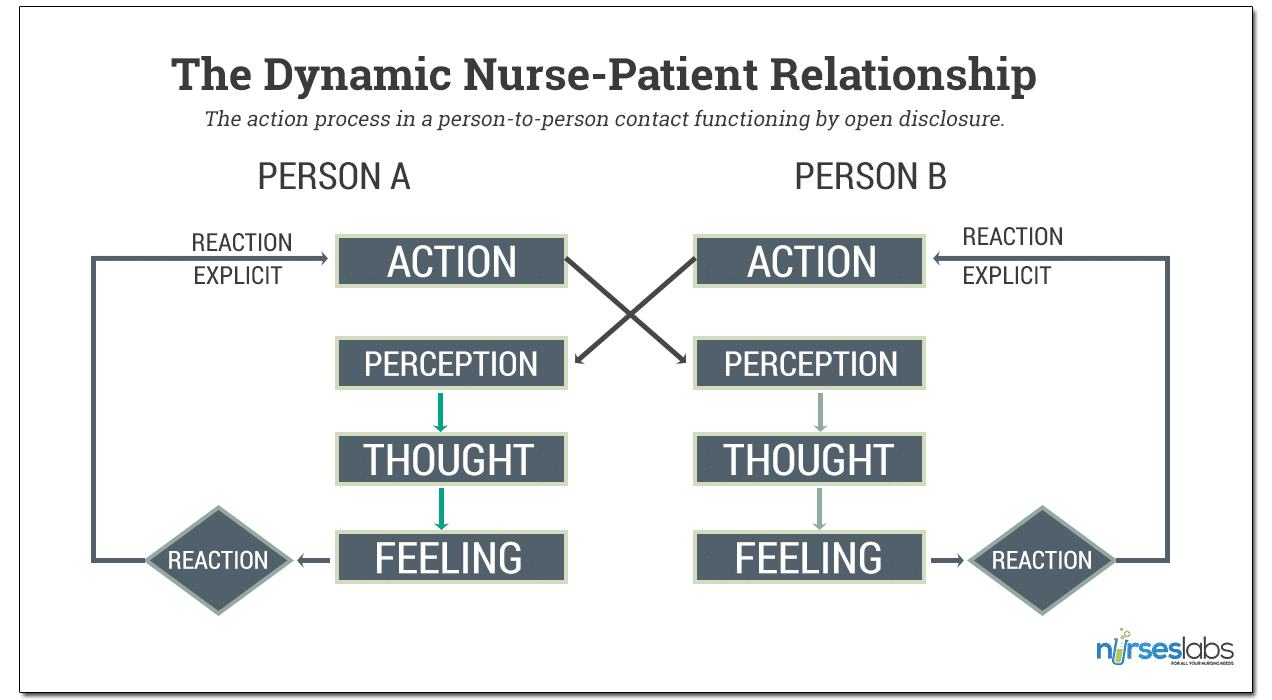
The action process in a person-to-person contact functioning by open disclosure. The perceptions, thoughts, and feelings of each individual are directly available to the other individual’s perception through the observable action.
Improvement
Improvement is the resolution to the patient’s situation. In the resolution, the nurse’s actions are not evaluated. Instead, the result of his or her actions is evaluated to determine whether their actions served to help the patient communicate his or her need for help and how it was met. In each contact, the nurse repeats learning how he or she can help the patient. The nurse’s own individuality and that of the patient require going through this each time the nurse is called upon to render service to those who need him or her.
5 Stages of the Deliberative Nursing Process
The Deliberative Nursing Process has five stages: assessment, diagnosis, planning, implementation, and evaluation.
Assessment
In the assessment stage, the nurse completes a holistic assessment of the patient’s needs. This is done without taking the reason for the encounter into consideration. The nurse uses a nursing framework to collect both subjective and objective data about the patient.
Diagnosis
The diagnosis stage uses the nurse’s clinical judgment about health problems. The diagnosis can then be confirmed using links to defining characteristics, related factors, and risk factors found in the patient’s assessment.
Planning
The planning stage addresses each of the problems identified in the diagnosis. Each problem is given a specific goal or outcome, and each goal or outcome is given nursing interventions to help achieve the goal. By the end of this stage, the nurse will have a nursing care plan.
Implementation
In the implementation stage, the nurse begins using the nursing care plan.
Evaluation
Finally, in the evaluation stage, the nurse looks at the patient’s progress toward the goals set in the nursing care plan. Changes can be made to the nursing care plan based on how well (or poorly) the patient is progressing toward the goals. If any new problems are identified in the evaluation stage, they can be addressed, and the process starts over again for those specific problems.
Analysis
Compared to other nursing theories, which are task-oriented, Orlando gave a clear-cut approach to patient-oriented nursing theory. It uplifts the integrity of individualized nursing care. This strengthens the role of the nurse as an independent nurse advocate for the patient. The nurse-patient interaction’s dynamic concept was justified since the patient’s participation in the relationship was sought. The whole process is in constant revision through continuous validation of the nurse’s findings with that of the patient. Because the nurse has to explore her reactions with the patient constantly, it prevents inaccurate diagnosis or ineffective plans. Since the model is applied to an immediate situation, its applicability to a long-term care plan is not feasible. The concept of interaction also limits it to individuals capable of conversing, a shared limitation with other nurse-client dynamic theories – this theory does not cover unconscious patients.
Strengths
The guarantee that patients will be treated as individuals is very much applied in Orlando’s theory of the Deliberative Nursing Process. Each patient will have an active and constant input into their own care.
The assertion of nursing’s independence as a profession and her belief that this independence must be based on a sound theoretical framework.
The model also guides the nurse to evaluate her care in terms of objectively observable patient outcomes.
Weaknesses
The lack of operational definitions of society or environment was evident, limiting the development of the research hypothesis.
Orlando’s work focuses on short-term care, particularly aware and conscious individuals, and the virtual absence of reference groups or family members.
Conclusion
Orlando’s nursing theory stresses the reciprocal relationship between patient and nurse. What the nurse and the patient say and do affects them both. Orlando views nursing’s professional function as finding out and meeting the patient’s immediate need for help. She was one of the first nursing leaders to identify and emphasize the nursing process elements and the critical importance of the patient’s participation in the nursing process. Orlando’s theory focuses on how to produce improvement in the patient’s behavior. Evidence of relieving the patient’s distress is seen as positive changes in the patient’s observable behavior. Orlando may have facilitated the development of nurses as logical thinkers.
The Deliberative Nursing Process helps nurses achieve more successful patient outcomes such as fall reduction. Orlando’s theory remains a most effective practice theory that is especially helpful to new nurses as they begin their practice.
Recommended Resources
Recommended books and resources to learn more about nursing theory:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
- Nursing Theorists and Their Work (10th Edition) by Alligood
Nursing Theorists and Their Work, 10th Edition provides a clear, in-depth look at nursing theories of historical and international significance. Each chapter presents a key nursing theory or philosophy, showing how systematic theoretical evidence can enhance decision making, professionalism, and quality of care. - Knowledge Development in Nursing: Theory and Process (11th Edition)
Use the five patterns of knowing to help you develop sound clinical judgment. This edition reflects the latest thinking in nursing knowledge development and adds emphasis to real-world application. The content in this edition aligns with the new 2021 AACN Essentials for Nursing Education. - Nursing Knowledge and Theory Innovation, Second Edition: Advancing the Science of Practice (2nd Edition)
This text for graduate-level nursing students focuses on the science and philosophy of nursing knowledge development. It is distinguished by its focus on practical applications of theory for scholarly, evidence-based approaches. The second edition features important updates and a reorganization of information to better highlight the roles of theory and major philosophical perspectives. - Nursing Theories and Nursing Practice (5th Edition)
The only nursing research and theory book with primary works by the original theorists. Explore the historical and contemporary theories that are the foundation of nursing practice today. The 5th Edition, continues to meet the needs of today’s students with an expanded focus on the middle range theories and practice models. - Strategies for Theory Construction in Nursing (6th Edition)
The clearest, most useful introduction to theory development methods. Reflecting vast changes in nursing practice, it covers advances both in theory development and in strategies for concept, statement, and theory development. It also builds further connections between nursing theory and evidence-based practice. - Middle Range Theory for Nursing (4th Edition)
This nursing book’s ability to break down complex ideas is part of what made this book a three-time recipient of the AJN Book of the Year award. This edition includes five completely new chapters of content essential for nursing books. New exemplars linking middle range theory to advanced nursing practice make it even more useful and expand the content to make it better. - Nursing Research: Methods and Critical Appraisal for Evidence-Based Practice
This book offers balanced coverage of both qualitative and quantitative research methodologies. This edition features new content on trending topics, including the Next-Generation NCLEX® Exam (NGN). - Nursing Research (11th Edition)
AJN award-winning authors Denise Polit and Cheryl Beck detail the latest methodologic innovations in nursing, medicine, and the social sciences. The updated 11th Edition adds two new chapters designed to help students ensure the accuracy and effectiveness of research methods. Extensively revised content throughout strengthens students’ ability to locate and rank clinical evidence.
See Also
Recommended site resources related to nursing theory:
- Nursing Theories and Theorists: The Definitive Guide for Nurses MUST READ!
In this guide for nursing theories, we aim to help you understand what comprises a nursing theory and its importance, purpose, history, types or classifications, and give you an overview through summaries of selected nursing theories.
Other resources related to nursing theory:
- Betty Neuman: Neuman Systems Model
- Dorothea Orem: Self-Care Deficit Theory
- Dorothy Johnson: Behavioral System Model
- Faye Abdellah: 21 Nursing Problems Theory
- Florence Nightingale: Environmental Theory
- Hildegard Peplau: Interpersonal Relations Theory
- Ida Jean Orlando: Deliberative Nursing Process Theory
- Imogene King: Theory of Goal Attainment
- Jean Watson: Theory of Human Caring
- Lydia Hall: Care, Cure, Core Nursing Theory
- Madeleine Leininger: Transcultural Nursing Theory
- Martha Rogers: Science of Unitary Human Beings
- Myra Estrin Levine: The Conservation Model of Nursing
- Nola Pender: Health Promotion Model
- Sister Callista Roy: Adaptation Model of Nursing
- Virginia Henderson: Nursing Need Theory
References
References and sources for this study guide about Ida Jean Orlando:
- George, J.B. (2011). Nursing theories: The base for professional nursing practice (6th ed.). Philadelphia: Pearson.com/nursing_theory/Orlando_nursing_process.html
- Orlando, I. J. (1972). The discipline and teaching of nursing process. In George, J. (Ed.). Nursing theories: the base for professional nursing practice. Norwalk, Connecticut: Appleton & Lange.
- Orlando, I. J. (1990). The dynamic nurse-patient relationship: Function, process, and principles. In George, J. (Ed.). Nursing theories: the base for professional nursing practice. Norwalk, Connecticut: Appleton & Lange.
- Potter, P.A., & Perry, A.G. (2012). Fundamentals of nursing (8th ed.). St. Louis, MO: Mosby Elsevier.
- Schmieding, N. (1990). An integrative nursing theoretical framework. Journal of Advanced. Nursing, 15(4), 463-467.
External Links
- Ida Jean Orlando: A Nursing Process Theory (Notes on Nursing Theories)
- Nursing Theorists and Their Work, 8th Edition
With contributions by Wayne, G. (for Biography), Vera, M., Ramirez, Q.

















Leave a Comment