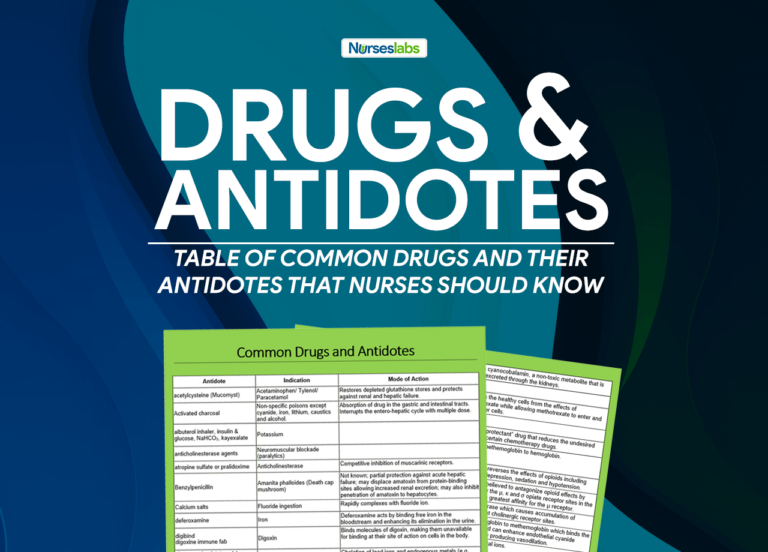
An antidote is a substance that can counteract a form of poisoning. The term antidote is a Greek word meaning “given against”. This post will help you familiarize yourself with the common antidotes that are used in the hospital setting. The following are antidotes that should be familiarized by the nurse to respond to this emergency situation quickly.
Table of Antidotes
| Antidote | Indication | Mode of Action |
|---|---|---|
| acetylcysteine (Mucomyst) | Acetaminophen/ Tylenol/ Paracetamol | Restores depleted glutathione stores and protects against renal and hepatic failure. |
| Activated charcoal | Non-specific poisons except cyanide, iron, lithium, caustics and alcohol. | Absorption of drug in the gastric and intestinal tracts. Interrupts the entero-hepatic cycle with multiple dose. |
| albuterol inhaler, insulin & glucose, NaHCO3, kayexalate | Potassium | |
| anticholinesterase agents | Neuromuscular blockade (paralytics) | |
| atropine sulfate or pralidoxime | Anticholinesterase | Competitive inhibition of muscarinic receptors. |
| Benzylpenicillin | Amanita phalloides (Death cap mushroom) | Not known; partial protection against acute hepatic failure; may displace amatoxin from protein-binding sites allowing increased renal excretion; may also inhibit penetration of amatoxin to hepatocytes. |
| Calcium salts | Fluoride ingestion | Rapidly complexes with fluoride ion. |
| deferoxamine | Iron | Deferoxamine acts by binding free iron in the bloodstream and enhancing its elimination in the urine. |
| digibind digoxine immune fab |
Digoxin | Binds molecules of digoxin, making them unavailable for binding at their site of action on cells in the body. |
| dimercapol, edetate calcium, disodium, | Lead | Chelation of lead ions and endogenous metals (e.g., zinc, manganese, iron, copper). |
| diphenhydramine (Benadryl) | Extrapyramidal symptoms (EPS) | A potent antagonist to acetylcholine in muscarinic receptors. |
| flumazenil | Benzodiazepines | Reverses the effects of benzodiazepines by competitive inhibition at the benzodiazepine binding site on the GABAA receptor. |
| fomepizole | Ethylene glycol | A competitive inhibitor of the enzyme alcohol dehydrogenase found in the liver. This enzyme plays a key role in the metabolism of ethylene glycol and methanol. |
| glucagon | Beta blockers and calcium channel blockers | Stimulates the formation of adenyl cyclase causing intracellular increase in cycling AMP and enhanced glycogenolysis and elevated serum glucose concentration. |
| Glucose (Dextrose 50%) | Insulin reaction | Dextrose (the monosaccharide glucose) is used, distributed and stored by body tissues and is metabolized to carbon dioxide and water with the release of energy. |
| Heparin | Ergotamine | Reverses hypercoagulable state by interacting with antithrombin III. Used in combination with vasodilator phentolamine or nitroprusside to prevent local thrombosis and ischemia. |
| Hydroxocobalamin | Cyanide | Forms cyanocobalamin, a non-toxic metabolite that is easily excreted through the kidneys. |
| leucovorin calcium | Fluorouracil | |
| Methotrexate | Protects the healthy cells from the effects of methotrexate while allowing methotrexate to enter and kill cancer cells. | |
| Magnesium sulfate | calcium gluconate | |
| mesna | Cyclophosphamide | A “chemoprotectant” drug that reduces the undesired effects of certain chemotherapy drugs. |
| Methylene blue | Chemical producing severe methemoglobinemia. Ifosamide-induced encephalopathy. | Reduces methemoglobin to hemoglobin. |
| nalmefene or naloxone | Opioid analgesics | Prevents or reverses the effects of opioids including respiratory depression, sedation and hypotension. |
| naloxone (Narcan) | Narcotics | Naloxone is believed to antagonize opioid effects by competing for the µ, κ and σ opiate receptor sites in the CNS, with the greatest affinity for the µ receptor. |
| Neostigmine | Anticholinergics | Anticholinesterase which causes accumulation of acetylcholine at cholinergic receptor sites. |
| Nitrite, sodium and glycerytrinitrate | Cyanide | Oxidizes hemoglobin to methemoglobin which binds the free cyanide and can enhance endothelial cyanide detoxification by producing vasodilation. |
| Penicillamine | Copper, gold, lead, mercury, zinc, arsenic | Chelation of metal ions. |
| phentolamine (Regitine) | Dopamine | Regitine produces an alpha-adrenergic block of relatively short duration. It also has direct, but less marked, positive inotropic and chronotropic effects on cardiac muscle and vasodilator effects on vascular smooth muscle. |
| phyostigmine or NaHCO3 | Tricyclic antidepressants | A reversible anticholinesterase which effectively increases the concentration of acetylcholine at the sites of cholinergic transmission. |
| Phytomenadione (Vitamin K.) | Coumadin/Warfarin | Bypasses inhibition of Vitamin K epoxide reductase enzyme. |
| protamine sulfate | Heparin | Protamine that is strongly basic combines with acidic heparin forming a stable complex and neutralizes the anticoagulant activity of both drugs. |
| Pyridoxine | Isoniazid, theophylline, monomethyl hydrazine. Adjunctive therapy in ethylene glycol poisoning. | Reverses acute pyridoxine deficiency by promoting GABA synthesis. Promotes the conversion of toxic metabolite glycolic acid to glycine. |
| Snake anti-venin | Cobra bite | Neutralizes venom by binding with circulating venom components and with locally deposited venom by accumulating at the bite site. |
| Sodium Bicarbonate | Iron | Prevents convertion of ferrous to ferric. |
| Cardiotoxic drug affecting fast sodium channel (TCA, cocaine) | Decreases affinity of cardiotoxic drugs to the fast sodium channel. | |
| Weak acids | Promotes ionization of weak acids. | |
| Chlorine gas inhalational poisoning | Neutralization of hydrochloric acid formed when chlorine gas reacts with water in the airways. | |
| Sodium thiosulphate | Cyanide | Replenishes depleted thiosulphate stores by acting as sulfur donor necessary for the conversion of CN-O to thiocyanate through the action of sulfur transferase enzyme rhodanese. |
| Thiamine | Alcohol, Wernicke-Korsakoff Syndrome | Reverses acute thiamine deficiency |
| Adjunctive in ethylene glycol | Enhances detoxification of glyoxylic acid. | |
| Vitamin C | Chemicals causing methemoglobinemia in patients with G6PD deficiency | Reduces methemoglobin to hemoglobin. |
Recommended Resources
Our recommended nursing pharmacology resources and books:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase which will help support us. Thank you! For more information, check out our privacy policy.
Pharm Phlash! Pharmacology Flash Cards #1 BEST SELLER!
Test-yourself review cards put critical clinical information for nearly 400 of the top generic medications at your fingertips. And, you can count on them for accuracy, because each card is based on content from Davis’s Drug Guide for Nurses. Increase your test scores in pharmacology class.
Focus on Pharmacology (8th Edition)
Focus on Nursing Pharmacology makes challenging concepts more approachable. Engaging learning features cultivate your clinical application, critical thinking and patient education capabilities. This updated 8th edition builds on your knowledge of physiology, chemistry and nursing fundamentals to help you conceptualize need-to-know information about each group of drugs.
Pharmacology Made Incredibly Easy (Incredibly Easy! Series®)
Nursing pharmacology guide offers step-by-step guidance so you can grasp the fundamentals in enjoyable Incredibly Easy style. This is the perfect supplement to class materials, offering solid preparation for NCLEX® as well as a handy refresher for experienced nurses. Colorfully illustrated chapters offer clear, concise descriptions of crucial nursing pharmacology concepts and procedures.
Lehne’s Pharmacology for Nursing Care (11th Edition)
The Eleventh Edition of Lehne’s Pharmacology for Nursing Care provides a thorough understanding of key drugs and their implications for nursing care. This text, written by renowned nursing educators, helps you comprehend and apply pharmacology principles. A clear and engaging writing style simplifies complex concepts, making even the most challenging pharmacology content enjoyable. We recommend this book if you want a comprehensive nursing pharmacology guide.
Nursing Drug Handbook
Nursing2023 Drug Handbook delivers evidence-based, nursing-focused drug monographs for nearly 3700 generic, brand-name, and combination drugs. With a tabbed, alphabetical organization and a “New Drugs” section, NDH2023 makes it easy to check drug facts on the spot.

Pharmacology and the Nursing Process
The 10th edition of Pharmacology and the Nursing Process offers practical, user-friendly pharmacology information. The photo atlas contains over 100 unique illustrations and photographs depicting drug administration techniques. Updated drug content reflects the most recent FDA drug approvals, withdrawals, and therapeutic uses.

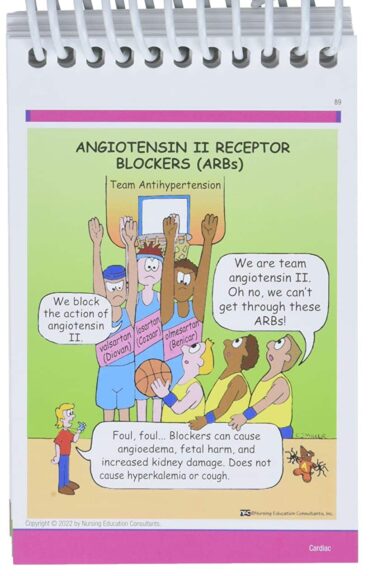
Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, and Memory Aids for Nurses
The 6th edition of Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, & Memory Aids for Nurses incorporates illustrations and humor to make studying easier and more enjoyable. This unique pharmacology review can be utilized as a spiral-bound notebook or as individual flashcards, making it ideal for mobile study.
See Also
Here are other nursing pharmacology study guides:
- Nursing Pharmacology – Study Guide for Nurses
Our collection of topics related to nursing pharmacology - Pharmacology Nursing Mnemonics & Tips
These nursing mnemonics aim to simplify the concepts of pharmacology through the use of a simple, concise guide. - Generic Drug Name Stems Cheat Sheet
Learn about these generic drug name stems to help you make sense of drugs easier! - Common Drugs and Their Antidotes
A guide to drug antidotes that nurses should be familiar about. - IV Fluids and Solutions Guide & Cheat Sheet
Get to know the different types of intravenous solutions or IV fluids in this guide and cheat sheet. - Drug Dosage Calculations NCLEX Practice Questions (100+ Items)
Care to take the challenge? This quiz aims to help students and registered nurses alike grasp and master the concepts of medication calculation.
Drug Guides NEW!
Individual drug guides and nursing considerations for the most common medications used in nursing pharmacology:
- Acetaminophen (Tylenol)
- Aspirin
- Atorvastatin (Lipitor)
- Enoxaparin (Lovenox)
- Furosemide (Lasix)
- Gabapentin
- Hydromorphone (Dilaudid)
- Lisinopril
- Metoprolol
- Morphine
Gastrointestinal System Drugs
Respiratory System Drugs
- Antihistamines
- Bronchodilators and Antiasthmatics
- Decongestants
- Expectorants and Mucolytics
- Inhaled Steroids
- Lung Surfactants
Endocrine System Drugs
- Adrenocortical Agents
- Antidiabetic Agents
- Glucose-Elevating Agents
- Hypothalamic Agents
- Insulin
- Parathyroid Agents: Bisphosphonates, Calcitonins
- Pituitary Drugs
- Sulfonylureas
- Thyroid Agents
Autonomic Nervous System Drugs
- Adrenergic Agonists (Sympathomimetics)
- Adrenergic Antagonists (Sympatholytics)
- Anticholinergics (Parasympatholytics)
- Cholinergic Agonists (Parasympathomimetics)
Immune System Drugs
Chemotherapeutic Agents
- Anthelmintics
- Anti-Infective Drugs
- Antibiotics
- Antifungals
- Antineoplastic Agents
- Antiprotozoal Drugs
- Antiviral Drugs
Reproductive System Drugs
Nervous System Drugs
- Antidepressants
- Antiparkinsonism Drugs
- Antiseizure Drugs
- Anxiolytics and Hypnotic Drugs
- General and Local Anesthetics
- Muscle Relaxants
- Narcotics, Narcotic Agonists, and Antimigraine Agents
- Neuromuscular Junction Blocking Agents
- Psychotherapeutic Drugs
Cardiovascular System Drugs
a.a.can u please send me some guidelines for the establishment of poison contrl center in a hospital?
thanks
can u please send me all natidote for all drugs thanks
Magnesium sulfate – calcium gluconate… to add in the list :)
Would anyone post Drug of choice for specific disease or condition here. thanks :)
Exellent job, thanks
Antidote for Heparin is Protamine SO4 right?
Hey Matt!
I was wondering if the printable cheat sheet for this is still available.
How can I download this as a pdf or some easily printable format?
I’m wondering too!
Matt, you cannot imagine how helpful your work is for all us student nurses. Thanks a ton, I wish you all the best in life.
so helpful, thank you
I am interested in developing generic form of Antidotes to avoid the fatal effects of drug abuse. It will be nice if the names of a few of such antidotes drug substances can be shared.
Will also look at the possibilities of development of the drug substances reported in this list at low cost.