Learn about the nursing care management of patients with hypothyroidism in this nursing study guide.
Hypothyroidism
Thyroid deficiency can affect all body functions and can range from mild, subclinical forms to advanced forms.
- Hypothyroidism results from suboptimal levels of thyroid hormone.
- Hypothyroidism also commonly occurs in patients with previous hypothyroidism that has been treated with radioiodine or antithyroid medications or thyroidectomy.
- The term myxedema refers to the accumulation of mucopolysaccharides in subcutaneous and other interstitial tissues.
Classification
The types of hypothyroidism are classified according to their causes:
- Central hypothyroidism. There is a failure of the pituitary gland, the hypothalamus, or both to stimulate production of thyroid hormones.
- Secondary or pituitary hypothyroidism. The cause is entirely a pituitary disorder in secondary hypothyroidism.
- Tertiary or hypothalamic hypothyroidism. This refers to the cause as a disorder of the hypothalamus resulting in inadequate secretion of TSH due to decreased stimulation of TRH.
- The thyroid disorder is already present at birth in cretinism.
Statistics and Epidemiology
Hypothyroidism occurs in specific individuals in different instances.
- Hypothyroidism occurs most frequently in older women.
- There is an increased incidence of thyroid cancer in men who have undergone radiation therapy for head and neck cancer.
- More than 95% of patients with hypothyroidism have primary or thyroidal hypothyroidism.
Causes
Several diseases and factors could cause hypothyroidism.
- The most common cause of hypothyroidism is inflammation of the thyroid gland, which damages the gland’s cells.
- Autoimmune diseases. The most common cause of hypothyroidism in adults is autoimmune thyroiditis or Hashimoto’s disease.
- Atrophy of the thyroid gland. The thyroid gland shrinks in size as a result of aging.
- Therapy for hyperthyroidism. Therapies such as radioactive iodine and thyroidectomy could also cause hypothyroidism.
- Medications such as lithium, iodine compounds, and antithyroid medications could decrease the production of TSH.
- Iodine deficiency or excess. The imbalance in the iodine levels in the body also affects the thyroid gland.
- Autoimmune or Hashimoto’s thyroiditis, in which the immune system attacks the thyroid gland, is the most common example of this.
- Some women develop hypothyroidism after pregnancy (often referred to as “postpartum thyroiditis”).
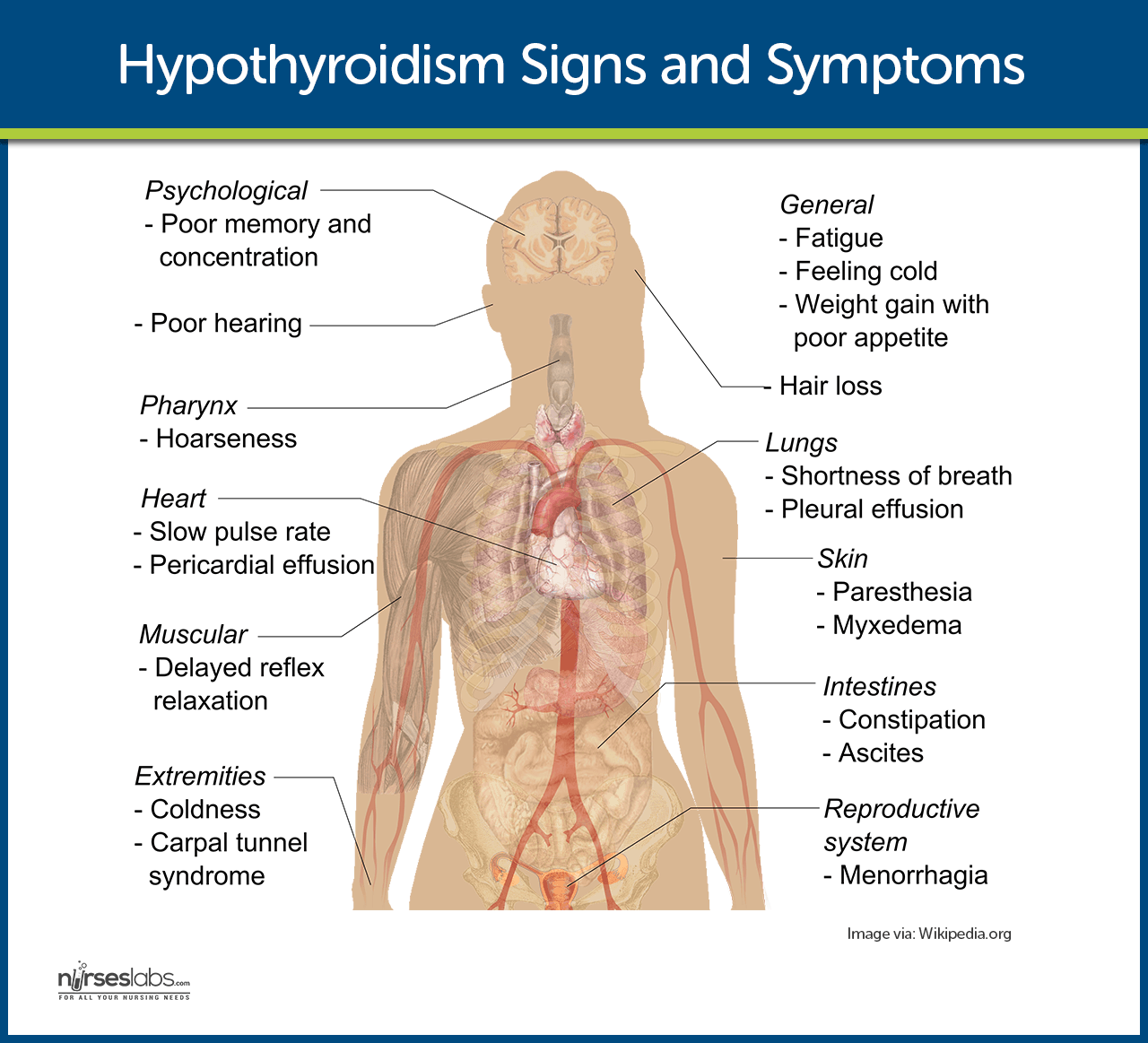
Clinical Manifestations
The signs and symptoms of hypothyroidism include:
- Extreme fatigue. Extreme fatigue makes it difficult for the person to complete a full day’s work or participate in usual activities.
- Menstrual disturbances. Menorrhagia or amenorrhea may also occur.
- Increase in weight. The patient usually begins to gain weight even without an increase in food intake.
- Cold intolerance. The patient often complains of being cold even in a warm environment.
- Thick skin. The skin becomes thickened because of an accumulation of mucopolysaccharides in the subcutaneous tissues.
Prevention
Prevention of hypothyroidism can be achieved with the following:
- Increase in iodine intake. Iodine intake is the foremost prevention strategy in hypothyroidism.
- Early detection. Undergoing thyroid tests after thyroid surgery or therapy could result in early detection and prompt treatment of hypothyroidism.
Complications
Hypothyroidism can be a life-threatening disease if left unchecked.
- Myxedema coma. This is the decompensated state of severe hypothyroidism in which the patient is hypothermic and unconscious.
Assessment and Diagnostic Findings
Hypothyroidism can be detected in many ways.
- Physical examination. The thyroid gland is inspected and palpated routinely in all patients.
- Serum thyroid-stimulating tests. Measurement of the serum TSH concentration is the single best screening test of thyroid function because of its high sensitivity.
- Serum T3 and T4. Measurement of total T3 or T4 includes protein-bound and free hormone levels that occur in response to TSH secretion.
- Thyroid antibodies. Results of testing by immunoassay techniques for antithyroid antibodies are positive in Hashimoto’s thyroiditis (100%).
Medical Management
The primary objective in the management of hypothyroidism is to restore a normal metabolic state by replacing the missing hormone.
- Pharmacologic therapy. Synthetic levothyroxine is the preferred preparation for treating hypothyroidism and suppressing nontoxic goiters.
- Prevention of cardiac dysfunction. As long as metabolism is subnormal and the tissues require relatively little oxygen, a reduction in the blood supply is tolerated without overt symptoms of coronary artery disease.
- Supportive therapy. Oxygen saturation levels should be monitored; fluids should be administered cautiously; application of external heat must be avoided, and oral thyroid hormone therapy should be continued.
Nursing Management
Nursing care for a patient with hypothyroidism includes the following:
Nursing Assessment
Assessment of the patient with hypothyroidism should include:
- Assessment of the thyroid from an anterior or posterior position.
- Auscultation of the lobes of the thyroid gland using the diaphragm of the stethoscope if there are abnormalities palpated.
- Assess thyroid gland for firmness (Hashimoto’s) or tenderness (thyroiditis).
Diagnosis
Based on the assessment data, the nursing diagnoses appropriate for a patient with hypothyroidism are:
- Activity intolerance related to fatigue and depressed cognitive process.
- Risk for imbalanced body temperature related to cold intolerance.
- Constipation related to depressed gastrointestinal function.
- Ineffective breathing pattern related to depressed ventilation.
- Disturbed thought processes related to depressed metabolism and altered cardiovascular and respiratory status.
Planning & Goals
To achieve a successful nursing care plan, the following goals should be realized:
- Increase in participation in activities.
- Increase in independence.
- Maintenance of normal body temperature.
- Return of normal bowel function.
- Improve respiratory status.
- Maintenance of normal breathing pattern.
- Improve thought processes.
Nursing Interventions
Nursing interventions for a patient with hypothyroidism include the following:
- Promote rest. Space activities to promote rest and exercise as tolerated.
- Protect against coldness. Provide extra layer of clothing or extra blanket.
- Avoid external heat exposure. Discourage and avoid the use of external heat source.
- Mind the temperature. Monitor patient’s body temperature.
- Increase fluid intake. Encourage increased fluid intake within the limits of fluid restriction.
- Provide foods high in fiber.
- Manage respiratory symptoms. Monitor respiratory depth, rate, pattern, pulse oximetry, and ABG.
- Pulmonary exercises. Encourage deep breathing, coughing, and use of incentive spirometry.
- Orient to present surroundings. Orient patient to time, place, date, and events around him or her.
Evaluation
A successful nursing care plan has achieved the following goals:
- Increased participation in activities.
- Increased independence.
- Maintained normal body temperature.
- Return of normal bowel function.
- Improved respiratory status.
- Maintained normal breathing pattern.
- Improved thought processes.
Discharge and Home Care Guidelines
At the completion of the home care instruction, the patient or caregiver will be able to:
- Medication compliance. State that compliance to medical regimen is life-long.
- Cold intolerance. State the need to avoid extreme cold temperature until condition is stable.
- Follow-up visits. State the importance of regular follow-up visits with health care provider.
- Weight reduction. Identify strategies for weight reduction and prevention of constipation such as high-fiber, low-calorie intake and adequate fluid intake.
Documentation Guidelines
The focus of documentation should include:
- Level of activity.
- Vital signs before, during, and after activity.
- Record of core temperature, initially and prn.
- Results of laboratory and diagnostic studies.
- Usual and current bowel pattern, duration of the problem, and individual contributing factors.
- Characteristics of stool.
- Respiratory pattern, breath sounds, and use of accessory muscles.
- Plan of care.
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcomes.
- Modifications to plan of care.
- Long term needs.
See Also
Posts related to this study guide:













Leave a Comment