Congenital hypothyroidism is a critical and relatively common endocrine disorder that affects newborns, resulting from an underactive thyroid gland since birth. This condition occurs when the thyroid gland fails to produce an adequate amount of thyroid hormones, essential for normal growth and development.
Without early detection and prompt intervention, congenital hypothyroidism can lead to significant developmental delays and intellectual disabilities
What is Congenital Hypothyroidism?
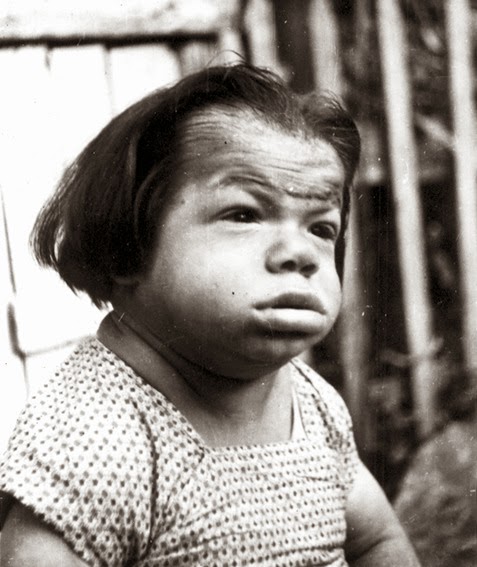
- At one time referred to by the now unacceptable term “cretinism“, congenital hypothyroidism is associated with either the congenital absence of a thyroid gland or the inability of the thyroid gland to secrete thyroid hormone.
- It can occur because of an anatomic defect in the gland, an inborn error in thyroid metabolism, or iodine deficiency.
- Lower TSH screening cutoffs may also be driving this increase in diagnosis, although altered ethnicities of the screened population, increased multiple and premature births, and iodine status are contributing factors.
- In the 1920s, adequate dietary intake of iodine was found to prevent endemic goiter and cretinism.
- The term sporadic cretinism was initially used to describe the random occurrence of cretinism in nonendemic areas; the cause of these abnormalities was identified as nonfunctioning or absent thyroid glands.
Pathophysiology
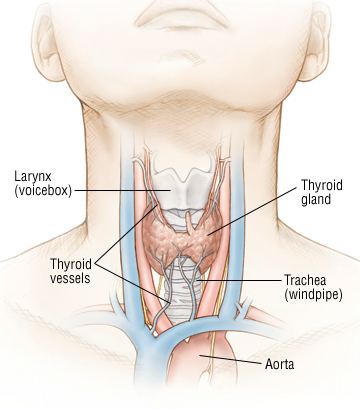
The thyroid gland develops from the buccopharyngeal cavity between 4 and 10 weeks gestation.
- The thyroid arises from the fourth branchial pouches and ultimately ends up as a bilobed organ in the neck.
- By 10-11 weeks gestation, the fetal thyroid is capable of producing thyroid hormone; by 18-20 weeks gestation, blood levels of T4 have reached term levels.
- The thyroid gland uses tyrosine and iodine to manufacture T4 and triiodothyronine (T3).
- Inborn errors of thyroid metabolism can result in congenital hypothyroidism in children with anatomically normal thyroid glands.
- T4 is the primary thyronine produced by the thyroid gland; only 10-40% of circulating T3 is released from the thyroid gland.
- T3 is the primary mediator of the biological effects of thyroid hormone and does so by interacting with a specific nuclear receptor; receptor abnormalities can result in thyroid hormone resistance.
- The major carrier proteins for circulating thyroid hormones are thyroid-binding globulin (TBG), thyroid-binding prealbumin (TBPA), and albumin.
- Infants born with low levels of TBG, as in congenital TBG deficiency, have low total T4 levels but are physiologically normal; familial congenital TBG deficiency can occur as an X-linked recessive or autosomal recessive condition.
- The most critical period for the effect of thyroid hormone on brain development is the first few months of life.
Statistics and Incidences
CH is the most common neonatal endocrine disorder, and historically, thyroid dysgenesis was thought to account for approximately 80% of cases.
- An increased incidence of congenital hypothyroidism is observed in twins; twin births are approximately 12 times as likely to have congenital hypothyroidism as singletons.
- Usually, only one twin is hypothyroid, but a common in-utero exposure can cause hypothyroidism in both.
- Most studies of congenital hypothyroidism suggest a female-to-male ratio of 2:1; Devos et al showed that much of the discrepancy is accounted for by infants with thyroid ectopy.
- In central Africa, where iodine deficiency occurs along with excess dietary cyanate from cassava (Manihot esculenta), as many as 10% of newborns may have both low cord blood T4 concentration and TSH concentrations over 100 mU/L.
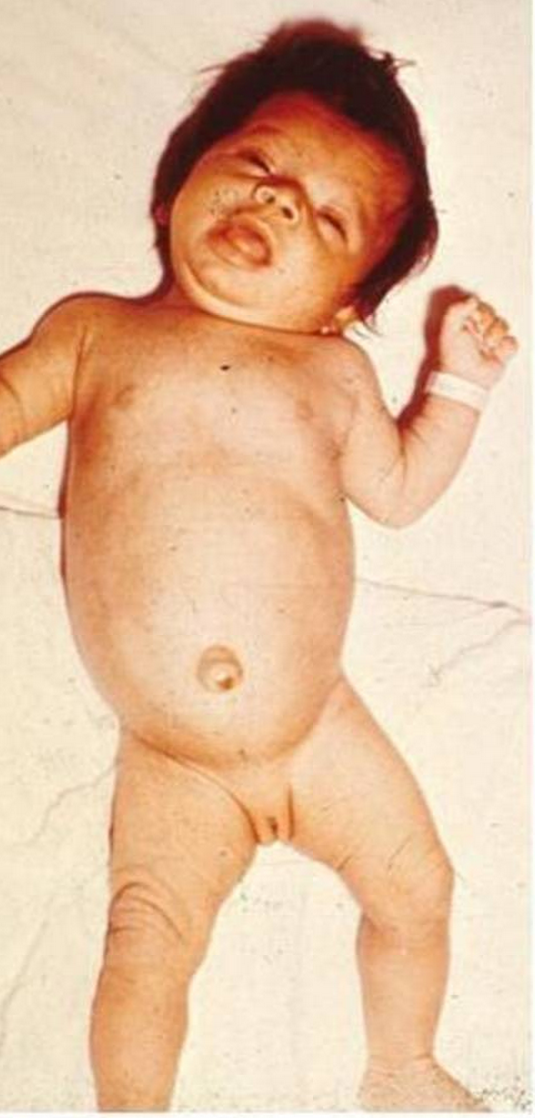
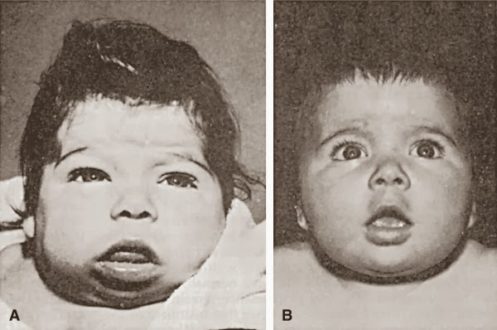
Clinical Manifestations
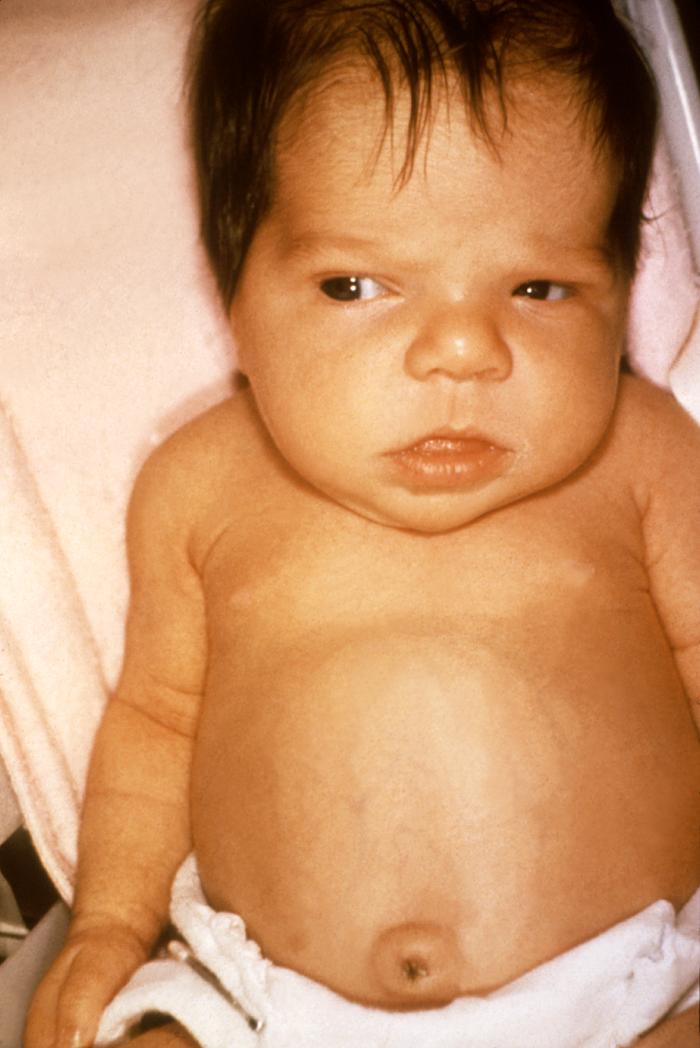
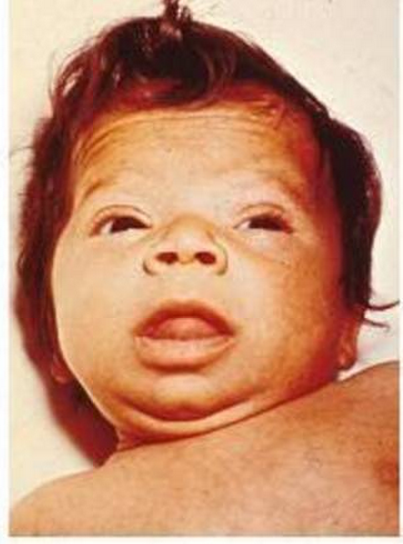
The physical findings of hypothyroidism may or may not be present at birth.
- Decreased activity. Often, affected infants are described as “good babies” because they rarely cry and they sleep most of the time.
- Large anterior fontanelle. A large anterior fontanelle is mostly found in infants with CH, with delayed closure.
- Poor feeding and weight gain. A child with CH mostly sleeps and rarely feeds, resulting in poor weight gain.
- Small stature or poor growth. There is a delay in the development of children with CH, with poor growth as one of the findings.
- Jaundice. The yellow coloration of the skin and sclera in newborns with jaundice is the result of the accumulation of unconjugated bilirubin.
Assessment and Diagnostic Findings
Diagnosis of primary hypothyroidism is confirmed by demonstrating decreased levels of serum thyroid hormone (total or free T4) and elevated levels of thyroid-stimulating hormone (TSH).
- Newborn screening. Screening for congenital hypothyroidism is recommended when a baby is 3 days old; testing should be performed before discharge or within 7 days of birth; false-positive TSH elevations may be found in specimens collected at 24-48 hours after birth, and false-negative results may be found in critically ill newborns or post-transfusion infants.
- T4 levels. Low or low-normal serum total T4 levels in the setting of a serum TSH within the reference range suggests TBG deficiency; this congenital disorder causes no pathologic consequence; however, it should be recognized to avoid unnecessary thyroid hormone administration.
- Ultrasonography and scintigraphy. Ultrasound and thyroid scintigraphy help determine the anatomy and function of the thyroid gland as well as the etiology of congenital hypothyroidism; ultrasound lacks sensitivity for detecting small ectopic glands but is the gold standard for measuring thyroid dimensions; scintigraphy (using technetium-99m or iodine-123) provides an etiologic diagnosis in most cases and can aid in distinguishing congenital hypothyroidism from transient hyperthyrotropinemia.
- Radiography. A lateral radiograph of the knee may be obtained to look for the distal femoral epiphysis; this ossification center appears at about 36 weeks gestation; its absence in a term or post-term infant indicates prenatal effects of hypothyroidism.
Medical Management
The thyroid hormone must be replaced as soon as the diagnosis is made. The goal of treatment in congenital hypothyroidism is to correct hypothyroidism and ensure normal growth and neuropsychological development.
- Levothyroxine. Only levothyroxine is recommended for treatment; it has been established as safe, effective, inexpensive, easily administered, and easily monitored.
- Diet. Dietary iodide supplementation in iodine-deficient areas can prevent endemic cretinism but does not have a major effect on sporadic congenital hypothyroidism; soy-based formulas may decrease the absorption of levothyroxine; this is not a contraindication to their use, even in infants with congenital hypothyroidism; switching an infant from a milk-based formula to a soy-based formula may increase the dose of thyroid hormone needed to maintain a euthyroid status.
Pharmacologic Management
The drug of choice for CH is only Levothyroxine.
- Thyroid hormones. These agents are administered to supplement thyroid hormones in patients with hypothyroidism. Levothyroxine is the preferred form of thyroid hormone replacement in all patients with hypothyroidism.
Nursing Management
Nursing care for a child with congenital hypothyroidism includes the following:
Nursing Assessment
Assessment of a child with congenital hypothyroidism include:
- History. Family history should be carefully reviewed for information about similarly affected infants or family members with unexplained mental retardation; maternal history of a thyroid disorder and mode of treatment, whether before or during pregnancy, can occasionally provide the etiology of the infant’s problem.
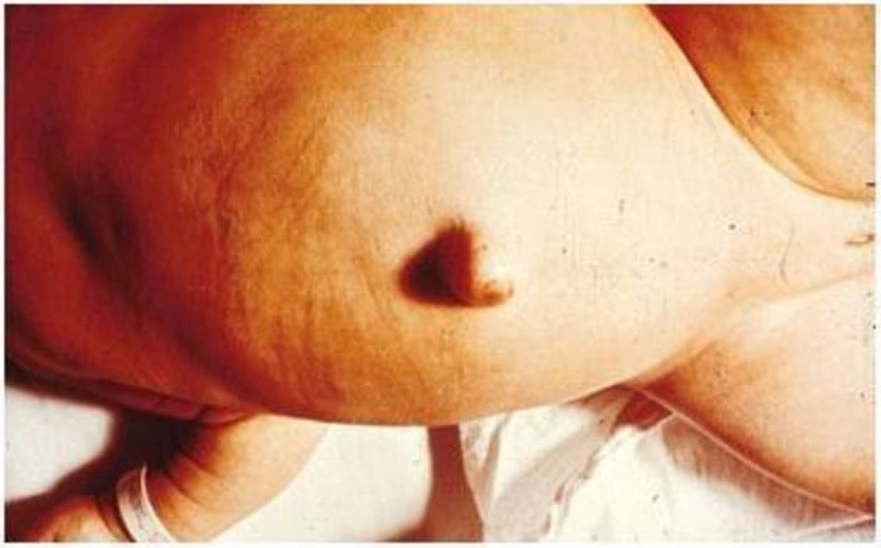
- Physical exam. Physical exam may show signs of coarse facial features, macroglossia, large fontanelles, umbilical hernia, developmental delay, pallor, myxedema, and goiter.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnosis for congenital hypothyroidism are:
- Imbalanced nutrition: more than body requirements related to greater intake than metabolic needs as evidenced by hypotonia or decreased activity level.
- Deficient knowledge related to lack of exposure to hypothyroidism and unfamiliarity with information sources.
- Fatigue related to impaired metabolic state.
Nursing Care Planning and Goals
Main Article: 3 Hypothyroidism Nursing Care Plans
The major nursing care planning goals for congenital hypothyroidism are:
- Client will maintain a stable weight and takes in necessary nutrients.
- Family members/caregivers will verbalize correct information about hypothyroidism and taking thyroid hormone replacement.
- Family members/caregivers will identify the basis of fatigue and individual areas of control.
- Family members/caregivers will verbalize reduction of fatigue and increased ability to complete desired activities.
Nursing Interventions
The nursing interventions are:
- Maintain a stable weight. Educate the client and family regarding body weight changes in hypothyroidism; collaborate with a dietician to determine client’s caloric needs; encourage the intake of foods rich in fiber; encourage a low-cholesterol, low-calorie, low-saturated-fat diet.
- Learn more about the disease. Provide information about hypothyroidism; educate the client and family regarding thyroid hormones; emphasize the importance of rest periods.
- Reduce fatigue. Note daily energy patterns; plan care to allow individually adequate rest periods; schedule activities for periods when the client has the most energy; promote an environment conducive to relieve fatigue.
Evaluation
Goals are met as evidenced by:
- Client maintained a stable weight and takes in necessary nutrients.
- Family members/caregivers verbalized correct information about hypothyroidism and taking thyroid hormone replacement.
- Family members/caregivers identified basis of fatigue and individual areas of control.
- Family members/caregivers verbalized reduction of fatigue and increased ability to complete desired activities.
Documentation Guidelines
Documentation in a child with congenital hypothyroidism includes:
- Individual findings include factors affecting, interactions, the nature of social exchanges, and specifics of individual behavior.
- Intake and output.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.



























Leave a Comment