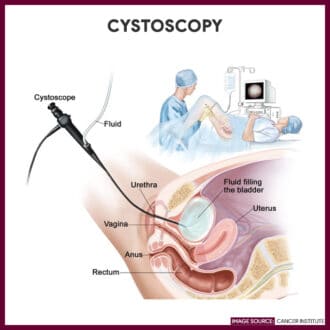
Cystoscopy, also known as cystoureterography or prostatography, is an invasive diagnostic procedure that allows direct visualization of the urethra, urinary bladder, and ureteral orifices through the transurethral insertion of a cystoscope into the bladder.
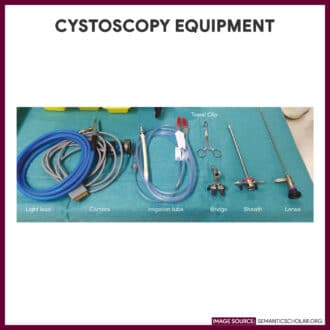
There are two types of cystoscopy: rigid and flexible. Rigid cystoscopy uses a thin, lighted tube that consists of an obturator and a telescope with a lens and light system; It is usually performed to take tissue samples and carry out complicated surgeries. It is done under general or spinal anesthesia. While flexible cystoscopy uses a flexible fiber-optic telescope to provide a diagnosis of urinary abnormalities and to evaluate the effectiveness of a treatment. It is performed under local anesthesia.
The nurse needs to help prepare the patient during cystoscopy. This study guide lists the tasks and responsibilities of the nurse during cystoscopy.
Indication
The cystoscopy may be performed for both diagnostic and therapeutic purposes:
Diagnostic Cystoscopy
- Assess the function of the kidneys by taking a urine specimen through ureteral catheters
- Assess changes in urinary elimination patterns
- Differentiate between benign and malignant bladder lesions
- Identify the source of hematuria
- Investigate the cause of recurrent urinary tract infection
- Evaluate the extent of enlarged prostate and degree of obstructions
- Evaluate urinary tract abnormalities such as dysuria, urgency, incontinence, frequency, retention, and inadequate stream
- Diagnose congenital anomalies such as ureteroceles, diverticula, duplicate ureters, urethral or ureteral strictures, and areas of inflammation or ulceration
Therapeutic Cystoscopy
- Coagulate bleeding areas
- Dilate the urethra and ureters
- Remove and resect polyps and small bladder tumors
- Remove foreign bodies and renal calculi
- Implant radioactive seeds into a tumor
- Place ureteral catheters to drain urine from the renal pelvis or for retrograde pyelography
- Resect hypertrophied or malignant prostate gland (transurethral resection of the prostate)
Contraindication
Cystoscopy should not be done with the following:
- Patients with an acute form of urethritis, prostatitis, or cystitis because instrumentation may increase the risk of bacterial invasion, leading to sepsis
- Patients with bleeding disorders since instrumentation may lead to further bleeding from the lower urinary tract
- Patients who are pregnant, unless the potential benefits of a procedure outweigh the risk of maternal and fetal damage
Interfering Factors
These are factors or conditions that may alter the outcome of cystoscopy:
- Inability to cooperate or remain still during the procedure due to age, significant pain, or mental status
- Failure to follow dietary restrictions prior may lead to the cancellation or repetition of the procedure
Procedure
Cystoscopy is usually performed in the operating room or it can also be done in the clinic setting. The following are the steps for cystoscopy:
- Empty the bladder.
The patient is asked to empty his or her bladder before the procedure and to change into a surgical gown.
-
Place patient in a lithotomy position.
The patient is placed in the lithotomy position, the buttocks should be positioned at the edge of the table and the feet are placed in stirrups. - Skin prep the patient.
The genitalia is cleaned with an antiseptic solution, and the patient is draped.
- Sedative or local anesthesia is given.
A local anesthetic is instilled into the urethra if general anesthesia will not be used.
- Cystoscope is inserted.
The cystoscope or a urethroscope is inserted to examine the urethra before cystoscopy. The urethroscope has a sheat that may be left in place, and the cystoscope is inserted through it, avoiding multiple instrumentations.
- Urine is examined.
After insertion of the cystoscope, a sample of residual urine may be taken for culture or other analysis.
- Bladder is filled with irrigating solution.
The bladder is irrigated through an irrigation system attached to the scope. The irrigation fluid helps in bladder visualization.
- Other procedures may be performed such as:
-If a prostatic tumor is found, a biopsy specimen may be obtained by means of a cytology brush or biopsy forceps inserted through the scope. If the tumor is small and localized, it can be excised and fulgurated. This procedure is termed transurethral resection of the bladder.
-Polyps can also be identified and excised.
-Ulcers or bleeding sites can be fulgurated using electrocautery.
-Renal calculi can be crushed and removed from the ureters and bladder.
-Ureteral catheters can be inserted via the scope to obtain urine samples from each kidney for comparative analysis and radiographic studies.
-Ureteral and urethral strictures can also be dilated during this procedure. - Cystoscope is removed.
Upon completion of the examination and related procedures, the cystoscope is withdrawn.
- Specimen is sent to the laboratory.
Place obtained specimens in proper containers, label them properly, and immediately transport them to the laboratory.
Cystoscopy Nursing Responsibility
The following are the nursing interventions and nursing care considerations for the patient undergoing cystoscopy:
Before cystoscopy
The following are the nursing interventions prior to cystography:
- Assess patient’s understanding of the procedure and answer any queries. The procedure is usually performed in a urology clinic and it takes about 30-45 minutes. Inform the patient who will perform the test, where it will take place, and other health team members involved in the care.
- Obtain informed consent. A written and informed consent is signed prior to the procedure and before the administration of medications.
- Withhold blood thinning medications. Some examples are aspirin, warfarin (Coumadin), enoxaparin (Lovenox), heparin, clopidogrel (Plavix), and dabigatran (Pradaxa).
- Provide instruction for fasting and non-fasting preparation. Unless a general anesthetic has been ordered, inform the patient that he doesn’t need to restrict food and fluids. If a general anesthetic will be administered, instruct the patient to fast for at least 6 to 8 hours prior to the test.
- Establish an IV line. To allow infusion of fluids, anesthetics, sedatives or emergency medications.
- Prepare the patient. Instruct the patient to empty the bladder prior to the procedure and to change into the hospital gown provided.
- Administer sedation and other medications as ordered. Preoperative medications are given 1 hour before the test. Sedative decreases the spasm of the bladder sphincter, reducing the patient’s discomfort.
After cystoscopy
The nurse should note the following nursing care after cystoscopy:
- Monitor and record vital signs. An increase in pulse (tachycardia) and a decrease in blood pressure (hypotension) may indicate a sign of hemorrhage.
- Assess the patient’s ability to void at least 24 hours after the procedure. Urinary retention may be secondary to edema as a result from instrumentation.
- Observe the color of urine. Pink-tinged urine and burning or mild discomfort when urinating may be experienced for a few voidings after the procedure. This usually resolves within two or three days.
- Encourage increased fluid intake as indicated. Fluids will help flush the bladder to decrease the amount of bleeding and reduce the risk of infection.
- Encourage deep breathing exercises. These exercises may relieve the patient from bladder spasms.
- Provide warm sitz baths and administer mild analgesics as ordered. These may relieve urinary discomfort and promote muscle relaxation.
- Watch out for signs of serious complications (sepsis, bladder perforation, hematuria). Persistent, severe flank pain, elevated temperature over 101° F, chills, bright red blood or clots in the urine, painful urination, or urinary retention must be reported immediately to the HCP.
Normal Results
Normal findings in a cystography will show:
Abnormal Results
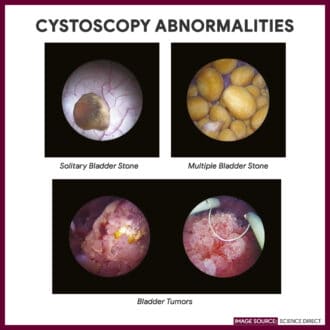
Abnormalities in a cystography will reveal:
- Bladder cancer
- Diverticulum of the bladder, fistula, stones, and strictures
- Foreign body
- Infection or inflammation
- Obstruction
- Polyps
- Prostatic hyperplasia
- Prostatitis
- Renal calculi
- Tumors
- Ureteral calculi
- Ureteral reflux
- Ureteral or urethral strictures
- Ureterocele
- Urinary fistula
- Urinary tract malformation and congenital anomalies
Gallery
Interesting images related to cystoscopy:





References
Additional resources and references for this guide:
- Anne M. Van Leeuwen, Mickey Lynn Bladh. Laboratory & Diagnostic Tests with Nursing Implications: Davis’s
- Suzanne C. Smeltzer. Brunner & Suddarth’s Handbook of Laboratory and Diagnostic Tests: Lippincott Williams & Wilkins
- Fenlon, H. M., Bell, T. V., Ahari, H. K., & Hussain, S. (1997). Virtual cystoscopy: early clinical experience. Radiology, 205(1), 272-275.
- Song, J. H., Francis, I. R., Platt, J. F., Cohan, R. H., Mohsin, J., Kielb, S. J., … & Montie, J. E. (2001). Bladder tumor detection at virtual cystoscopy. Radiology, 218(1), 95-100.
- Vining, D. J., Zagoria, R. J., Liu, K., & Stelts, D. (1996). CT cystoscopy: an innovation in bladder imaging. AJR. American journal of roentgenology, 166(2), 409-410.













Leave a Comment