Measuring blood pressure is a fundamental skill in nursing, essential for monitoring a patient’s cardiovascular health. Accurate blood pressure readings provide critical information about a patient’s hemodynamic status and can help detect hypertension and hypotension. Nurses must be proficient in using both manual sphygmomanometers and automated blood pressure devices, ensuring proper technique to obtain precise measurements. This skill not only aids in diagnosing and managing various health conditions but also plays a key role in evaluating the effectiveness of treatments and interventions. Learn about the procedure and nursing responsibilities when measuring blood pressure.
Table of Contents
- What is Blood Pressure?
- What is a Normal Blood Pressure?
- Determinants of Blood Pressure
- Factors Affecting Blood Pressure
- Hypertension
- Hypotension
- Assessing Blood Pressure
- References
What is Blood Pressure?
Arterial blood pressure is the force exerted by circulating blood on the walls of the arteries, the blood vessels that carry oxygen-rich blood away from the heart to the rest of the body. It is a critical parameter that reflects the heart’s pumping efficiency and the resistance of the blood vessels. Arterial blood pressure is typically measured in millimeters of mercury (mmHg). It is represented by two values: systolic pressure and diastolic pressure.
Systolic, Diastolic, and Pulse Pressure
Arterial blood pressure is represented by two values: systolic pressure, the higher value indicating the pressure during the heart’s contraction, and diastolic pressure, the lower value indicating the pressure when the heart is at rest between beats. The difference between the diastolic and the systolic pressures is called the pulse pressure. Maintaining proper arterial blood pressure is essential for ensuring adequate blood flow to vital organs and tissues, and abnormalities in blood pressure can lead to various health issues such as hypertension, hypotension, heart disease, and stroke.
Mean Arterial Pressure (MAP)
Mean arterial pressure (MAP) is an important hemodynamic parameter that represents the average pressure in a person’s arteries during one cardiac cycle. It provides a better understanding of the perfusion pressure seen by the organs of the body than either systolic or diastolic pressure alone.
How to Compute MAP
There are several methods to calculate Mean Arterial Pressure (MAP). One commonly used and straightforward formula is: by multiplying the diastolic blood pressure to two, add it to the systolic blood pressure, and then divide the sum by 3.
For example:
If a patient has a blood pressure of 120/80 mmHg:
\text{MAP} = \frac{120 + (2 \times 80)}{3}
Multiply the diastolic blood pressure by two:
\text{MAP} = [120 + 160] / 3Add the systolic and diastolic blood pressure:
\text{MAP} = \frac{280}{3} \\For the result:
\text{MAP} = 93.33 \, \text{mmHg}
Normal Range of MAP
The normal range for MAP is typically between 70 and 100 mmHg. Maintaining MAP within this range is important for perfusion of vital organs such as the brain, kidneys, and heart. Values below this range may indicate insufficient blood flow, while values above may indicate excessive pressure on the blood vessels and organs.
Abnormal MAP
- Low MAP (< 70 mmHg). May suggest hypoperfusion, potentially leading to organ dysfunction and failure.
- High MAP (> 100 mmHg). May indicate hypertension, increasing the risk for cardiovascular events and end-organ damage.
What is a Normal Blood Pressure?
The American Heart Association typically defines normal blood pressure as a systolic pressure of less than 120 millimeters of mercury (mmHg) and a diastolic pressure of less than 80 mmHg. This is often expressed as 120/80 mmHg. Maintaining blood pressure within this range is helps in reducing the risk of cardiovascular diseases, including heart attack, stroke, and kidney problems. Blood pressure readings consistently above or below this range may indicate hypertension or hypotension, respectively, and require medical evaluation and management to prevent complications.
Determinants of Blood Pressure
Blood pressure is determined by a combination of several physiological factors that influence the force and volume of blood against the arterial walls. Understanding these determinants helps in comprehending the underlying mechanisms that regulate blood pressure and the potential causes of hypertension or hypotension. The primary determinants of blood pressure include:
1. Cardiac Output. The amount of blood the heart pumps per minute. Cardiac output is the product of heart rate (HR) and stroke volume (SV), where stroke volume is the amount of blood pumped with each beat. Increased cardiac output raises blood pressure, while decreased cardiac output lowers it.
2. Peripheral Resistance (PR). The resistance to blood flow offered by the blood vessels, primarily the arterioles. Factors affecting PR include vessel diameter (vasoconstriction increases resistance, vasodilation decreases resistance), blood viscosity, and vessel length. Increased peripheral resistance elevates blood pressure, whereas decreased resistance reduces it.
3. Blood Volume. The total amount of blood circulating within the vascular system. Higher blood volume increases blood pressure by raising the amount of blood returning to the heart, while lower blood volume decreases blood pressure.
4. Blood Viscosity. The thickness or stickiness of the blood. Higher viscosity (e.g., due to increased red blood cell count) increases peripheral resistance and therefore raises blood pressure. Lower viscosity reduces resistance and lowers blood pressure.
5. Elasticity of Arterial Walls. The ability of the arteries to expand and contract with each heartbeat. Healthy, elastic arteries help buffer the pressure changes. Loss of elasticity (as in arteriosclerosis) leads to higher systolic pressure and potentially higher overall blood pressure.
6. Neural Factors. The sympathetic nervous system (SNS) increases heart rate and vasoconstriction, raising blood pressure, while the parasympathetic nervous system (PNS) decreases heart rate, lowering blood pressure.
7. Hormonal Factors
- Renin-Angiotensin-Aldosterone System (RAAS). Regulates blood volume and systemic vascular resistance, influencing blood pressure. Angiotensin II causes vasoconstriction, and aldosterone increases sodium and water retention, both raising blood pressure.
- Antidiuretic Hormone (ADH). Promotes water retention by the kidneys, increasing blood volume and pressure.
- Adrenaline and Noradrenaline. Released from the adrenal medulla, these hormones increase heart rate and vasoconstriction, raising blood pressure.
8. Renal Regulation. The kidneys regulate blood pressure through the control of blood volume (via excretion or retention of water and sodium) and the secretion of renin, which influences the RAAS.
Factors Affecting Blood Pressure
Blood pressure can be influenced by a multitude of factors that range from biological and lifestyle to environmental and medical. Understanding these factors is essential for both prevention and management of hypertension and hypotension. The following are the key factors affecting blood pressure:
1. Age. As people age, blood vessels gradually lose their elasticity, and arterial stiffness increases. This can lead to higher systolic blood pressure. Additionally, age-related changes in kidney function can affect blood pressure regulation.
2. Exercise. Regular physical activity strengthens the heart, allowing it to pump blood with less effort, which can lower blood pressure. However, during exercise, blood pressure temporarily increases due to the increased demand for oxygen and nutrients by muscles.
3. Stress. Chronic stress can lead to consistently elevated blood pressure. Stress hormones like adrenaline and cortisol increase heart rate and cause vasoconstriction, which raises blood pressure. Acute stress also temporarily raises blood pressure.
4. Race. Certain racial groups, particularly African Americans, have a higher prevalence of hypertension. Genetic factors, lifestyle, socioeconomic status, and access to healthcare contribute to these differences.
5. Sex. Men are more likely to have high blood pressure at a younger age compared to women. However, post-menopause, women’s risk of hypertension increases, likely due to hormonal changes.
6. Medications. Various medications can affect blood pressure. For example, antihypertensive drugs lower blood pressure, while medications like corticosteroids, decongestants, and nonsteroidal anti-inflammatory drugs (NSAIDs) can raise it.
7. Diurnal Variations. Blood pressure naturally fluctuates throughout the day. It tends to be lower during sleep and rises upon waking (morning surge), peaking in the mid-morning and gradually declining in the evening. These variations are due to the body’s circadian rhythms.
8. Medical Conditions. Conditions such as chronic kidney disease, diabetes, sleep apnea, and thyroid disorders can influence blood pressure. For instance, kidney disease can affect the body’s ability to regulate fluid balance, while diabetes can damage blood vessels.
9. Temperature. Blood pressure can be affected by ambient temperature. Cold temperatures can cause vasoconstriction, raising blood pressure. Conversely, hot temperatures can cause vasodilation and sweating, which may lower blood pressure.
10. Diet. High salt intake is associated with elevated blood pressure due to increased fluid retention. Diets high in fruits, vegetables, and low-fat dairy products, such as the DASH diet, can help lower blood pressure. Alcohol and caffeine consumption can also impact blood pressure.
11. Weight. Obesity increases the risk of hypertension as it often leads to increased blood volume and arterial stiffness. Weight loss can significantly lower blood pressure in overweight individuals.
12. Smoking. Nicotine in cigarettes causes immediate increases in blood pressure due to vasoconstriction. Long-term smoking contributes to arterial damage and increases the risk of chronic hypertension.
13. Genetics. Family history plays a significant role in an individual’s risk of developing hypertension. Genetic predispositions can affect how the body regulates blood pressure.
14. Sleep. Poor sleep quality or sleep disorders like sleep apnea can lead to elevated blood pressure. Adequate, restful sleep helps regulate stress hormones and maintains healthy blood pressure levels.
15. Physical Position. Blood pressure can vary with body position. It is usually lower when lying down and can rise upon standing due to the effects of gravity on blood flow.
Hypertension
Hypertension, commonly known as high blood pressure, is a medical condition characterized by persistently elevated pressure in the arteries. It is a major risk factor for cardiovascular diseases, stroke, and kidney disease.
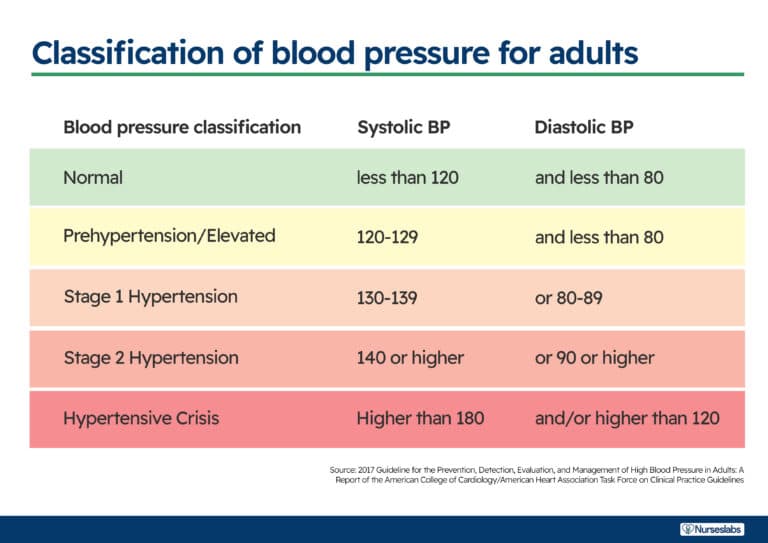
Normal and Hypertensive Ranges
- Normal Blood Pressure. Typically defined as a systolic pressure less than 120 mmHg and a diastolic pressure less than 80 mmHg.
- Elevated Blood Pressure. Systolic pressure between 120-129 mmHg and diastolic pressure less than 80 mmHg.
- Hypertension Stage 1. Systolic pressure between 130-139 mmHg or diastolic pressure between 80-89 mmHg.
- Hypertension Stage 2. Systolic pressure of 140 mmHg or higher, or diastolic pressure of 90 mmHg or higher.
- Hypertensive Crisis. Systolic pressure over 180 mmHg and/or diastolic pressure over 120 mmHg, requiring immediate medical attention.
See also: Hypertension
Causes and Risk Factors
- Primary (Essential) Hypertension. No identifiable cause, develops gradually over many years. It accounts for about 90-95% of cases.
- Secondary Hypertension. Caused by an underlying condition, such as kidney disease, hormonal disorders, or certain medications. It accounts for 5-10% of cases.
- Risk Factors. Include age, family history, obesity, sedentary lifestyle, tobacco use, excessive alcohol consumption, high-sodium diet, low-potassium diet, stress, and chronic conditions such as diabetes and sleep apnea.
Symptoms
- Often called the “silent killer” because it usually has no symptoms until it has caused significant health problems.
- In some cases, people may experience headaches, shortness of breath, or nosebleeds, but these symptoms are not specific and usually occur when blood pressure has reached a dangerously high level.
Diagnosis
- Blood pressure readings taken using a sphygmomanometer (blood pressure cuff) at multiple times and settings to confirm the diagnosis.
- Home blood pressure monitoring and ambulatory blood pressure monitoring may also be used.
Complications
- Long-term uncontrolled hypertension can lead to serious health problems, including heart attack, stroke, heart failure, aneurysm, chronic kidney disease, vision loss, and cognitive decline.
Management and Treatment
- Lifestyle Changes: Weight loss, regular physical activity, a healthy diet (such as the DASH diet), reducing sodium intake, limiting alcohol, quitting smoking, and managing stress.
- Medications: Various classes of antihypertensive medications, including diuretics, beta-blockers, ACE inhibitors, angiotensin II receptor blockers (ARBs), calcium channel blockers, and others, may be prescribed based on individual needs.
- Regular Monitoring: Regular blood pressure check-ups and ongoing monitoring to ensure effective management and adjustment of treatment as necessary.
Hypotension
Hypotension, commonly known as low blood pressure, is a condition where the blood pressure in the arteries is abnormally low. This can lead to inadequate blood flow to the organs, causing symptoms such as dizziness and fainting, particularly when standing up suddenly. While low blood pressure can be normal and asymptomatic for some individuals, it can also be a sign of an underlying health problem.
Causes
- Dehydration. Insufficient fluid intake can reduce blood volume, leading to low blood pressure.
- Heart Problems. Conditions such as bradycardia (slow heart rate), heart valve problems, heart attack, and heart failure can result in low blood pressure.
- Endocrine Disorders. Issues with the thyroid, adrenal insufficiency (Addison’s disease), and low blood sugar (hypoglycemia) can cause hypotension.
- Severe Infection (Septicemia). Severe infections can lead to septic shock, where blood pressure drops dangerously low.
- Blood Loss. Significant blood loss from injury or internal bleeding reduces blood volume and pressure.
- Lack of Nutrients. Deficiency in essential nutrients such as vitamin B12 and folate can prevent the body from producing enough red blood cells, leading to low blood pressure.
- Medications. Certain medications, including those for high blood pressure, heart conditions, and depression, can cause hypotension.
- Postural Hypotension (Orthostatic Hypotension). A sudden drop in blood pressure when standing up from a sitting or lying position.
- Postprandial Hypotension. A drop in blood pressure that occurs after eating, more common in older adults.
- Pregnancy. Blood pressure may drop during pregnancy due to changes in the circulatory system.
Symptoms
- Dizziness or Lightheadedness. Especially upon standing up quickly.
- Fainting. Loss of consciousness due to inadequate blood flow to the brain.
- Blurred Vision. Temporary visual disturbances.
- Nausea. Feeling of queasiness or unease in the stomach.
- Fatigue. Feeling unusually tired or weak.
- Lack of Concentration. Difficulty focusing or thinking clearly.
Diagnosis
- Blood Pressure Measurements. Repeated measurements using a sphygmomanometer to confirm low readings.
- Medical History and Physical Exam. Assessment of symptoms, medical history, and physical examination.
- Additional Tests. Depending on suspected underlying causes, tests may include blood tests, electrocardiogram (ECG), echocardiogram, stress test, tilt table test, and others.
Complications
- If left untreated, severe hypotension can cause shock, which is life-threatening and requires immediate medical attention.
- Chronic low blood pressure can lead to persistent symptoms that affect quality of life and increase the risk of falls and injuries.
Management and Treatment
- Lifestyle Changes. Increasing salt and fluid intake, wearing compression stockings, avoiding prolonged standing, and rising slowly from sitting or lying positions.
- Medications. In some cases, medications may be prescribed to raise blood pressure or manage the underlying condition causing hypotension.
- Treatment of Underlying Causes. Addressing the root cause of hypotension, whether it’s a heart problem, endocrine issue, or other condition, is crucial for effective management.
Assessing Blood Pressure
Assessing blood pressure is a fundamental skill for nurses, as it provides critical information about a patient’s cardiovascular health. Accurate measurement and interpretation of blood pressure are essential for diagnosing and managing conditions such as hypertension and hypotension. Here’s a comprehensive overview of the process and considerations involved in assessing blood pressure in nursing.
What is a Sphygmomanometer?
Blood pressure is measured using a blood pressure cuff, a sphygmomanometer, and a stethoscope. The cuff contains an inflatable bag, known as a bladder, encased in cloth with two tubes attached. One tube connects to a bulb, which is used to inflate the bladder. This bulb has a small valve on its side that controls the release and trapping of air in the bladder.
The other tube is connected to a sphygmomanometer, which displays the air pressure within the bladder. Sphygmomanometers come in two types: aneroid and digital. The aneroid sphygmomanometer features a calibrated dial with a needle that points to the pressure readings.
Blood Pressure Assessment Sites
Blood pressure can be measured at various anatomical sites, each providing valuable information depending on the clinical scenario. Understanding the different assessment sites and their specific considerations is crucial for obtaining accurate and reliable readings. Here are the primary sites used for blood pressure assessment in nursing:
1. Brachial Artery
- Location. The upper arm, just above the elbow crease.
- Procedure. Place the cuff about 1 inch above the antecubital fossa, with the stethoscope over the brachial artery.
- Advantages. The most common and standardized site; provides consistent and reliable readings; easily accessible.
- Considerations. Ensure the arm is at heart level and supported to avoid falsely high or low readings.
2. Radial Artery
- Location. The wrist, on the thumb side of the forearm.
- Procedure. Use a smaller cuff designed for the wrist and position it snugly around the wrist.
- Advantages. Useful for patients with large upper arms where a standard cuff won’t fit.
- Considerations. Arm and wrist should be at heart level to ensure accuracy; less commonly used due to potential for variability.
3. Popliteal Artery
- Location. The back of the knee, in the popliteal fossa.
- Procedure. Use a larger cuff around the thigh, and place the stethoscope over the popliteal artery.
- Advantages. Useful for patients with arm injuries or conditions that prevent brachial measurement.
- Considerations. Ensure the patient is lying down with the leg supported and relaxed; readings may be slightly higher than brachial readings.
4. Dorsalis Pedis and Posterior Tibial Arteries
- Location. The top of the foot (dorsalis pedis) or the inner side of the ankle (posterior tibial).
- Procedure. Use appropriate-sized cuffs for the ankle, and position the stethoscope over the respective artery.
- Advantages. Useful for patients with severe obesity, burns, or trauma affecting the upper limbs.
- Considerations. Less common; readings may be less reliable due to peripheral vasoconstriction or poor perfusion in the extremities.
5. Forearm
- Location. The forearm, midway between the elbow and wrist.
- Procedure. Use a smaller cuff appropriate for the forearm circumference, with the stethoscope over the radial artery.
- Advantages. Alternative for patients with upper arm restrictions.
- Considerations. Ensure the arm is at heart level; readings should be compared to brachial readings for consistency.
Considerations Across Different Sites
When measuring blood pressure, selecting the appropriate site is crucial for obtaining accurate and reliable readings. Each site has specific considerations that can affect the measurement results. Here are key factors to consider across different blood pressure assessment sites:
1. Accuracy
- Cuff Size and Fit. Ensure the cuff is appropriately sized for the selected site. An incorrect cuff size can lead to inaccurate readings.
- For the upper arm, the cuff should cover about 80% of the arm’s circumference and be wide enough to cover 40% of the arm’s length.
- For the wrist or forearm, ensure the cuff is snug but not too tight.
- Cuff Placement. The cuff should be placed correctly according to the specific site’s anatomy to ensure accurate pressure transmission.
- Heart Level. The limb where the blood pressure is being measured should be at heart level to avoid hydrostatic pressure effects that can alter readings. Lower or higher placement can result in falsely elevated or decreased readings, respectively.
2. Patient Factors
- Position. The patient’s position can significantly impact blood pressure readings.
- Seated Position. Feet should be flat on the floor, back supported, and arm supported at heart level.
- Lying Down. Ensure the arm or limb is supported and at heart level.
- Standing. May be used to assess orthostatic hypotension but requires careful positioning to maintain arm at heart level.
- Rest and Activity. Ensure the patient has rested for at least 5 minutes before measurement and has not engaged in vigorous activity, smoking, or caffeine consumption within 30 minutes prior.
- Anxiety and Stress. These can temporarily raise blood pressure; provide a calm environment and allow the patient to relax.
3. Clinical Context
- Critical Care. Non-standard sites may be necessary when traditional sites are inaccessible due to medical equipment, injuries, or surgeries.
- Frequency of Monitoring. Continuous monitoring may require arterial lines for accurate and ongoing measurements in critical care settings.
- Home Monitoring. Upper arm and wrist devices are common for home use. Educate patients on proper technique and positioning to ensure accurate readings.
4. Special Populations
- Children. Use pediatric-sized cuffs and consider alternative sites like the forearm or lower leg for young children.
- Elderly. Peripheral arteries may be less reliable due to atherosclerosis or poor perfusion. Ensure proper cuff placement and consider multiple readings.
- Obesity. Larger upper arms may necessitate forearm or wrist measurements. Use appropriately sized cuffs designed for larger limbs.
5. Site-Specific Considerations
- Upper Arm (Brachial Artery). Most standard and reliable; ensure arm is supported and at heart level.
- Wrist (Radial Artery). Ensure wrist is at heart level and straight; less reliable for patients with vascular issues.
- Thigh (Popliteal Artery). Suitable for patients with arm injuries; readings are typically higher than brachial readings, requiring adjusted reference ranges.
- Ankle (Dorsalis Pedis and Posterior Tibial Arteries). Less common and may be influenced by peripheral vascular conditions; used as a last resort.
Purpose of Assessing Blood Pressure
The purpose of assessing blood pressure is multifaceted, serving as a critical component of health monitoring and management. Here are the key purposes:
1. Diagnosing Hypertension and Hypotension. Regular blood pressure assessments help identify hypertension (high blood pressure) and hypotension (low blood pressure), enabling timely intervention and management to prevent complications.
2. Monitoring Treatment Efficacy. For patients already diagnosed with blood pressure-related conditions, regular assessments are essential to monitor the effectiveness of medications and lifestyle changes, ensuring that treatment goals are being met.
3. Preventing Cardiovascular Diseases. Blood pressure measurement is crucial in the early detection and prevention of cardiovascular diseases. Consistently high blood pressure can lead to heart attacks, strokes, and other cardiovascular conditions.
4. Assessing Overall Health. Blood pressure readings provide valuable insights into a person’s overall health status. Significant deviations from normal ranges can indicate underlying health issues that may require further investigation.
5. Guiding Clinical Decisions. Accurate blood pressure readings help healthcare providers make informed decisions regarding patient care, including the adjustment of medications, the need for further diagnostic tests, and the implementation of lifestyle modifications.
Assessment
Assessing blood pressure involves several steps to ensure accurate and reliable readings. This process includes preparing the patient, selecting the appropriate equipment, performing the measurement correctly, and interpreting the results.
1. Assess for signs and symptoms of hypertension, which may include headaches, ringing in the ears, facial flushing, nosebleeds, and fatigue.
Identifying these symptoms can help in early detection and management of hypertension, preventing potential complications such as cardiovascular disease or stroke.
2. Monitor for signs and symptoms of hypotension, such as tachycardia, dizziness, mental confusion, restlessness, cool and clammy skin, and pale or cyanotic skin.
Recognizing these symptoms is crucial for timely intervention to prevent severe hypotension, which can lead to inadequate perfusion of vital organs, causing shock or other life-threatening conditions.
3. Evaluate factors that can affect blood pressure, including recent physical activity, emotional stress, pain, and the time since the patient last smoked or consumed caffeine.
Understanding these factors is essential for obtaining accurate blood pressure readings and for making appropriate clinical decisions. These factors can cause temporary fluctuations in blood pressure and might mask the patient’s true baseline measurements.
4. Check if the blood pressure cuff contains latex. If the patient has a latex allergy, ensure to use a latex-free cuff.
Preventing exposure to latex in allergic patients is vital to avoid allergic reactions, which can range from mild dermatitis to severe anaphylaxis, compromising the patient’s safety and well-being.
Planning
The planning phase in measuring blood pressure in nursing encompasses several key steps to ensure accurate and effective assessment including delegation and preparation of equipment.
Delegation
In a clinical setting, the task of measuring blood pressure can be delegated to Unlicensed Assistive Personnel (UAP), such as nursing assistants or aides. Delegation of this task helps ensure efficiency and allows nurses to focus on more complex aspects of patient care. However, certain responsibilities and limitations are associated with this delegation.
Role of UAP
- Procedure Execution. UAP are trained to correctly apply the blood pressure cuff, use the sphygmomanometer or digital blood pressure monitor, and record the readings.
- Patient Interaction. They are also responsible for ensuring the patient is positioned correctly and is relaxed to obtain accurate readings.
- Reporting. After taking the measurement, UAP should report the readings promptly to the supervising nurse, especially if the readings fall outside of normal parameters.
Benefits of Delegation
- Efficiency. Delegating this task helps streamline workflow and allows for timely monitoring of blood pressure in a busy healthcare setting.
- Focus. It enables nurses to concentrate on interpreting data, making clinical decisions, and providing direct patient care.
Role of the Nurse
- Interpretation. Nurses are responsible for interpreting the blood pressure readings obtained by UAP. This involves understanding the context of the readings, considering patient history, current medications, and other relevant factors.
- Clinical Decision-Making. Nurses determine the appropriate response to abnormal blood pressure readings. This may include interventions such as medication adjustments, initiating further assessments, or contacting the physician for additional orders.
- Patient Education. Nurses also educate patients about the significance of their blood pressure readings and any necessary lifestyle or medication adjustments.
Responsibilities
- Accuracy Assurance. Nurses must ensure that UAP are adequately trained and competent in performing blood pressure measurements.
- Supervision. They provide supervision and are available to address any questions or issues that arise during the measurement process.
- Documentation. Nurses document the readings and any interventions or follow-up actions in the patient’s medical record, ensuring continuity of care.
Equipment
1. Manual Sphygmomanometer with Stethoscope
Components
- Cuff. A fabric bladder wrapped around the upper arm, available in various sizes to fit different arm circumferences.
- Bulb. A hand-operated bulb used to inflate the cuff with air.
- Valve. Allows controlled release of air from the cuff.
- Gauge. A calibrated dial (aneroid sphygmomanometer) or a mercury column (mercury sphygmomanometer) that displays pressure measurements.
- Stethoscope. Used to listen to Korotkoff sounds over the brachial artery, which indicate systolic and diastolic pressures.
Procedure
- The cuff is wrapped snugly around the upper arm and inflated using the bulb.
- Air pressure temporarily occludes the brachial artery, and then is slowly released.
- The healthcare provider listens through the stethoscope for the onset and cessation of Korotkoff sounds to determine systolic and diastolic pressures.
Advantages of Manual Sphygmomanometer with Stethoscope
- High accuracy when used correctly.
- Suitable for environments where precision is critical, such as hospitals and clinics.
- Reliable in patients with irregular heart rhythms.
Disadvantages of Manual Sphygmomanometer with Stethoscope
- Requires training and proficiency in auscultation.
- Time-consuming compared to automated devices.
- May not be suitable for patients with hearing impairments.
2. Digital Blood Pressure Monitors
Components
- Automatic Cuff. Similar to manual cuffs, but with an automated inflation mechanism.
- Digital Display. Shows systolic, diastolic, and pulse rate readings.
- Microprocessor. Analyzes oscillometric data to determine blood pressure.
Procedures
- The cuff is wrapped around the upper arm or wrist and secured.
- The monitor automatically inflates and deflates the cuff.
- Blood pressure and pulse rate are displayed digitally.
Advantages of Digital Blood Pressure Monitors
- Easy to use and requires minimal training.
- Provides quick readings, suitable for routine checks in clinics and homes.
- Some models store data for tracking trends over time.
Disadvantages of Digital Blood Pressure Monitors
- Accuracy may be affected by improper cuff placement or movement.
- Calibration and maintenance are necessary to ensure accuracy.
- Costlier than manual sphygmomanometers.
3. Ambulatory Blood Pressure Monitors
Components
- Portable Monitor. Worn by the patient and connected to a cuff.
- Cuff. Typically worn on the upper arm.
- Data Storage. Stores multiple blood pressure readings taken over a 24-hour period.
Procedure
- The cuff remains on the patient’s arm throughout the monitoring period.
- The device automatically inflates and deflates the cuff at preset intervals (e.g., every 15-30 minutes during the day and every hour at night).
- Data is stored and later downloaded for analysis by healthcare providers.
Advantages of Ambulatory Blood Pressure Monitors
- Provides comprehensive data on blood pressure variations throughout the day and night.
- Useful for diagnosing conditions like white-coat hypertension or masked hypertension.
- Helps assess the effectiveness of treatment over an extended period.
Disadvantages of Ambulatory Blood Pressure Monitors
- Patients may find wearing the device uncomfortable.
- Requires proper positioning and fit of the cuff for accurate readings.
- More expensive than traditional monitors.
Implementation
Here’s a detailed outline of the steps involved, along with the rationale for each step:
1. Ensure that the equipment is intact and functioning properly.
Proper functioning equipment ensures accurate readings. Checking for defects or malfunctions prevents erroneous measurements that could impact patient care.
2. Check for leaks in the tubing between the cuff and the sphygmomanometer.
Leaks can lead to inaccurate pressure readings. Ensuring the integrity of the tubing maintains the reliability of the equipment.
3. Prior to performing the procedure, introduce self and verify the patient’s identity using agency protocol.
Introducing oneself allows the patient to know who will be performing the procedure, fostering trust and a positive patient-provider relationship. Verifying the patient’s identity ensures that the procedure is performed on the correct patient, preventing errors and enhancing patient safety.
4. Perform hand hygiene.
Hand hygiene, including washing hands with soap and water or using alcohol-based hand rubs, is essential to prevent the spread of infection. Healthcare providers come into contact with various patients and surfaces throughout their shift, making proper hand hygiene a critical step in reducing the transmission of pathogens between patients, healthcare workers, and the environment.
5. Provide patient privacy.
When patients feel that their privacy is respected, they are more likely to feel comfortable and cooperative during examinations or procedures. This enhances the quality of care by reducing anxiety and facilitating open communication between the patient and healthcare provider.
6. Position patient properly.
Proper positioning of the patient is essential for accurate assessment and treatment. For instance, positioning a patient in the correct anatomical alignment ensures that physiological measurements, such as blood pressure or respiratory rate, are obtained accurately.
7. Place the cuff about 2.5 cm above the antecubital fossa (crease of the elbow), aligning the artery marker over the brachial artery.
Proper cuff placement ensures accurate compression of the brachial artery, facilitating the detection of Korotkoff sounds.
8. Locate the brachial artery and position the diaphragm of the stethoscope over it.
Palpation helps in identifying the artery’s location and ensures correct placement of the stethoscope for auscultation.
9. Inflate the cuff rapidly by squeezing the bulb while simultaneously observing the gauge.
Rapid inflation ensures that the cuff pressure exceeds systolic pressure quickly, facilitating the accurate detection of the beginning of Korotkoff sounds.
10. Slowly deflate the cuff by releasing air through the valve while listening for the first clear tapping sound and the disappearance of sound.
Korotkoff sounds correspond to changes in blood flow through the compressed artery and provide audible indicators of systolic and diastolic pressures.
11. Note the point at which the first Korotkoff sound is heard (systolic pressure) and when the sound disappears (diastolic pressure).
Accurate recording ensures documentation of the patient’s blood pressure status for ongoing monitoring and treatment decisions.
12. Completely deflate the cuff and remove it from the patient’s arm.
Complete deflation relieves any discomfort for the patient and prepares for subsequent assessments.
13. Wipe the cuff with an approved disinfectant.
Cuffs can become significantly contaminated. Many institutions use disposable blood pressure cuffs.
14. Record the blood pressure readings along with relevant patient information, including arm circumference, cuff size used, patient position, and any factors influencing the measurement (e.g., recent activity, pain).
Accurate documentation provides a clear record of the patient’s cardiovascular status and facilitates continuity of care among healthcare providers.
Evaluation
Evaluation in measuring blood pressure involves a systematic assessment and interpretation of the obtained blood pressure readings. Here’s a detailed elaboration on the evaluation process:
1. Accuracy and Consistency
After measuring blood pressure, the first step in evaluation is to ensure the accuracy and consistency of the readings. This involves checking for any potential errors during measurement, such as improper cuff size, inadequate rest for the patient, or incorrect positioning. Repeating the measurement if there are discrepancies ensures reliable data for evaluation.
2. Comparison with Baseline and Previous Readings
Evaluation includes comparing the current blood pressure readings with baseline measurements taken at previous visits or with the patient’s typical blood pressure range. This helps identify trends and changes over time, which are crucial for monitoring the patient’s cardiovascular health and response to treatment.
3. Clinical Guidelines and Standards
Blood pressure evaluation involves assessing readings against established clinical guidelines and standards, such as those provided by organizations like the American Heart Association (AHA) or the European Society of Cardiology (ESC). These guidelines define normal, elevated, and hypertensive ranges, guiding healthcare providers in interpreting the significance of the measured blood pressure.
4. Patient-Specific Factors
Evaluation considers patient-specific factors that may influence blood pressure readings, such as age, gender, medical history (including cardiovascular conditions and medications), lifestyle factors (such as diet and physical activity), and current health status (including acute illness or chronic conditions).
5. Assessment of Symptoms and Signs
In cases where blood pressure measurements are abnormal or atypical, evaluation includes assessing the patient for symptoms and signs associated with hypertension or hypotension. This may involve asking about symptoms like headaches, dizziness, chest pain, or visual disturbances, which can provide additional context to the measured blood pressure values.
6. Documentation and Reporting
Evaluation concludes with accurate documentation of the measured blood pressure readings, including systolic and diastolic values, along with any relevant clinical observations or patient symptoms. Reporting abnormal findings promptly to the healthcare team ensures timely intervention and management, contributing to patient safety and continuity of care.
7. Patient Education and Follow-Up
Finally, evaluation in blood pressure measurement includes patient education and counseling. This involves explaining the significance of the blood pressure readings to the patient, discussing lifestyle modifications or treatment plans as needed, and scheduling follow-up assessments to monitor progress or changes in blood pressure over time.
Common Errors in Assessing Blood Pressure
Assessing blood pressure is a fundamental skill in nursing, but several common errors can lead to inaccurate readings. These errors include:
1. Incorrect Cuff Size. Using a cuff that is too small or too large can significantly affect blood pressure readings. A cuff that is too small may result in falsely elevated readings, whereas a cuff that is too large can lead to falsely low readings.
2. Improper Arm Positioning. The patient’s arm should be positioned correctly at heart level during measurement. Incorrect positioning, such as having the arm above or below heart level, can affect blood pressure readings. The arm should also be supported and relaxed, with the palm facing upward.
3. Incomplete Deflation of the Cuff. Failing to completely deflate the cuff can result in inaccurate diastolic pressure readings. It’s crucial to deflate the cuff slowly and continuously while listening for the Korotkoff sounds until they completely disappear.
4. Failure to Locate the Brachial Artery. Placing the cuff incorrectly over the brachial artery can lead to inaccurate readings. Proper technique involves palpating the brachial artery with a penlight to ensure correct cuff placement.
5. Inadequate Rest Period. Patients should be seated quietly for at least 5 minutes before blood pressure measurement to allow stabilization of blood pressure. Failure to provide adequate rest can lead to falsely elevated readings, especially if the patient was physically active or stressed before measurement.
6. Talking During Measurement. Conversation during blood pressure measurement can elevate blood pressure due to stress or anxiety. It’s essential to minimize talking and distractions during the procedure to obtain accurate readings.
7. Unsupported Back or Feet. The patient should sit with their back supported and feet flat on the floor during measurement. Improper support or dangling feet can affect blood pressure readings.
8. Failure to Check for Patient Comfort. Discomfort or anxiety can cause an increase in blood pressure readings. Ensuring patient comfort, explaining the procedure, and providing privacy can help reduce anxiety and obtain more accurate measurements.
9. Not Using Proper Technique for Auscultation. Proper use of the stethoscope during auscultation is crucial. The diaphragm should be firmly placed over the brachial artery, and the earpieces should be correctly positioned in the ears to clearly hear Korotkoff sounds.
10. White Coat Hypertension. Some patients experience elevated blood pressure readings in clinical settings due to anxiety or stress (white coat hypertension). Multiple readings over time or using ambulatory blood pressure monitoring can help differentiate between true hypertension and white coat hypertension.
References
- Pickering, T. G., Shimbo, D., & Haas, D. (2006). Ambulatory blood-pressure monitoring. New England Journal of Medicine, 354(22), 2368–2374.
- Turner, J. R., Viera, A. J., & Shimbo, D. (2015). Ambulatory blood pressure monitoring in clinical practice: A review. The American Journal of Medicine, 128(1), 14–20.

































Leave a Comment