The “5 Rights” of medication administration—right patient, right drug, right dose, right route, and right time—have long been a foundational framework in nursing to ensure patient safety and effective care. Developed to minimize medication errors and enhance the reliability of drug administration, these principles have been integral in teaching and clinical practice. However, despite their longstanding use, medication errors persist, highlighting the need for a more comprehensive approach. This has led to the proposal of expanding the framework to the “10 Rights” to address additional critical aspects right to refuse, right knowledge and understanding, right questions or challenges, right advice, and right response, thus further enhancing patient safety and care quality in increasingly complex healthcare environments.
Medication Errors
Medication errors can occur from preparation to administration and affect patient outcomes. Ensuring safe medication requires understanding the drug’s purpose, pharmacokinetics, pharmacodynamics, and considering patient care. Errors are common in primary care, with rates up to 42%.
Medication errors impact more than 7 million US patients every year and 1 in 10 hospital patients will experience a medication error during their stay. The FDA receives more than 100,000 reports each year associated with suspected medication error. While most medication errors don’t have any serious consequences, some can cause longer hospital stays, disability, birth defects, or even death.
Despite few serious errors, the high volume of prescriptions poses significant risks, including adverse reactions, interactions, reduced efficacy, and increased healthcare use. Medication-related hospital admissions are notably high, particularly in the elderly due to polypharmacy.
Causes of medication errors, may include the following:
- Healthcare Factors: Lack of training, inadequate drug knowledge, overwork, fatigue, poor communication.
- Patient Factors: Literacy, language barriers, complex cases, polypharmacy.
- Environmental Factors: High workload, time pressures, distractions, poor conditions.
- System Issues: Medication naming, labeling, packaging, computer system challenges, poor communication at care interfaces.
Efforts to reduce medication errors often focus on the “5 Rights” (right patient, right drug, right dose, right route, and right time), but this framework alone is insufficient. Strategies to address human, system, and environmental factors are crucial such as protected time for medication administration, improved team communication, and the use of technological interventions like computerized physician order entry (CPOE) and barcoding. Regular training and education are essential for maintaining healthcare professionals’ competency and reducing errors.
Medication management involves all health professionals and stakeholders, including drug companies, packaging designers, doctors, pharmacists, nurses, paramedics, patients, and policymakers.
The 10 R’s Approach
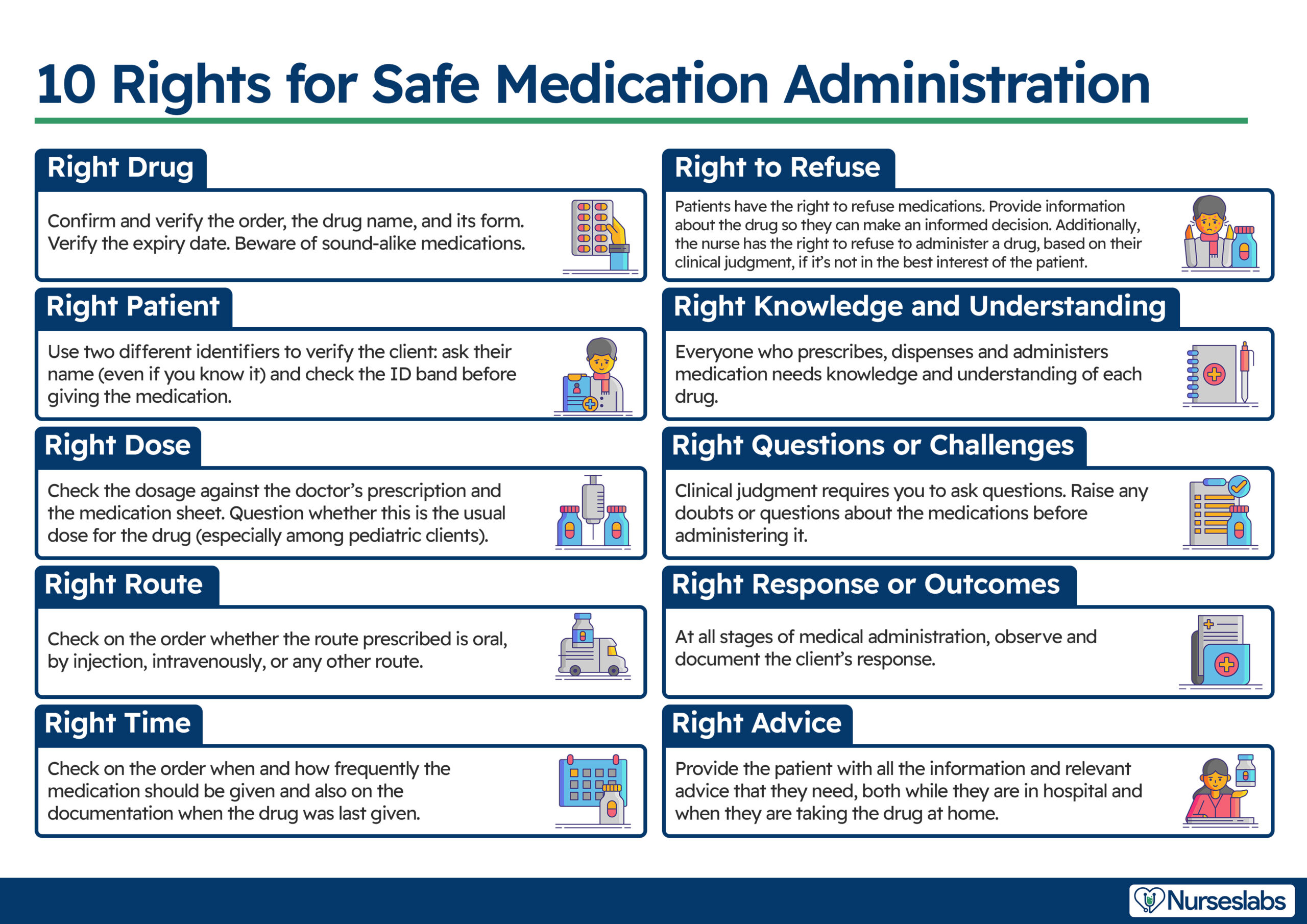
Building on the traditional “5 Rights” (right patient, drug, dose, route, and time), this article discusses the expanded “10 Rights” approach to medication management.
- Right Patient
- Right Drug
- Right Dose
- Right Route
- Right Time
- Right to Refuse (Patient and Nurse)
- Right Knowledge and Understanding
- Right Questions or Challenges
- Right Advice
- Right Response
Right Drug
Right Drug ensure that the medication administered matches the prescribed drug and is in the correct form for the prescribed route.
It is crucial to differentiate between similarly named medications, as they can have vastly different effects. To minimize confusion, prescribers are encouraged to write full generic names and indications rather than brand names, and clear documentation is essential to avoid errors caused by poor handwriting and abbreviations.
For example, consider the medications Celebrex (celecoxib) and Celexa (citalopram). Celecoxib is a nonsteroidal anti-inflammatory drug (NSAID) used to treat pain and inflammation, while citalopram is an antidepressant. Administering the wrong drug due to name similarity can lead to severe adverse effects and ineffective treatment.
Nurses should verify the medication name and expiration date on the packaging before administration. They should routinely ask patients about known allergies or previous allergic reactions to medications, educating them on the difference between allergic reactions (e.g., skin rash, anaphylaxis) and expected side effects (e.g., nausea, diarrhea). Research indicates that up to one-third of medication errors involve administering the wrong medication. Nurses should always verify with the prescriber if there is any uncertainty about the medication name or suspicion of an error.
Medications must also be administered in the correct form. For instance, paracetamol comes in tablets, syrup, suppositories, and intravenous ampoules. Errors can occur when these forms are confused, such as when oral medication is mistakenly given intravenously.
Some medications need to be crushed for administration through a nasogastric tube, but certain tablets, like enteric-coated ones, should not be crushed as they are designed to dissolve in the small intestine to avoid stomach irritation. Nurses should discuss alternatives with the prescriber or pharmacist if a medication only comes in an unsuitable form.
Packaging of some medications can also lead to errors. For instance, a patient may receive Acebutolol instead of Amiodarone due to similar blister pack designs. Nurses should familiarize themselves with medications in their clinical area that have similar packaging to avoid such errors.
Right Patient
Right Patient ensures that the medication is given to the correct individual.
Nurses should ask patients to state their full name aloud and verify this information against medical wristbands and ID numbers on the chart. Confirm the patient has been prescribed the medication. Check the patient’s name band and ensure there is a clear identifier. Make sure the patient knows they are receiving the drug and understands why. Addressing patients by their full name, rather than just first or last name, helps avoid confusion, especially in cases where multiple patients have similar names. For patients who may not wear wristbands or have altered mental states, such as psychiatric patients, nurses should use alternative methods to confirm the patient’s identity with appropriate care and due diligence.
Right Dose
Right Dose ensures medications are administered at the correct dosage, thereby preventing errors related to incorrect dosages, unit conversions, and substance concentrations.
Dosing errors stem from confusing or incorrect units used by prescribers. Misleading abbreviations, like using µg instead of mcg for micrograms, and improper use of decimal points (e.g., 10.0mg), can lead to significant errors. Nurses must use correct units when calculating medication volumes to prevent serious mistakes, such as administering 5ml of morphine at 20mg/ml instead of 5mg, which can be fatal.
To prevent these errors, nurses should consult with pharmacy personnel, use calculators for accurate arithmetic, and cross-check with patients or their families about usual doses administered at home. These strategies ensure the correct dose is consistently delivered, enhancing patient safety.
Nurses must exercise vigilance when reading medication charts to avoid these errors and should always verify with the prescriber any dubious orders.
Right Route
Administering drugs via the Right Route ensures medications are administered via the correct method, significantly affecting absorption time, onset of action, and potential side effects.
Common routes include oral, intramuscular, intravenous, topical, and subcutaneous injection, with modern medicine introducing more complex routes like central venous catheters, PCA, epidural infusions, and intrathecal administration.
Nurses must be informed about newer and less common medications and their administration routes to ensure safe delivery. Understanding drug absorption and onset is crucial, as intravenous medications have faster action compared to oral medications.
Errors often occur when the correct medication is given via the incorrect route, such as administering Vincristine intravenously instead of intrathecally, leading to severe outcomes. Labeling issues and factors like neglect and workload also contribute to errors. Increasing medication complexity and technological advancements heighten these risks.
Right Time
Right Time ensures medications are administered at the time specified by the prescriber to maintain their therapeutic effect.
Medications should be given as close to the prescribed time as possible, ideally within a half-hour window, to avoid issues like altered bioavailability or other chemical mechanisms. Administering medications at the wrong time is a common source of errors in healthcare. Studies have shown that a significant portion of medication errors are due to incorrect timing, highlighting the need for stringent protocols and careful attention to medication schedules to ensure patient safety and efficacy of treatments.
For infusion medications, such as intravenous drugs, it is important to administer them at the correct rate to prevent adverse effects. For example, vancomycin must be infused slowly to avoid vancomycin flushing syndrome, a hypersensitivity reaction. Similarly, rapid infusion of medications like Digoxin can cause serious adverse effects such as vasoconstriction and hypertension.
Medications should be prepared at the appropriate time to ensure safety and effectiveness. Preparing medications well in advance can pose risks, such as with intravenous phenytoin, which must be administered shortly after preparation. Avoid preparing them for later shifts, as this increases the risk of errors. Administer medications as close to the prescribed time as possible, ideally within a half-hour window, to maintain their bioavailability. If workload or other factors cause delays, a medication error report should be completed to address and investigate the issues.
Right to Refuse
The Right to Refuse ensures that both nurses and patients can exercise their judgment regarding medication administration. Nurses can refuse or omit a drug if necessary, explaining their rationale, while patients have the right to refuse medication.
The traditional “5 Rights” of medication administration overlook complexities such as patients refusing medication due to difficulties in taking it or questioning its necessity, highlighting the need for a sixth right: the right of the patient to refuse medication. This right should also extend to nurses, allowing them to decline administering drugs if they believe it is unsafe or incorrectly prescribed.
Nurses should advocate for patient safety by making evidence-based decisions without fear of being accused of errors. For instance, a nurse might refuse to administer insulin if a patient’s blood sugar levels are already dangerously low, as giving the medication could result in hypoglycemia. Similarly, a nurse might decline to administer a sedative if the patient is exhibiting signs of severe respiratory depression, recognizing the potential for further compromising the patient’s breathing. Such decisions should reflect the nurse’s autonomy and clinical judgment, ensuring patient safety through evidence-based practice. Nurses should understand the appropriate actions to take when a patient refuses medication and identify and address any barriers to administration, such as dysphagia or confusion.
Right Knowledge and Understanding
Right Knowledge and Understanding emphasizes the importance of in-depth knowledge and understanding of pharmacology principles for safe drug administration.
This includes understanding drug naming conventions (chemical, generic, and trade names), how drugs are prepared and administered, and their pharmacokinetics (absorption, distribution, metabolism, and excretion) and pharmacodynamics (therapeutic and adverse effects). Additionally, healthcare professionals must be aware of potential side effects, drug toxicity, interactions, and poisoning.
Healthcare assistants (HCAs), who are increasingly involved in administering medicines, must possess the same level of knowledge as other health professionals about how medicines work, their interactions, and potential side effects. Qualified nurses and prescribers are responsible for ensuring that delegated staff have sufficient knowledge to safely administer medications.
Know the required monitoring before administration. Prepare and administer the medication according to local policies. Understand the patient’s preferences and have comprehensive knowledge of the drug’s pharmacokinetics, pharmacodynamics, action, interactions, side effects, expected outcomes, and potential adverse effects. Be familiar with the relevant laws.
Right Questions or Challenges
Right Questions or Challenges ensure the prescription is appropriate for the patient’s condition and written clearly with unambiguous instructions. Verify that the writing is legible. Communicate with other professionals as needed and access available resources like drug formularies and product information leaflets.
Right Questions or Challenges involves ensuring the appropriateness of the prescribed drug for the patient’s condition. Key considerations include confirming the prescription is clear and unambiguous, verifying dosing schedules, and ensuring the drug formulation suits the patient, such as using liquid preparations for those who have difficulty swallowing. It’s also crucial to assess whether the drug is being used for the right reasons and not merely to counteract side effects of another medication.
Additionally, nurses must verify that the medication is appropriate for the patient’s condition (right indication). For instance, antibiotics should not be given for viral infections, and sedatives should not be given to already sedated patients. When administering medication, nurses should explain its purpose to the patient, such as, “Here is your antibiotic for your chest infection.” If the patient responds with confusion about their diagnosis, it may indicate a potential error.
Concordance can be improved by considering dosing frequency and specific timings. For instance, slow-release preparations may require less frequent dosing and cause fewer side effects. Additionally, the risk of adverse drug interactions increases significantly with the number of medications a patient takes, reaching 100% with eight or more drugs. This is particularly relevant for elderly patients on multiple medications (polypharmacy).
Medication reviews by pharmacists, doctors, and non-medical prescribers are essential to identify potential errors, stop unnecessary medications, and ensure continuity of care, especially during transitions from hospital to home. In cases where the route of administration (e.g., intravenous) is no longer appropriate, nurses should advocate for changes, such as switching to oral medications.
Nurses must feel empowered to question prescriptions and other staff members, regardless of seniority, if they suspect a medication is inappropriate. This proactive approach helps prevent errors and ensures optimal patient care.
Right Response
Right Response involves reviewing the patient’s response to the medication to ensure the expected outcomes.
For instance, has a course of antibiotics resolved the infection? This includes monitoring the drug’s effects, such as reduced blood pressure or improved lung function, and ensuring the drug’s safety for the patient by checking for any harm, allergies, adverse effects, or interactions.
All health professionals involved in medication management share the responsibility for the right response. This involves documenting the medicines prescribed and administered, reviewing the patient’s response, and updating records to ensure continuity of care. It also includes reporting adverse drug reactions to relevant parties and updating allergy status as needed.
When a nurse administers medication, they must sign the medication chart to provide evidence of administration. Signing the chart before administering the medication is risky, as the patient may refuse or forget to take the medication. Conversely, failing to sign after administration can lead to another nurse mistakenly administering a repeat dose.
For ‘as needed’ (prn) medications, nurses should document the administration in the patient’s medical record, including the medication’s generic name, dose, time, route, reason for administration, and effect achieved.
Finally, the right response includes informing patients about what to do if their progress is not as expected and recording this information in the patient’s notes to ensure they know the appropriate actions to take.
Right Advice
Right Advice ensure the patient is informed about the medication. Provide advice, details, and information about the medication as needed.
Right advice focuses on ensuring that patients receive comprehensive advice about their medications. Health professionals should explain the drug’s actions, indications, side effects, correct timing, and expected outcomes. It’s essential that patients understand their medications and potential side effects. Nurses should also consider patient preferences and health beliefs.
Informing patients about possible side effects, how the medication works, its effectiveness, the risks of not taking it, and interactions with other medications are top priorities. This communication enhances the therapeutic relationship and improves medication adherence.
Tips for Safe Medication Administration
Other than the 10 Rights, here are some other tips on how to prevent medication errors:
- Mitigate Environmental Distractions. Administer medications in quiet, well-lit environments. Use visual reminders like “do not disturb” signs or bright tabards to minimize distractions. For example, placing a “medication in progress” sign on a patient’s door to minimize interruptions.
- Improve Team Communication. Enhance communication among healthcare team members to ensure better patient outcomes and reduce medication errors. For instance, using a standardized handoff protocol during shift changes.
- Implement Technological Solutions. Utilize computerized physician order entry (CPOE), barcoding of drugs, and automated dispensing devices to improve patient safety. For example, scanning barcodes on medication and patient wristbands to ensure correct administration.
- Promote a Reporting Culture. Encourage the reporting of near-misses and medication errors without fear of punishment to foster a learning environment and prevent future errors. For instance, creating an anonymous reporting system for medication errors as this can encourage reporting.
- Maintain Competency Through Training. Regularly update nurses’ skills and knowledge in medication administration, theoretical knowledge, and drug calculations to ensure competency and confidence. For example, conducting annual competency assessments and refresher courses.
- Adopt a Multidisciplinary Approach. Streamline prescribing and medication management by involving all healthcare professionals, including pharmacists, doctors, nurses, and policymakers, to ensure safe practices. For instance, holding regular interdisciplinary meetings to discuss patient care plans.
- Conduct Medication Reviews and Reconciliation. Regularly review and reconcile medications, especially during care transitions, to reduce hospital admissions and address polypharmacy. For instance, verifying medication lists during patient admissions and discharges.
- Educate Healthcare Providers. Provide ongoing education to healthcare providers to improve adherence to guidelines and enhance medication safety. For example, organizing monthly training sessions on new medications and guidelines.
- Empower Patients Through Education. Educate patients about their medications to promote safe self-administration and improve health outcomes. For instance, providing patients with clear instructions and informational leaflets about their medications.
- Use Multicomponent Interventions. Combine education, provider supervision, and community case management to reduce inappropriate prescribing and adverse drug events, particularly in elderly populations and low- and middle-income countries. For example, implementing a community outreach program to educate elderly patients about medication management.






























Leave a Comment