Learn about the nursing care management of patients with heart failure.
What is Heart Failure?
Heart failure, also known as congestive heart failure, is recognized as a clinical syndrome characterized by signs and symptoms of fluid overload or of inadequate tissue perfusion.
- Heart failure is the inability of the heart to pump sufficient blood to meet the needs of the tissues for oxygen and nutrients.
- The term heart failure indicates myocardial disease in which there is a problem with contraction of the heart (systolic dysfunction) or filling of the heart (diastolic dysfunction) that may or may not cause pulmonary or systemic congestion.
- Heart failure is most often a progressive, life-long condition that is managed with lifestyle changes and medications to prevent episodes of acute decompensated heart failure.
Classification
Heart failure is classified into two types: left-sided heart failure and right-sided heart failure.
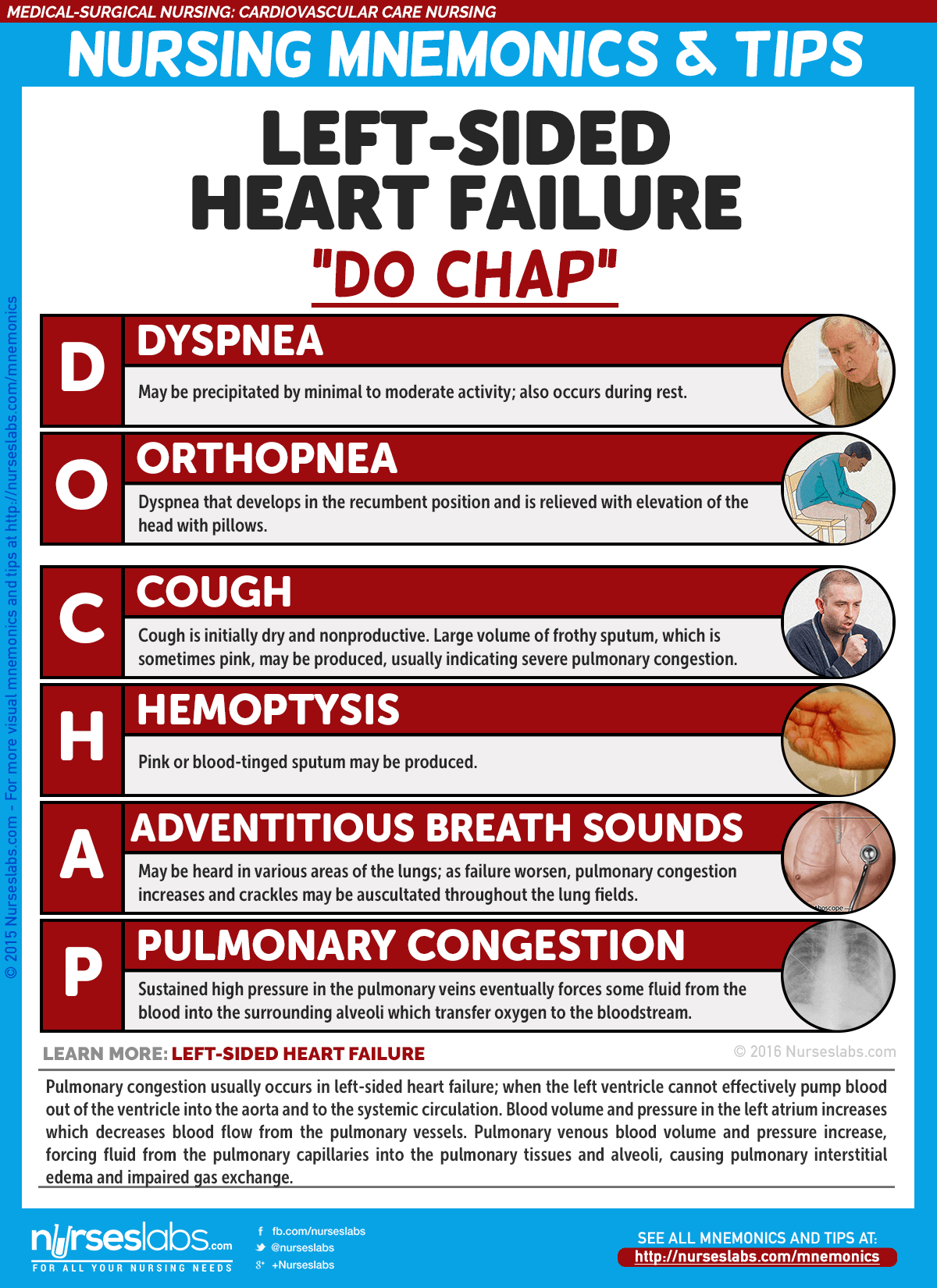
Left-Sided Heart Failure
- Left-sided heart failure or left ventricular failure have different manifestations with right-sided heart failure.
- Pulmonary congestion occurs when the left ventricle cannot effectively pump blood out of the ventricle into the aorta and the systemic circulation.
- Pulmonary venous blood volume and pressure increase, forcing fluid from the pulmonary capillaries into the pulmonary tissues and alveoli, causing pulmonary interstitial edema and impaired gas exchange.
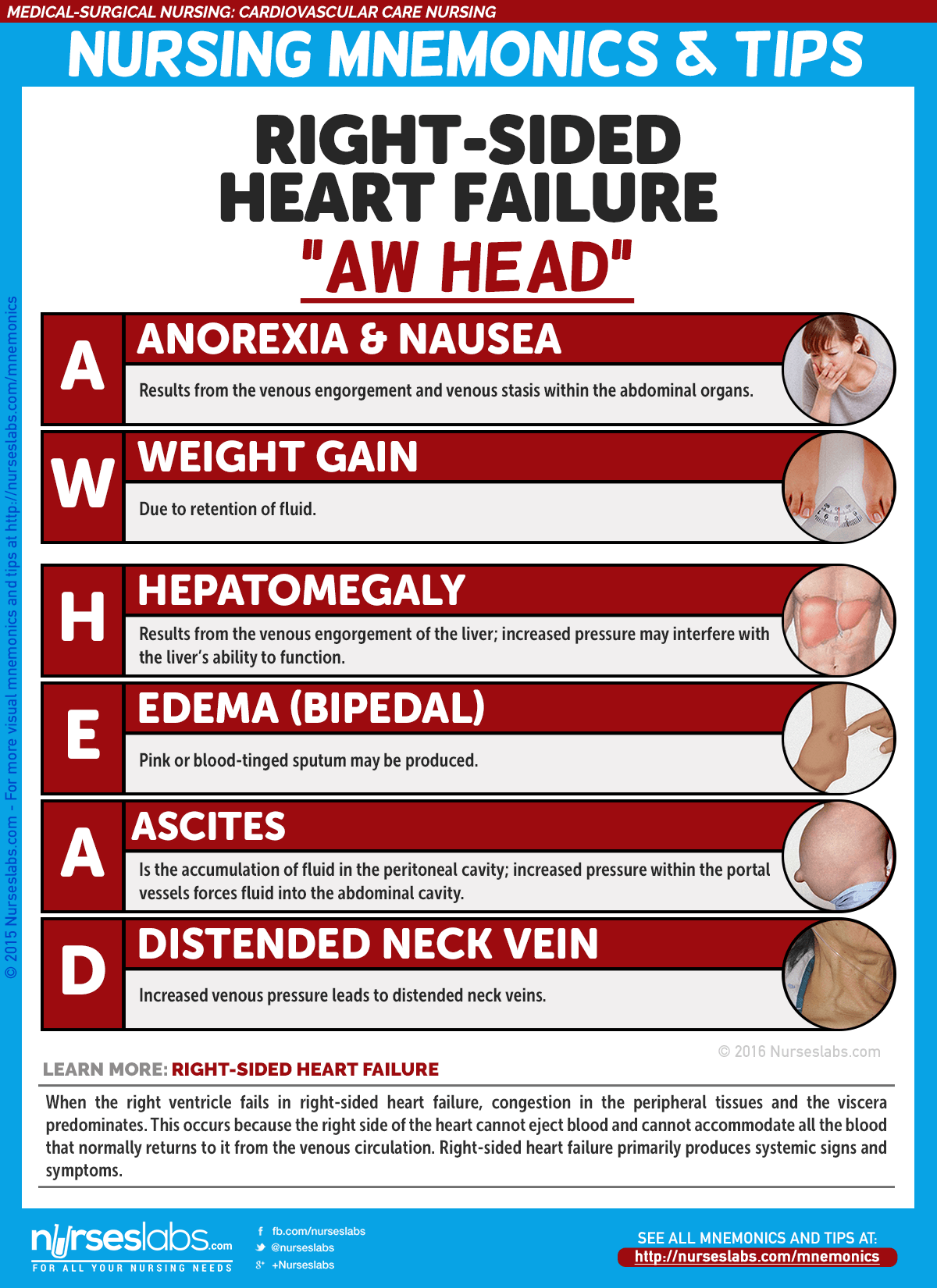
Right-Sided Heart Failure
- When the right ventricle fails, congestion in the peripheral tissues and the viscera predominates.
- The right side of the heart cannot eject blood and cannot accommodate all the blood that normally returns to it from the venous circulation.
- Increased venous pressure leads to JVD and increased capillary hydrostatic pressure throughout the venous system.
The American College of Cardiology and American Heart Association have classifications of heart failure.
- Stage A. Patients at high risk for developing left ventricular dysfunction but without structural heart disease or symptoms of heart failure.
- Stage B. Patients with left ventricular dysfunction or structural heart disease that has not developed symptoms of heart failure.
- Stage C. Patients with left ventricular dysfunction or structural heart disease with current or prior symptoms of heart failure.
- Stage D. Patients with refractory end-stage heart failure requiring specialized interventions.
Pathophysiology
Heart failure results from a variety of cardiovascular conditions, including chronic hypertension, coronary artery disease, and valvular disease.
- As HF develops, the body activates neurohormonal compensatory mechanisms.
- Systolic HF results in decreased blood volume being ejected from the ventricle.
- The sympathetic nervous system is then stimulated to release epinephrine and norepinephrine.
- Decrease in renal perfusion causes renin release, and then promotes the formation of angiotensin I.
- Angiotensin I is converted to angiotensin II by ACE which constricts the blood vessels and stimulates aldosterone release that causes sodium and fluid retention.
- There is a reduction in the contractility of the muscle fibers of the heart as the workload increases.
- Compensation. The heart compensates for the increased workload by increasing the thickness of the heart muscle.
Statistics
Just like coronary artery disease, the incidence of HF increases with age.
- More than 5 million people in the United States have HF.
- There are 550, 000 cases of HF diagnosed each year according to the American Heart Association.
- HF is most common among people older than 75 years of age.
- HF is now considered epidemic in the United States.
- HF is the most common reason for hospitalization of people older than 65 years of age.
- It is also the second most common reason for visits to the physician’s office.
- The estimated economic burden caused by HF is more than $33 billion annually in direct and indirect costs and is still expected to increase.
Incidences
Heart failure can affect both women and men, although the mortality is higher among women.
- There are also racial differences; at all ages death rates are higher in African American than in non-Hispanic whites.
- Heart failure is primarily a disease of older adults, affecting 6% to 10% of those older than 65.
- It is also the leading cause of hospitalization in older people.
Causes
Systemic diseases are usually one of the most common causes of heart failure.
- Coronary artery disease. Atherosclerosis of the coronary arteries is the primary cause of HF, and coronary artery disease is found in more than 60% of the patients with HF.
- Ischemia. Ischemia deprives heart cells of oxygen and leads to acidosis from the accumulation of lactic acid.
- Cardiomyopathy. HF due to cardiomyopathy is usually chronic and progressive.
- Systemic or pulmonary hypertension. Increase in afterload results from hypertension, which increases the workload of the heart and leads to hypertrophy of myocardial muscle fibers.
- Valvular heart disease. Blood has increasing difficulty moving forward, increasing pressure within the heart and increasing cardiac workload.
Clinical Manifestations
The clinical manifestations produced y the different types of HF are similar and therefore do not assist in differentiating the types of HF. The signs and symptoms can be related to the ventricle affected.
Left-sided HF
- Dyspnea or shortness of breath may be precipitated by minimal to moderate activity.
- Cough. The cough associated with left ventricular failure is initially dry and nonproductive.
- Pulmonary crackles. Bibasilar crackles are detected earlier and as it worsens, crackles can be auscultated across all lung fields.
- Low oxygen saturation levels. Oxygen saturation may decrease because of increased pulmonary pressures.
Right-sided HF
- Enlargement of the liver result from venous engorgement of the liver.
- Accumulation of fluid in the peritoneal cavity may increase pressure on the stomach and intestines and cause gastrointestinal distress.
- Loss of appetite results from venous engorgement and venous stasis within the abdominal organs.
Prevention
Prevention of heart failure mainly lies in lifestyle management.
- Healthy diet. Avoiding intake of fatty and salty foods greatly improves the cardiovascular health of an individual.
- Engaging in cardiovascular exercises thrice a week could keep the cardiovascular system up and running smoothly.
- Smoking cessation. Nicotine causes vasoconstriction that increases the pressure along the vessels.
Complications
Many potential problems associated with HF therapy relate to the use of diuretics.
- Hypokalemia. Excessive and repeated dieresis can lead to hypokalemia.
- Hyperkalemia. Hyperkalemia may occur with the use of ACE inhibitors, ARBs, or spironolactone.
- Prolonged diuretic therapy might lead to hyponatremia and result in disorientation, fatigue, apprehension, weakness, and muscle cramps.
- Dehydration and hypotension. Volume depletion from excessive fluid loss may lead to dehydration and hypotension.
Assessment and Diagnostic Findings
HF may go undetected until the patient presents with signs and symptoms of pulmonary and peripheral edema.
- ECG: May show hypertrophy, axis deviation, ischemia, and damage patterns. Dysrhythmias and ST-T segment abnormalities may be present.
- Chest x-ray: May show enlarged cardiac shadow or abnormal contour indicating ventricular aneurysm.
- Sonograms (echocardiography, Doppler, and transesophageal echocardiography): May reveal chamber dimensions, valvular function/structure, and ventricular dilation and dysfunction.
- Heart scan (MUGA): Measures cardiac volume, ejection fraction, and wall motion.
- Exercise or pharmacological stress myocardial perfusion: Determines presence of myocardial ischemia and wall motion abnormalities.
- PET scan: Sensitive test for evaluating myocardial ischemia and viability.
- Cardiac catheterization: Assesses pressures, differentiates right- versus left-sided heart failure, and evaluates coronary artery patency.
- Liver enzymes: Elevated in liver congestion/failure.
- Digoxin and other cardiac drug levels: Determines therapeutic range.
- Bleeding and clotting times: Identifies clotting risks and therapeutic range.
- Electrolytes: May be altered due to fluid shifts, renal function, or diuretic therapy.
- Pulse oximetry: Measures oxygen saturation, especially in conjunction with COPD or chronic HF.
- Arterial blood gases (ABGs): Reflects respiratory and acid-base status.
- BUN/creatinine: Evaluates renal perfusion and function.
- Serum albumin/transferrin: Indicates protein intake and liver function.
- Complete blood count (CBC): Assesses for anemia, polycythemia, and dilutional changes.
- ESR: Evaluates acute inflammatory reaction.
- Thyroid studies: Determines thyroid activity as a potential precipitator of HF.
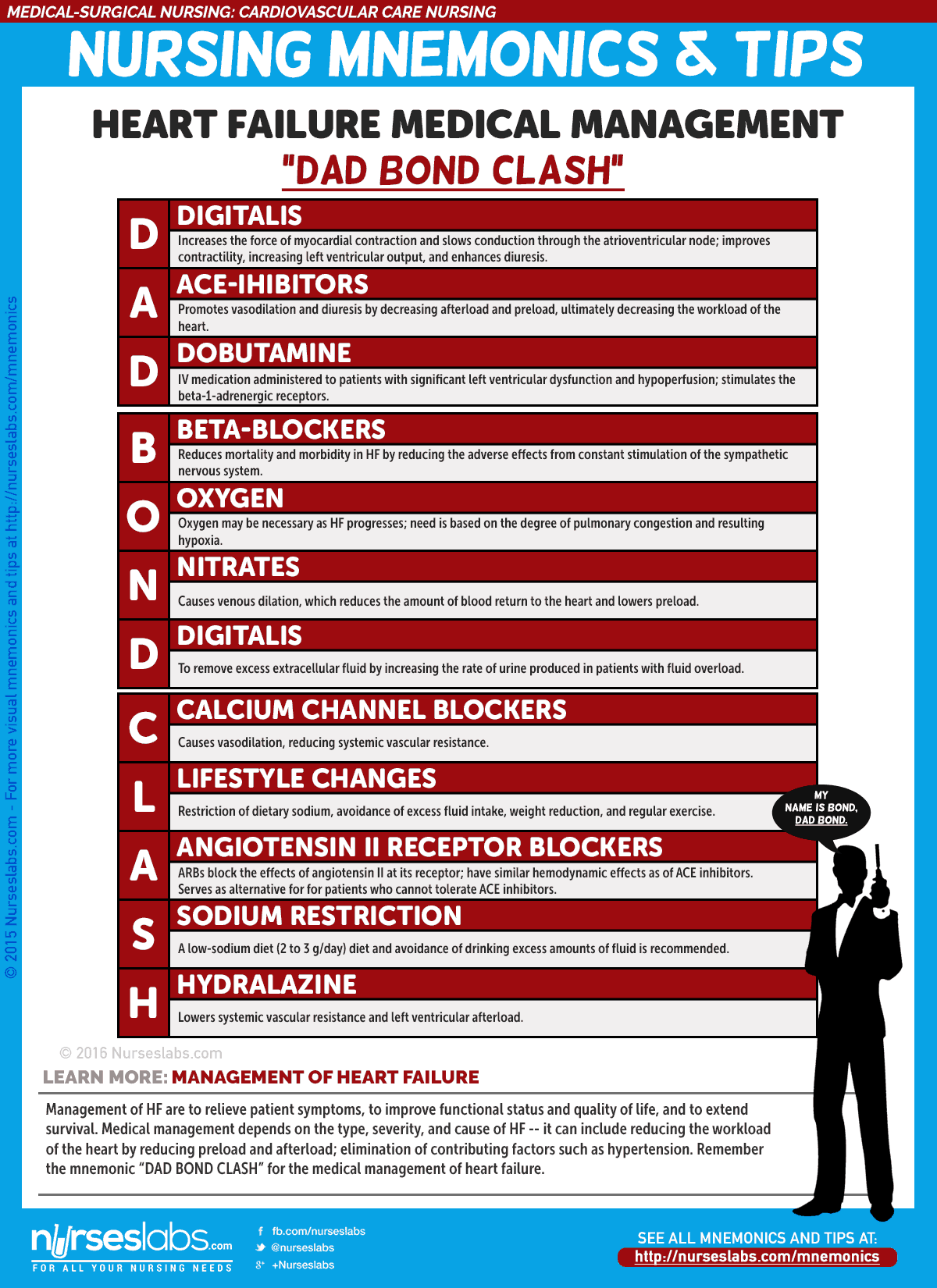
Medical Management
The overall goals of management of HF are to relieve patient symptoms, to improve functional status and quality of life, and to extend survival.
Pharmacologic Therapy
- ACE Inhibitors. ACE inhibitors slow the progression of HF, improve exercise tolerance, decrease the number of hospitalizations for HF, and promote vasodilation and diuresis by decreasing afterload and preload.
- Angiotensin II Receptor Blockers. ARBs block the conversion of angiotensin I at the angiotensin II receptor and cause decreased blood pressure, decreased systemic vascular resistance, and improved cardiac output.
- Beta Blockers. Beta blockers reduce the adverse effects from the constant stimulation of the sympathetic nervous system.
- Diuretics. Diuretics are prescribed to remove excess extracellular fluid by increasing the rate of urine produced in patients with signs and symptoms of fluid overload.
- Calcium Channel Blockers. CCBs cause vasodilation, reducing systemic vascular resistance but contraindicated in patients with systolic HF.
Nutritional Therapy
- Sodium restriction. A low sodium diet of 2 to 3g/day reduces fluid retention and the symptoms of peripheral and pulmonary congestion, and decrease the amount of circulating blood volume, which decreases myocardial work.
- Patient compliance. Patient compliance is important because dietary indiscretions may result in severe exacerbations of HF requiring hospitalizations.
Additional Therapy
- Supplemental Oxygen. The need for supplemental oxygen is based on the degree of pulmonary congestion and resulting hypoxia.
- Cardiac Resynchronization Therapy. CRT involves the use of a biventricular pacemaker to treat electrical conduction defects.
- Ultrafiltration. Ultrafiltration is an alternative intervention for patients with severe fluid overload.
- Cardiac Transplant. For some patients with end-stage heart failure, cardiac transplant is the only option for long term survival.
Nursing Management
Despite advances in the treatment of HF, morbidity and mortality remains high. Nurses have a major impact on outcomes for patients with HF.
For a more comprehensive nursing care management, please visit 18 Heart Failure Nursing Care Plans
Practice Quiz: Heart Failure
Let’s test what you’ve learned from this study guide with this 5-item quiz for heart failure.
1. The most frequent cause of hospitalization for people older than 75 years old is:
A. Angina pectoris
B. Heart failure
C. Hypertension
D. Pulmonary edema
2. The primary cause of heart failure is:
A. Arterial hypertension
B. Coronary atherosclerosis
C. Myocardial dysfunction
D. Valvular dysfunction
3. The dominant function in cardiac failure is:
A. Ascites
B. Hepatomegaly
C. Inadequate tissue perfusion
D. Nocturia
4. On assessment, the nurse knows that a patient who reports no symptoms of heart failure at rest but is symptomatic with increased physical activity would have a heart failure classification of:
A. Stage I
B. Stage II
C. Stage III
D. Stage IV
5. The diagnosis of heart failure is usually confirmed by:
A. Chest x-ray
B. Echocardiogram
C. Electrocardiogram
D. Ventriculogram
Answers and Rationale
1. Answer: B. Heart failure
- B: Heart failure is the most frequent cause of hospitalization for people older than 75 years old.
- A: Angina pectoris also occurs among people more than 75 years of age but it is not the most frequent cause of hospitalization.
- C: Hypertension also occurs among people more than 75 years of age but it is not the most frequent cause of hospitalization.
- D: Pulmonary edema also occurs among people more than 75 years of age but it is not the most frequent cause of hospitalization.
2. Answer: B. Coronary atherosclerosis
- B: Coronary atherosclerosis is the primary cause of heart failure.
- A: Arterial hypertension is not the primary cause of heart failure.
- C: Myocardial dysfunction is not a cause of heart failure.
- D: Valvular dysfunction is not the primary cause of heart failure.
3. Answer C. Inadequate tissue perfusion
- C: Inadequate tissue perfusion is the dominant function as low oxygenation occurs because of this.
- A: Ascites may occur in cardiac failure but is not considered as a dominant function.
- B: Hepatomegaly is present in heart failure but not a dominant function.
- D: Nocturia is not present in heart failure.
4. Answer: A. Stage I
- A: Stage I refer to a patient who reports no symptoms of heart failure at rest but becomes symptomatic with increased physical activity.
- B: Stage II refers to a patient who reports presence of symptoms with increased physical activities.
- C: Stage III refers to a patient who reports presence of symptoms with minimal physical activity.
- D: Stage IV refers to a patient who reports presence of symptoms even during at rest.
5. Answer: B: Echocardiogram
- B: An echocardiogram is usually performed to confirm the diagnosis of HF, and identify the underlying cause.
- A: Chest x-ray findings are also basis of the diagnosis of HF, but it is not the confirmatory diagnostic test.
- C: ECG is obtained to assist in the diagnosis.
- D: Ventriculogram is not a part of the diagnostic tests for HF.
See Also
Posts related to Heart Failure:
Great work and keep it up to help nurses.
Can you do an app for it on play store or IOS so that we can easily assess it anywhere at any time like medscape did
THANK YOU FOR YOUR WORK, IT HELP US AS NURSES TO BE UPDATED.
Great work keep it up sir.
Almighty God blessing you in everything of life.
This is an excellent resource for nurses! However, I think nurses would benefit from an update in the medication section to include angiotensin receptor neprilysin inhibitors (ARNI: sacubitril/valsartan), mineralocorticoid receptor antagonists (MRAs: spironolactone, eplerenone), and sodium-glucose co-transporter-2 inhibitors (SGLT2I: dapagliflozin, empagliflozin). The 2022 AHA/ACC/HFSA Guidelines for Heart Failure Management recommends quadruple therapy (ARNI, BB, MRA, SGLT2I) up-titrated to target or maximally tolerated doses for patients diagnosed with heart failure with a reduced ejection fraction to reverse, stabilize, or slow disease progression. These medications are also used in patients with heart failure and preserved ejection fraction.
Hi Keysha, thank you for sharing this. I’ll add your suggestions and the 2022 AHA/ACC/HFSA Guidelines on our next update for this care plan.