Acute nasopharyngitis, commonly known as the common cold, is a highly prevalent viral infection that affects the upper respiratory tract, including the nose and throat. While generally self-limiting, acute nasopharyngitis can cause discomfort and inconvenience, and its management focuses on symptomatic relief and supportive care.
This nursing note aims to discuss acute nasopharyngitis, including its etiology, clinical presentation, medical management, and nursing interventions.
Table of Contents
- What is Acute Nasopharyngitis?
- Pathophysiology
- Statistics and Incidences
- Causes
- Clinical Manifestations
- Assessment and Diagnostic Findings
- Medical Management
- Nursing Management
What is Acute Nasopharyngitis?
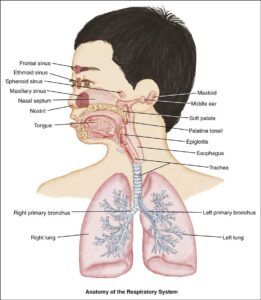
Upper respiratory infections include infectious processes involving any or all structures in the upper respiratory tract. It is characterized by symptoms such as a runny or stuffy nose, sneezing, sore throat, and coughing.
- Acute nasopharyngitis is caused by any number of different viruses, usually rhinoviruses, respiratory syncytial virus, adenovirus, influenza virus, or parainfluenza virus.
- The common cold is one of the most common infectious conditions of childhood.
- The primary concern for pharyngitis in children aged 2 years or older is that untreated GABHS pharyngitis may subsequently cause rheumatic fever.
Pathophysiology
Primary bacterial pathogens account for approximately 30% of cases of pharyngitis in children.
- GABHS pharyngitis is spread via respiratory droplets through close contact.
- It has an incubation period of 2-5 days.
- The bronchi and bronchioles become plugged with thick, viscid mucus, causing air to be trapped in the lungs.
- The child can breathe air in but has difficulty expelling it.
- This hinders the exchange of gases, and cyanosis appears.
Statistics and Incidences
Pharyngitis is a leading cause of pediatric ambulatory care visits.
- Approximately 10% of children seen by medical care providers each year have pharyngitis, and 25-50% of these children have GABHS pharyngitis.
- Approximately 20% of asymptomatic children are chronic carriers of GABHS.
- According to the Red Book, from 1990-1995, approximately 48,000 cases of epidemic diphtheria were reported in the former Soviet Union and central Asia.
- The peak prevalence of GABHS pharyngitis is in children aged 5-10 years.
Causes
Multiple entities can cause irritation and inflammation of the pharynx.
- Group A Beta-Hemolytic Streptococci (GABHS). GABHS is the primary organism of concern in most pediatric cases of pharyngitis because appropriate antibiotic therapy is effective and can eliminate the cardiac complications of rheumatic fever.
- Viruses. Viruses that may cause acute viral pharyngitis include the following: EBV (mononucleosis), rhinovirus, adenovirus, parainfluenza virus, coxsackievirus, coronavirus, echovirus, cytomegalovirus (CMV).
Clinical Manifestations
Symptoms of nasopharyngitis are more severe in infants and children than in adults.
- Fever. Fever is common, especially in young children; older children have low-grade fevers, which appear early and suddenly.
- Dyspnea. The onset of dyspnea is abrupt, sometimes preceded by a cough or nasal discharge.
- Cough. Symptoms include a dry and persistent cough.
- Nasal inflammation. Nasal inflammation may lead to obstruction of passages, and continual wiping away of secretions causes skin irritation to nares.
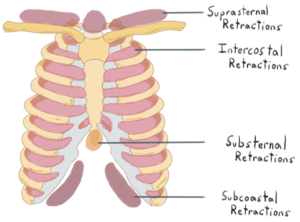
- Retractions. Suprasternal and substernal retractions are present.
- Barrel-shaped chest. The chest becomes barrel-shaped from the trapped air.
- Shallow respirations. Respirations are 60 to 80 breaths per minute.
- . Viral pharyngitis is usually associated with sneezing, rhinorrhea, and cough.
Assessment and Diagnostic Findings
Diagnosis is made from clinical findings and can be confirmed by laboratory testing of the mucus.
- Throat culture. A throat culture remains the standard for diagnosis, though results can take as long as 48 hours; throat culture results are highly sensitive and specific for group A beta-hemolytic streptococci (GABHS), but results can vary according to technique, sampling, and culture media.
- Rapid testing. Most institutions and clinics have rapid testing, which is useful when immediate therapy is desired; rapid testing can be highly reliable when used in conjunction with throat cultures; several rapid diagnostic tests are available; compared with throat culture, such tests are 70-90% sensitive and 95-100% specific.
- Testing for viral causes. If Epstein-Barr virus (EBV) is considered, obtain a complete blood count (CBC) to detect atypical cells in the white blood cell (WBC) differential, along with a Monospot test (or another rapid heterophile antibody test).
- Radiography. Imaging studies are usually not necessary unless a retropharyngeal, parapharyngeal, or peritonsillar abscess is suspected; in such cases, a plain lateral neck film can be used as an initial screening tool.
Medical Management
Approach considerations for a child with acute nasopharyngitis include:
- Oxygen administration. Oxygen may be administered in addition to the mist tent.
- Oral and IV fluids. For patients with signs of dehydration, administer adequate oral or intravenous (IV) fluids; remember that pain may limit oral intake, complicating hydration maintenance in the patient.
Pharmacologic Management
Medications for a child with acute nasopharyngitis include:
- Antibiotics. Penicillin is the typical therapy for GABHS pharyngitis, in conjunction with prevention of dehydration and supportive care for pain.
- Antipyretics. Antipyretics are usually prescribed for mild fever and discomfort.
- Corticosteroids. Corticosteroids (e.g., dexamethasone) have been suggested as an adjunctive therapy to decrease pain and shorten symptom duration in adults with pharyngitis.
Nursing Management
A cold is often the parents’ first introduction to an illness in their infants.
Nursing Assessment
Assessment of a child with nasopharyngitis include:
- History of exposure. A history of exposure to known carriers, fever, headache, and abdominal pain in conjunction with a sore throat suggests group A beta-hemolytic streptococcal (GABHS) pharyngitis.
- History of intake. Because supportive care is a primary goal in all cases, historical information regarding oral intake and hydration status is important.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Ineffective breathing pattern related to the inflammatory process in the respiratory tract.
- Ineffective airway clearance related to mechanical obstruction of the airway secretions and increased production of secretions.
- Anxiety related to the disease experienced by the child.
Nursing Care Planning and Goals
The major nursing care planning goals for a child with acute nasopharyngitis are:
- The patient will report increased energy.
- The patient will remain afebrile.
- The patient will expectorate sputum effectively.
- The patient will express feelings of comfort in maintaining air exchange.
- The patient will experience no further signs or symptoms of infection.
Nursing Interventions
Nursing interventions for a child with acute nasopharyngitis are:
- Positioning. Place the child in a semi-Fowlers position using pillows to facilitate lung expansion.
- Increase fluid intake. Encourage increased fluid intake to decrease the viscosity of secretions.
- Increase room humidity. Increase the humidity by using cool mist vaporizers to relieve stuffiness of the nose.
- Administer medications. Administer antibiotics as prescribed after a positive culture result.
Evaluation
Goals are met as evidenced by:
- The patient reported increased energy.
- The patient is afebrile.
- The patient was able to expectorate sputum effectively.
- The patient expressed feelings of comfort in maintaining air exchange.
- The patient experienced no further signs or symptoms of infection.
Documentation Guidelines
Documentation in a child with acute nasopharyngitis includes:
- Breath sounds, presence and character of secretions, use of accessory muscles for breathing.
- Plan of care.
- Teaching plan.
- Responses to interventions and actions performed.
- Attainment or progress towards desired outcomes.
- Modifications to the plan of care.

Thanks