Papanicolaou smear (Pap smear, cervical smear) is a safe, noninvasive cytological examination for early detection of cervical cancer. During the 1900s, cervical cancer was one of the leading cause of death among women. It was until the year 1928, where a greek physician George Nicholas Papanicolaou was able to discover the difference between normal and malignant cervical cells by viewing the samples microscopically, hence Pap smear was invented.
For women ages 30 and above, this procedure can be done in conjunction with a test on Human papillomavirus (HPV), the most common sexually transmitted disease and primary causative agent for cervical cancer. The American Cancer Society recommends a Pap smear at least once every three years for women ages 21 to 29 who are not in a high-risk category and who have had negative results and who have had negative results from three previous Pap tests. While a Pap test and an HPV test is recommended every five years for women ages 30 to 65 years old. If a Pap smear is positive or suggests malignancy, a cervical biopsy can confirm the diagnosis.
Nurses play an important role in promoting public health awareness to inform, encourage and motivate the public in considering health screening such as pap smear. This pap smear study guide can help nurses understand their tasks and responsibilities during the procedure.
Table of Contents
- Indications of Pap Smear
- Interfering Factors
- Pap Smear Procedure
- Nursing Responsibility for Pap Smear
- Results
- Gallery
- References and Sources
Indications of Pap Smear
Pap smear is indicated for the following reasons:
- Identify the presence of sexually transmitted disease such as human papillomavirus (HPV), herpes, chlamydia, cytomegalovirus, Actinomyces spp., Trichomonas vaginalis, and Candida spp.
- Detect primary and metastatic neoplasms
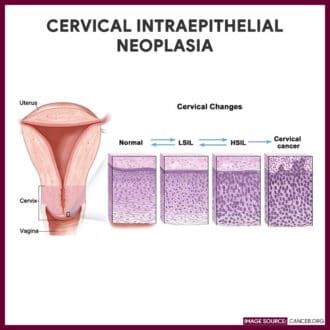
- Evaluate abnormal cervical changes (cervical dysplasia)
- Detect condyloma, vaginal adenosis, and endometriosis
- Assess hormonal function
- Evaluate the patient’s response to chemotherapy and radiation therapy
Interfering Factors
These are factors or conditions that may alter the outcome of the study
- Delay in fixing a specimen, allows the cells to dry therefore destroying the effectiveness of the stain and makes cytologic interpretation difficult
- Improper collection site may cause rejection of the specimen. Samples for hormonal evaluation are taken from the vagina while samples for cancer screening are obtained from the vaginal fornix
- Use of lubricating jelly on the speculum that may affect the viability of some organisms
- Specimen collection during normal menstruation since blood can contaminate the sample
- Douching, using tampons, or having sexual intercourse within 24 hours before the exam can wash away cellular deposits
- Existing vaginal infections that may interfere with hormonal cytology
Pap Smear Procedure
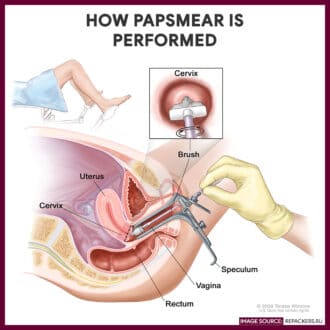
Pap smear is performed by a practitioner and takes approximately about 5 to 10 minutes. The step-by-step procedure is as follows:
- The patient is positioned.
The client is assisted in a supine, dorsal lithotomy position with feet in stirrups. - A speculum is inserted.
The practitioner puts on gloves and inserts an unlubricated plastic or metal speculum into the vagina and is opened gently to spread apart the vagina to access the cervix. The speculum may be moistened with saline solution or warm water to make insertion easier. - Cervical and vaginal specimens collection.
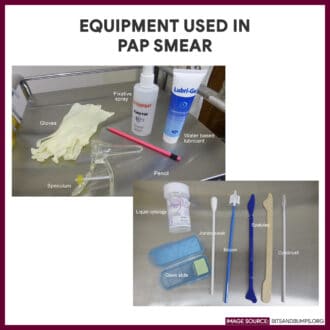
After positioning the speculum, specimen from the vagina and cervix are taken. A cytobrush is inserted inside the cervix and rolls it firmly into the endocervical canal. The brush is then rotated one turn and removed. A plastic or wooden spatula is utilized to scrape the outer opening of the cervix and vaginal wall. - Collection technique (Using the conventional collection).
The specimen from the brush and spatula is wiped on the slide and fixed immediately by immersing the slide in equal parts of 95% ethanol or by using a spray fixative. - Collection technique (Using the ThinPrep collection).
The brush and spatula are immediately immersed in a ThinPrep solution with a swirling motion to release the material. The brush and spatula are then removed from the solution and the bottle lid is replaced and secured. - Label the specimen
The slides are properly labeled with the patient’s name, age, initials of the health care provider collecting the specimen, date, and time of collection. - Specimens are sent to the laboratory
The specimens are transported to the laboratory for cytologic analysis. - Bimanual examination may follow.
After the removal of the speculum, a bimanual examination may be performed wherein the health care provider will insert two fingers of one hand inside the vaginal canal to feel the uterus and ovaries with the other hand on top of the abdomen.
Nursing Responsibility for Pap Smear
The following are the nursing interventions and nursing care considerations for a patient indicated for Pap smear.
Before the procedure
The following are the nursing interventions prior to pap smear:
- Secure patient’s consent. The test must be adequately explained and understood by the patient before a written, and informed consent is obtained.
- Obtain the patient’s health history. These include parity, date of last menstrual period, surgical status, contraceptive use, history of vaginal bleeding, history of previous Pap smears, and history of radiation or chemotherapy.
- Ask lists of the patient’s current medications. If a patient is taking a vaginal antibiotic, the pap smear is delayed for one month after the treatment has been completed.
- Explain that Pap smear is painless. The test requires that the cervix may be scraped and may experience minimal discomfort but no pain from the insertion of the speculum.
- Avoid interfering factors. Having sexual intercourse within 24 hours, douching within 48 hours, using a tampon, or applying vaginal creams or lotions is avoided before the test since it can wash away cellular deposits and change the ph of the vagina.
- Empty the bladder. Pap smear involves the insertion of the speculum into the vagina and could press down the lower abdomen.
After the procedure
The nurse should note the following nursing interventions after pap smear:
- Cleanse the perineal area. Secretions or excess lubricant from the vagina are removed and cleansed.
- Provide a sanitary pad. Slight spotting may occur after the pap smear.
- Provide information about the recommended frequency of screening. The American Cancer Society recommends screening every three years for women aged 21 to 29 years old and co-testing for HPV and cytological screening every five years for women aged 30 to 65 years old.
- Answer any questions or fears by the patient or family. Anxiety related with the pending test results may occur. Discussion of the implications of abnormal test results on the patient’s lifestyle may be provided to the patient.
Results
Normal findings in a Pap smear will indicate a negative result which means that no abnormal, malignant cells or atypical cells are found. While a positive result signifies that there are abnormal or unusual cells discovered, it is not synonymous to having cervical cancer.
The Bethesda System (TBS) is the current method for interpreting cervical cytology and it includes the following components.
1. Adequacy of specimen
- Satisfactory for evaluation: Describe the presence or absence of endocervical transformation zone component and other quality indicators such as partially obscuring blood, inflammation.
- Unsatisfactory for evaluation: Specimen is rejected (specify reason) or the specimen is processed and examined but unsatisfactory for evaluation of epithelial abnormalities (specify reason)
2. Interpretation/result
- Negative for intraepithelial lesion or malignancy
- Showing evidence of organism causing infection:
- Trichomonas vaginalis; fungal organisms morphologically consistent with Candida spp.; a shift in flora indicative of bacterial vaginosis (coccobacillus); bacteria consistent with Actinomyces spp.; cellular changes consistent with herpes simplex virus.
- Other non-neoplastic findings:
- Reactive cellular changes related to inflammation (includes repair), radiation, intrauterine device use, atrophy, glandular cell status after hysterectomy.
- Showing evidence of organism causing infection:
- Epithelial cell abnormalities
- Squamous cell abnormalities
- Atypical squamous cells of undetermined significance (ASC-US) cannot exclude HSIL (ASC-H):
- Low-grade squamous intraepithelial lesion (LSIL) encompassing HPV, mild dysplasia, cervical intraepithelial neoplasm (CIN) grade 1
- High-grade squamous intraepithelial lesion (HSIL) encompassing moderate and severe dysplasia, CIS/CIN grade 2 and CIN grade 3 with features suspicious for invasion (If invasion is suspected).
- Squamous cell carcinoma: indicate the presence of cancerous cells.
- Glandular cell
- Atypical glandular cells (not otherwise specify)
- Atypical glandular cells, favor neoplastic (not otherwise specify)
- Endocervical adenocarcinoma in situ
- Adenocarcinoma
- Squamous cell abnormalities
- Others
- Endometrial cells (in woman >=40 years of age)
Gallery
Related images to help you understand pap smear better.

References and Sources
Additional resources and references for the Pap Smear study guide:
- Adele Pillitteri. Maternal and Child Health Nursing:Care of the Childbearing and Childrearing Family. Lippincott Williams & Wilkins.
- Anne M. Van Leeuwen, Mickey Lynn Bladh. Laboratory & Diagnostic Tests with Nursing Implications: Davis’s
- Solomon, D., Davey, D., Kurman, R., Moriarty, A., O’connor, D., Prey, M., … & Young, N. (2002). The 2001 Bethesda System: terminology for reporting results of cervical cytology. Jama, 287(16), 2114-2119. [Link]
- Suzanne C. Smeltzer. Brunner & Suddarth’s Handbook of Laboratory and Diagnostic Tests: Lippincott Williams & Wilkins
Unfortunately, a pap smear will NOT detect clear cell adenocarcinoma — a rare cancer that tends to be found in women who are African American and over the age of 60. Mine was caught at a very early stage due to being symptomatic at the time. However, I am of Caucasian race (I hate that term, because we are all of the human race, and we all bleed red!!), and I was 48 at the time which made this a rare find indeed. Clear cell adenocarcinoma can only be diagnosed visual appearance of any abnormalities, and subsequent biopsy.