Otitis media is a common and frequently encountered ear infection that affects individuals of all ages, particularly young children. This condition involves inflammation and infection of the middle ear, often resulting from viral or bacterial pathogens. Otitis media can lead to various symptoms, including ear pain, fever, hearing difficulties, and fluid buildup behind the eardrum.
This article aims to serve as a comprehensive nursing guide to otitis media, diving into its causes, clinical manifestations, diagnostic methods, medical management, and nursing interventions.
Table of Contents
- What is Otitis Media?
- Pathophysiology
- Statistics and Incidences
- Causes
- Clinical Manifestations
- Assessment and Diagnostic Findings
- Medical Management
- Surgical Management
- Nursing Management
What is Otitis Media?
Otitis media is very common among children.
- Otitis media is an inflammation of the middle ear without reference to etiology or pathogenesis.
- It can be classified into many variants based on etiology, duration, symptomatology, and physical findings.
Pathophysiology
In children, developmental alterations of the eustachian tube, an immature immune system, and frequent infections of the upper respiratory mucosa all play major roles in AOM development.
- The most important factor in middle ear diseases is eustachian tube dysfunction, in which the mucosa at the pharyngeal end of the ET is part of the mucociliary system of the middle ear.
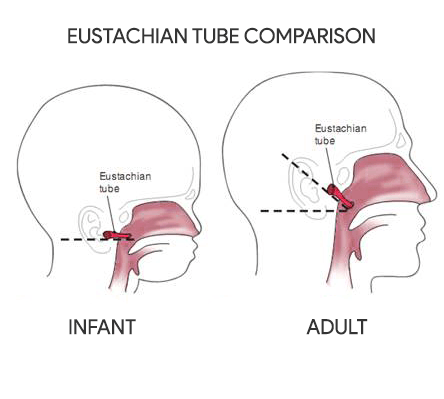
- The eustachian tube in an infant is shorter and wider than in an older child or adult.
- The tube is also straighter, thereby allowing nasopharyngeal secretions to enter the middle ear more easily.
- Interference with the mucosa by edema, tumor, or negative intratympanic pressure facilitates the direct extension of infectious processes from the nasopharynx to the middle ear, causing otitis media.
Statistics and Incidences
Otitis media is one of the most common infectious diseases of childhood.
- Two of every three children have at least one episode of otitis media by the time they are 1 year old.
- Otitis media accounts for approximately 20 million annual physician visits.
- Various epidemiologic studies report the prevalence rate of acute otitis media to be 17-20% within the first two years of life.
- One-third of children experience six or more episodes of otitis media by age 7 years.
- Peak prevalence of otitis media in both sexes occurs in children aged 6 to 18 months.
Causes
A multitude of host, infectious, allergic, and environmental factors contribute to the development of otitis media.
- Immature immune system. Otitis media is an infectious disease that prospers in an environment of decreased immune defenses.
- Genetic predisposition. Although familial clustering of otitis media has been demonstrated in studies that examined genetic associations of otitis media, separating genetic factors from environmental influences has been difficult.
- Anatomic abnormality. Children with anatomic abnormalities of the palate and associated musculature have a higher risk for otitis media.
- Physiologic dysfunction. Abnormalities in the physiologic function of the ET mucosa increase the risk of bacterial invasion of the middle ear and the resultant otitis media.
- Bacterial pathogens. The most common bacterial pathogen is Streptococcus pneumoniae, followed by Haemophilus influenzae, and Moraxella catarrhalis.
- Infant feeding methods. Many studies report that breastfeeding protects infants against otitis media.
Clinical Manifestations
Otitis media should be suspected in children with a history of characteristic head-neck and general symptoms.
- Otalgia. Young children may exhibit signs of otalgia by pulling on the affected ear or ears or pulling on the hair; otalgia apparently occurs more often when the child is lying down.
- Otorrhea. Discharge may come from the middle ear through a recently perforated tympanic membrane, or through another perforation.
- Headache. An older child may complain of a headache.
- Symptoms of upper respiratory infection. Concurrent or recent symptoms of URI, such as cough, rhinorrhea or sinus congestion is common.
- Fever. Two-thirds of children with otitis media have a history of fever, although fevers greater than 40°C are uncommon.
- Irritability. Irritability may be the sole early symptom in a young infant or toddler.
Assessment and Diagnostic Findings
Otitis media may be revealed through the following:
- Laboratory tests. Laboratory evaluation is usually unnecessary, although many experts recommend a full sepsis workup in infants younger than 12 weeks who present with fever and otitis media.
- Tympanocentesis. The criterion standard in the diagnosis of otitis media is tympanocentesis to determine middle ear fluid, followed by culture of fluid to identify causative pathogens.
Medical Management
In 2013, the American Academy of Pediatrics (AAP) and the American Academy of Family Practice published updated guidelines on the medical management of otitis media.
- Antibiotic therapy. Among other recommendations, the guidelines recommended antibiotics for bilateral and unilateral otitis media in children aged at least 6 months with severe signs and symptoms.
Pharmacologic Management
The FDA has approved more than a dozen antibiotics to treat otitis media.
- Antimicrobial agents. These agents remove pathogenic bacteria from the middle ear fluid.
Surgical Management
From the beginning, it is essential to integrate surgical management of otitis media with medical treatment.
- Myringotomy and TT placement. Myringotomy or the incision of the eardrums may be performed to establish drainage and to insert tiny tubes into the tympanic membrane to facilitate drainage.
- Adenoidectomy. The performance of adenoidectomy to treat patients with otitis media has generated extensive discussion and research, though potential benefits are controversial.
Nursing Management
Most infants and children with otitis media are cared for at home; therefore, a primary responsibility of the nurse is to teach the family caregivers about prevention and the care of the child.
Nursing Assessment
Assessment of a child with otitis media include the following:
- Physical examination. The infant’s ear is examined with an otoscope by pulling he ear down and back to straighten the ear canal.
- History. Assess if there is a history of trauma to the ears, affected siblings, a history of cranial/facial defects or any familial history of otitis media.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Acute pain related to the inflammation of the middle ear.
- Anxiety related to health status.
- Impaired verbal communication related to effects of hearing loss.
- Disturbed sensory perception related to obstruction, infection of the middle ear, or auditory nerve damage.
- Risk for injury related to hearing loss, decreased visual acuity.
- Infection related to presence of pathogens.
Nursing Care Planning and Goals
Main Article: 4 Otitis Media Nursing Care Plans
The major goals for the child with otitis media are:
- The child or parent will indicate absence of pain.
- The child will be free of infection.
- The parents will state understanding of preventive measures.
- The child will have normal hearing.
Nursing Interventions
Nursing care for the child with otitis media include:
- Positioning. Have the child sit up, raise head on pillows, or lie on unaffected ear.
- Heat application. Apply heating pad or a warm hot water bottle.
- Diet. Encourage breastfeeding of infants as breastfeeding affords natural immunity to infectious agents; position bole-fed infants upright when feeding.
- Hygiene. Teach family members to cover mouths and noses when sneezing or coughing and to wash hands frequently.
- Monitoring hearing loss. Assess hearing ability frequently.
Evaluation
Goals are met as evidenced by:
- The child or parent indicated absence of pain.
- The child is free of infection.
- The parents stated understanding of preventive measures.
- The child has normal hearing.
Documentation Guidelines
Documentation in a child with otitis media include the following:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcome.


This was very useful..thank you
One tip I always share with parents is to make sure their child is up to date on their pneumococcal vaccinations, as pneumococcal bacteria are a common cause of ear infections. Another important tip is to encourage frequent hand washing, especially after being in crowded or public places, to help prevent the spread of infections. It’s also important to monitor for signs of an ear infection, such as pain, redness, or discharge, and to seek prompt medical attention if these symptoms occur. Thank you for bringing attention to this important topic!
Super
I have this and It absolutely sucks! I started getting Eustachian tubes put in when I was 18months old, and still to this day I am having Estuation tubes put in every other year or so. I am currently, 24. I got my first set of hearing aids when I turned 17, bilateral. I hope one day in the future we can have an answer to permanently treat this instead of creating more and more scar tissue on my eardrums every single surgery I get. Scar tissue gets worse and worse every surgery I have. It’s building up on my eardrum, so it’s just decreasing my hearing every single time.
Hello Skyler M,
I’m really sorry to hear about your ongoing struggle with otitis meida and hearing loss. It sounds incredibly tough, especially with the impact on your hearing. It’s totally understandable to hope for a better, more lasting solution.
Have you explored any new treatment options lately? Sometimes specialists in audiology or advanced otology might have different approaches worth considering.