Lisinopril is a medication commonly used to treat hypertension (high blood pressure) and heart failure. As a nurse, there are several important nursing considerations to keep in mind when administering lisinopril or caring for patients who are taking this medication.
What is Lisinopril?
Lisinopril is a medication that belongs to a class of drugs known as angiotensin-converting enzyme (ACE) inhibitors. It is commonly used to treat hypertension (high blood pressure) and heart failure. Lisinopril works by relaxing the blood vessels, which helps to lower blood pressure and improve blood flow to the heart. It is typically taken orally once a day, with or without food. As with any medication, lisinopril may cause side effects, including dizziness, cough, and hypotension (low blood pressure). It is important to follow the instructions of a healthcare provider when taking lisinopril and to report any potential side effects.
Generic Name
- lisinopril
Brand Names
Lisinopril is sold under various brand names, including:
- Prinivil
- Zestril
- Qbrelis
- Acerbon
- Carace
- Diroton
- Lisihexal
- Lisinocomp
- Lysinoton
Drug Classification of Lisinopril
The drug classification of lisinopril is:
Therapeutic Class
Pharmacologic Class
Indications and Therapeutic Effects
Lisinopril is primarily indicated for the treatment of hypertension (high blood pressure) and heart failure. However, there are several other conditions for which lisinopril may be used. Below is a list of indications for lisinopril:
1. Hypertension. Lisinopril is commonly used to treat hypertension, which is a condition characterized by elevated blood pressure. Lisinopril works by relaxing the blood vessels, which helps to lower blood pressure and improve blood flow.
2. Heart failure. Lisinopril is also used to treat heart failure, which is a condition in which the heart is unable to pump enough blood to meet the body’s needs. Lisinopril helps to improve heart function and reduce the risk of hospitalization due to heart failure.
3. Acute myocardial infarction. Lisinopril may be used to improve survival after a heart attack (acute myocardial infarction). It is typically given to patients who have had a heart attack within the past 24 hours, and it may be continued for several weeks after the event.
4. Diabetic nephropathy. Lisinopril is sometimes used to manage diabetic nephropathy, which is a type of kidney disease that occurs in patients with diabetes and high blood pressure. Lisinopril helps to reduce the risk of kidney failure and other complications of diabetic nephropathy.
5. Migraine prophylaxis. Lisinopril has been used off-label for the prevention of migraines. It is thought to work by reducing blood pressure and improving blood flow to the brain.
Mechanism of Action
Lisinopril is a medication that belongs to a class of drugs known as angiotensin-converting enzyme (ACE) inhibitors. Its mechanism of action involves inhibiting the activity of ACE, an enzyme that is responsible for converting angiotensin I into angiotensin II. Angiotensin II is a potent vasoconstrictor, which means that it causes the blood vessels to narrow and increases blood pressure. By inhibiting ACE, lisinopril helps to reduce the production of angiotensin II, which leads to the relaxation of blood vessels and a decrease in blood pressure. Additionally, lisinopril may also improve blood flow to the heart and other organs, which can help to reduce the risk of heart failure and other cardiovascular complications.
Precautions and Contraindications
Here is a list of precautions and contraindications for lisinopril:
Precautions
1. Hypotension. Lisinopril may cause hypotension (low blood pressure), especially in patients who are volume-depleted, have renal impairment, or are taking other medications that lower blood pressure. Blood pressure should be monitored regularly during treatment with lisinopril.
2. Renal impairment. Lisinopril is primarily excreted by the kidneys, and it may accumulate in patients with renal impairment. Dosage adjustments may be necessary in patients with impaired renal function.
3. Hyperkalemia. Lisinopril may increase potassium levels in the blood, particularly in patients with renal impairment or those taking other medications that increase potassium levels. Blood potassium levels should be monitored regularly.
4. Angioedema. Lisinopril may cause angioedema, a potentially life-threatening swelling of the face, lips, tongue, or throat. Patients with a history of angioedema should not take lisinopril.
5. Pregnancy and breastfeeding. Lisinopril may cause harm to a developing fetus, and it should not be used during pregnancy. It is also not recommended for use during breastfeeding.
6. Surgery and anesthesia. Lisinopril should be discontinued prior to surgery or anesthesia, as it may increase the risk of hypotension.
Contraindications
1. History of angioedema. Lisinopril is contraindicated in patients with a history of angioedema, a potentially life-threatening swelling of the face, lips, tongue, or throat.
2. Hypersensitivity. Lisinopril is contraindicated in patients who have had a hypersensitivity reaction to any ACE inhibitor.
3. Pregnancy. Lisinopril is contraindicated in pregnancy, as it may cause harm to a developing fetus.
4. Bilateral renal artery stenosis. Lisinopril is contraindicated in patients with bilateral renal artery stenosis, a condition in which the arteries that supply blood to the kidneys become narrowed.
Drug Interactions
When administering lisinopril, the nurse should consider the following drug interactions:
Drug-Drug
Here is a list of drug interactions of lisinopril:
1. Diuretics. Taking lisinopril with diuretics (water pills) may increase the risk of hypotension (low blood pressure) and electrolyte imbalances such as hyperkalemia (high potassium levels in the blood).
2. Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs such as ibuprofen and naproxen may reduce the effectiveness of lisinopril and increase the risk of renal dysfunction (kidney problems).
3. Potassium-sparing diuretics and potassium supplements. Taking lisinopril with potassium-sparing diuretics or potassium supplements may increase the risk of hyperkalemia.
4. Lithium. Lithium toxicity may occur in patients taking lisinopril and lithium due to decreased renal excretion of lithium.
5. Antidiabetic agents. Lisinopril may enhance the hypoglycemic effects of antidiabetic agents, including insulin and oral hypoglycemic agents.
6. Gold. Concomitant use of lisinopril and gold compounds may increase the risk of neutropenia (low white blood cell count).
7. Other antihypertensive agents. Combining lisinopril with other antihypertensive agents may increase the risk of hypotension.
Drug-Natural Products
Here is a list of potential drug-natural product interactions with lisinopril:
1. Potassium supplements. Natural products high in potassium, such as potassium supplements or potassium-rich foods like bananas, may increase the risk of hyperkalemia when taken with lisinopril.
2. Salt substitutes. Some salt substitutes contain potassium and using them while taking lisinopril may also increase the risk of hyperkalemia.
3. Herbal supplements. Herbal supplements with blood pressure-lowering effects, such as garlic, ginger, or hawthorn, may increase the risk of hypotension when taken with lisinopril.
4. Grapefruit juice. Grapefruit juice may increase the levels of lisinopril in the blood, which can lead to an increased risk of side effects.
5. St. John’s Wort. St. John’s Wort may reduce the effectiveness of lisinopril by increasing its breakdown in the liver.
6. Ginseng. Ginseng may increase blood pressure and should be used with caution in patients taking antihypertensive medications like lisinopril.
7. Coenzyme Q10 (CoQ10). CoQ10 may reduce blood pressure and should be used with caution in patients taking antihypertensive medications like lisinopril.
Drug-Food
Here is a list of potential drug-food interactions with lisinopril:
1. Grapefruit juice. Drinking grapefruit juice may increase the levels of lisinopril in the blood, which can lead to an increased risk of side effects.
2. Foods high in potassium. Eating foods high in potassium, such as bananas and leafy greens, may increase the risk of hyperkalemia when taken with lisinopril.
3. Alcohol. Drinking alcohol while taking lisinopril may increase the risk of hypotension (low blood pressure) and should be avoided.
4. Tyramine-rich foods. Tyramine-rich foods, such as aged cheeses, cured meats, and some fermented foods, may interact with lisinopril and increase the risk of hypertensive crisis (sudden, severe high blood pressure).
5. Caffeine. Consuming large amounts of caffeine may increase blood pressure and should be used with caution in patients taking antihypertensive medications like lisinopril.
Adverse Effects
Here is a list of potential side effects and adverse reactions of lisinopril:
1. Hypotension (low blood pressure). This is a common side effect of lisinopril and may cause dizziness, lightheadedness, and fainting.
2. Hyperkalemia (high levels of potassium in the blood). This can be a serious side effect of lisinopril and may cause weakness, fatigue, and abnormal heart rhythms.
3. Angioedema. This is a rare but potentially serious adverse reaction to lisinopril, which can cause swelling of the face, lips, tongue, or throat and may require emergency medical attention.
4. Cough. Lisinopril can cause a persistent dry cough in some patients, which may require discontinuation of the medication.
5. Rash. Lisinopril can cause a skin rash or itching in some patients, which may be a sign of an allergic reaction.
6. Renal impairment. Lisinopril can cause renal impairment, especially in patients with preexisting kidney disease.
7. Neutropenia (low levels of white blood cells). This is a rare but potentially serious adverse reaction to lisinopril, which can increase the risk of infections.
8. Hepatotoxicity (liver damage). Lisinopril can cause liver damage in rare cases, especially in patients with preexisting liver disease.
9. Sexual dysfunction. Lisinopril can cause sexual dysfunction in some patients, including erectile dysfunction and decreased libido.
Administration Considerations
Available Forms
Lisinopril is available in the following forms:
- Oral solution: 1 mg/mL.
- Tablets: 2.5 mg, 5 mg, 10 mg, 20 mg, 30 mg, 40 mg.
- In combination with: hydrochlorothiazide (Prinzide, Zestoretic).
Dosage for Children
- PO (Children ≥6 yr)
- Hypertension. 0.07 mg/kg once daily (up to 5 mg/day), may be titrated every 1 – 2 wk up to 0.6 mg/kg/day (or 40 mg/day).
- Renal Impairment. CCr <30 mL/min — Contraindicated.
Dosage for Adults
- PO (Adults)
- Hypertension. 10 mg once daily, can be increased up to 20 – 40 mg/day (initiate therapy at 5 mg/day in patients receiving diuretics)
- HF. 5 mg once daily; may be titrated every 2 wk up to 40 mg/day; begin with 2.5 mg once daily in patients with hyponatremia (serum sodium <130 mEq/L)
- Post-MI. 5 mg once daily for 2 days, then 10 mg daily.
- Renal Impairment. CCr 10 – 30 mL/min — Begin with 5 mg once daily; may be slowly titrated up to 40 mg/day; CCr <10 ml/min — Begin with 2.5 mg once daily; may be slowly titrated up to 40 mg/day.
Pharmacokinetics
Lisinopril is a medication used to treat hypertension and heart failure. Its pharmacokinetics describes how the drug is absorbed, distributed, metabolized, and excreted in the body.
1. Absorption. Lisinopril is well absorbed when taken orally, with a bioavailability of approximately 25%. It reaches peak plasma concentrations within 7 hours of oral administration.
2. Distribution. Lisinopril is widely distributed throughout the body, including to the heart, kidneys, liver, and lungs. It is not highly protein-bound, with approximately 10% binding to plasma proteins.
3. Metabolism and Excretion. Lisinopril is not extensively metabolized in the liver and is primarily eliminated unchanged in the urine. Its elimination half-life is approximately 12 hours.
4. Half-life. The half-life of lisinopril is approximately 12 hours, meaning that it takes about 12 hours for the concentration of the drug in the body to be reduced by half.
5. Protein-Binding. Lisinopril is minimally protein-bound, with only about 10% binding to plasma proteins.
Overall, lisinopril is well-absorbed when taken orally, is widely distributed throughout the body, and is primarily eliminated unchanged in the urine with a half-life of approximately 12 hours.
Nursing Considerations for Lisinopril
As a nurse, it is important to be aware of nursing considerations when administering lisinopril. Here are some important nursing considerations for lisinopril:
Nursing Assessment
It is important to perform a thorough nursing assessment of patients taking lisinopril. Here are some nursing assessments to consider:
1. Monitor the patient’s vital signs such as the patient’s blood pressure, heart rate, and respiratory rate before and after the administration of lisinopril.
It is important to monitor the patient’s vital signs when taking lisinopril to ensure that blood pressure is properly controlled and to identify any potential adverse reactions to the medication.
2. Assess the patient’s renal function before initiating therapy with lisinopril, and monitor their serum creatinine and blood urea nitrogen levels regularly.
Lisinopril can cause renal impairment, especially in patients with pre-existing kidney disease, and monitoring renal function can help prevent further renal damage.
3. Obtain a complete medical history, including allergies, previous adverse reactions to medications, and any pre-existing medical conditions that may be contraindicated for lisinopril use.
Lisinopril may be contraindicated in patients with certain medical conditions, such as a history of angioedema or renal disease, and the medical history can help guide appropriate prescribing and monitoring of the medication.
4. Obtain a complete medication history, including over-the-counter medications, supplements, and herbal remedies, to check for drug interactions with lisinopril.
Lisinopril may interact with other medications, such as diuretics or potassium supplements, and the medication history can help guide appropriate prescribing and monitoring of the medication.
5. Assess the patient for symptoms of hypertension or heart failure, such as shortness of breath, chest pain, and fatigue.
Assessing the patient for symptoms of hypertension or heart failure when taking lisinopril is important because these symptoms may indicate the need for additional medication or a change in the current treatment plan, and may also suggest potential adverse reactions to the medication.
6. Monitor the patient’s electrolyte levels, especially potassium, as lisinopril can cause hyperkalemia.
It is important to monitor the patient’s electrolyte levels, especially potassium, when taking lisinopril because the medication can cause hyperkalemia, which can lead to serious cardiac complications, and monitoring electrolyte levels can help prevent these complications.
7. Assess the patient for symptoms of angioedema, such as swelling of the face, lips, tongue, or throat.
Assessing the patient for symptoms of angioedema when taking lisinopril is important because the medication can cause this serious allergic reaction, which can be life-threatening, and early identification of symptoms can lead to prompt treatment and prevent further complications.
8. Assess the patient’s compliance with lisinopril therapy, including the dosing schedule and any missed doses.
Assessing the patient’s compliance with lisinopril therapy, including the dosing schedule and any missed doses, is important when taking lisinopril because non-compliance can lead to poor blood pressure control and potentially serious complications, and addressing non-compliance can improve the effectiveness of the medication.
9. Assess the patient for side effects of lisinopril, such as dizziness, dry cough, and headache.
Assessing the patient for side effects of lisinopril, such as dizziness, dry cough, and headache, is important because these side effects can significantly impact the patient’s quality of life and may lead to non-compliance, and early identification of side effects can lead to appropriate interventions and management.
10. Assess the patient’s lifestyle factors, including smoking, diet, and exercise habits, as these can impact the effectiveness of lisinopril therapy.
Assessing the patient’s lifestyle factors, including smoking, diet, and exercise habits, when taking lisinopril is important because lifestyle modifications can significantly impact blood pressure control and reduce the need for medication, and addressing these factors can improve overall cardiovascular health and reduce the risk of complications.
Nursing Diagnosis
List of nursing diagnosis and explanation for patient taking lisinopril:
1. Decreased cardiac output due to the heart’s inability to pump blood effectively. The weakened or damaged heart muscle is unable to generate sufficient force to propel blood forward, leading to decreased blood flow throughout the body.
2. Ineffective therapeutic regimen management related to poor adherence to lisinopril therapy. This nursing diagnosis applies when a patient fails to comply with their lisinopril regimen, leading to poor blood pressure control and potential complications.
3. Risk for injury related to lisinopril-induced hypotension. This nursing diagnosis applies when a patient experiences a drop in blood pressure as a result of lisinopril therapy, which can increase the risk of falls, dizziness, and other injuries.
4. Risk for ineffective renal function related to lisinopril therapy. This nursing diagnosis applies when a patient taking lisinopril is at risk for renal impairment, which can occur due to the medication’s effects on renal function.
5. Anxiety related to potential adverse effects of lisinopril therapy. This nursing diagnosis applies when a patient experiences anxiety or fear related to the potential adverse effects of lisinopril therapy, such as angioedema or hyperkalemia.
6. Non-compliance related to cost or lack of understanding of lisinopril therapy. This nursing diagnosis applies when a patient may not comply with their lisinopril regimen due to financial or educational barriers, which can lead to poor blood pressure control and potential complications.
Lisinopril Nursing Interventions
1. Administer lisinopril as prescribed.
This nursing intervention involves administering the medication according to the prescribed dose and schedule.
2. Correct volume depletion, if possible, before initiation of therapy.
It is important to correct volume depletion, if possible, before initiation of lisinopril therapy because lisinopril can cause further depletion of volume, leading to hypotension and renal impairment. By correcting volume depletion before starting lisinopril, the risk of these adverse effects can be reduced, and the medication’s effectiveness can be improved.
3. Collaborate with the healthcare team.
This nursing intervention involves working collaboratively with the healthcare team to ensure the patient receives appropriate and effective care, including medication adjustments and referrals to other healthcare providers as needed.
Patient Education and Teaching
Patients receiving lisinopril should receive education about the medication, its therapeutic effects, potential adverse effects, and the importance of compliance with the prescribed dosage and frequency of administration.
1. Advise the patient to take medication as directed at the same time each day, even if feeling well.
Tell the patient to take missed doses as soon as possible but not if almost time for the next dose. Do not double doses.
2. Warn the patient not to discontinue ACE inhibitor therapy unless directed by a healthcare professional.
suddenly stopping the medication can cause a rapid increase in blood pressure, which can lead to serious complications such as heart attack or stroke. It is important to follow a healthcare professional’s instructions on how to safely discontinue the medication.
3. Advise the patient to avoid salt substitutes or foods containing high levels of potassium or sodium unless directed by healthcare professional.
Lisinopril can increase potassium levels in the blood, and consuming high-potassium foods or salt substitutes can further increase potassium levels and lead to hyperkalemia. Similarly, consuming high-sodium foods can counteract the medication’s effects and increase blood pressure. Therefore, it is essential to follow a balanced, low-sodium diet as advised by a healthcare professional.
4. Caution patient to change positions slowly to minimize hypotension.
Use of alcohol, standing for long periods, exercising, and hot weather may increase orthostatic hypotension.
5. Instruct the patient to notify the healthcare professional of all medications, vitamins, or herbal products being taken.
Lisinopril may interact with other medications, such as diuretics or potassium supplements, and the medication history can help guide appropriate prescribing and monitoring of the medication.
6. Advise the patient to avoid driving and other activities requiring alertness until response to medication is known.
Lisinopril can cause dizziness, lightheadedness, and fatigue as potential side effects, which can impair the patient’s ability to perform these activities safely. Therefore, patients should be cautious when performing activities that require mental alertness until they know how this medication affects them.
7. Tell the patient to report any side effects.
Patients should report any side effects of lisinopril, such as dizziness, dry cough, or headache, to their healthcare provider promptly.
8. Inform the patient to give information on past and present medical conditions.
Patients should inform their healthcare provider if they have any medical conditions, such as kidney disease or diabetes, as lisinopril may need to be adjusted or monitored more closely in these cases.
9. Advise the patient that medication may cause impairment of taste that generally resolves within 8 – 12 weeks even with continued therapy.
Lisinopril can cause impairment of taste as a potential side effect because it can affect the taste receptors in the mouth, leading to changes in the perception of taste. Additionally, the medication can cause dry mouth, which can also alter the patient’s taste perception.
10. Instruct diabetic patients to monitor blood glucose closely, especially during the first month of therapy.
Lisinopril may cause hypoglycemia.
11. Suggest women of childbearing age use contraception and notify healthcare professional if pregnancy is planned or suspected. If pregnancy is detected, discontinue medication as soon as possible.
Lisinopril may be teratogenic. Patients who are pregnant or planning to become pregnant should not take lisinopril, as it can cause harm to the fetus. They should inform their healthcare provider immediately if they become pregnant while taking lisinopril.
12. Advise the patient to follow a healthy lifestyle.
Patients should follow a healthy lifestyle, including regular exercise, a healthy diet, and avoiding smoking and excessive alcohol intake, to help manage their blood pressure and improve the effectiveness of lisinopril.
13. Emphasize the importance of follow-up examinations.
Regular monitoring is necessary to assess the effectiveness of the medication, adjust the dosage if needed, and detect any potential adverse effects. Additionally, follow-up examinations provide an opportunity for patient education and reinforcement of medication adherence.
14. Encourage the patient to comply with additional interventions for hypertension.
Additional interventions such as weight reduction, low sodium diet, discontinuation of smoking, moderation of alcohol consumption, regular exercise, and stress management are vital in achieving the therapeutic effect of the medication. Medication controls but does not cure hypertension.
15. Instruct the patient and family on the correct technique for monitoring BP. Advise them to check BP at least weekly and to report significant changes to healthcare professional.
It is important to instruct the patient and family on the correct technique for monitoring blood pressure when taking lisinopril because accurate blood pressure readings are crucial to monitor the effectiveness of the medication and adjust the dosage if needed. Additionally, incorrect technique can result in falsely high or low blood pressure readings, leading to inappropriate changes in medication dosage or management. Proper technique ensures that the patient and healthcare provider have an accurate representation of the patient’s blood pressure and can make informed decisions about treatment.
Evaluation and Desired Outcomes
Here are some of the evaluation and desired outcomes for patients taking lisinopril:
1. Reduction in blood pressure. The patient’s blood pressure is within the normal range, reducing the risk of complications such as stroke, heart attack, or kidney disease.
2. Improvement in symptoms of heart failure. The patient experiences decreased shortness of breath, fatigue, and swelling, indicating that lisinopril is effectively managing heart failure.
3. Minimal side effects. The patient reports minimal side effects from lisinopril, such as dizziness or dry cough, indicating that the medication is well-tolerated and improving the patient’s condition.
4. Stable renal function. The patient’s renal function remains stable or improves, indicating that lisinopril is not causing any further damage to the kidneys and may even be protective against kidney disease.
5. Compliance with medication regimen. The patient reports taking lisinopril as prescribed, indicating that they understand the importance of medication adherence and are actively managing their health.
Recommended Resources
Our recommended nursing pharmacology resources and books:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase which will help support us. Thank you! For more information, check out our privacy policy.
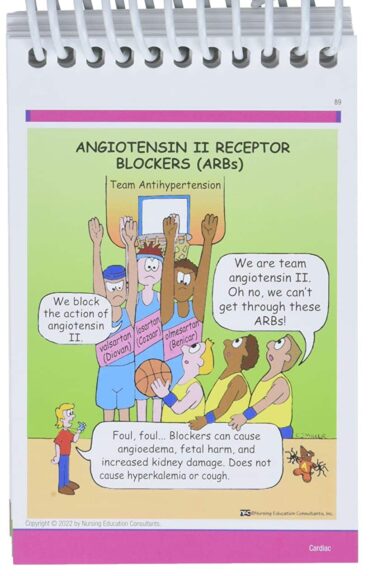
Pharm Phlash! Pharmacology Flash Cards #1 BEST SELLER!
Test-yourself review cards put critical clinical information for nearly 400 of the top generic medications at your fingertips. And, you can count on them for accuracy, because each card is based on content from Davis’s Drug Guide for Nurses. Increase your test scores in pharmacology class.
Focus on Pharmacology (8th Edition)
Focus on Nursing Pharmacology makes challenging concepts more approachable. Engaging learning features cultivate your clinical application, critical thinking and patient education capabilities. This updated 8th edition builds on your knowledge of physiology, chemistry and nursing fundamentals to help you conceptualize need-to-know information about each group of drugs.
Pharmacology Made Incredibly Easy (Incredibly Easy! Series®)
Nursing pharmacology guide offers step-by-step guidance so you can grasp the fundamentals in enjoyable Incredibly Easy style. This is the perfect supplement to class materials, offering solid preparation for NCLEX® as well as a handy refresher for experienced nurses. Colorfully illustrated chapters offer clear, concise descriptions of crucial nursing pharmacology concepts and procedures.
Lehne’s Pharmacology for Nursing Care (11th Edition)
The Eleventh Edition of Lehne’s Pharmacology for Nursing Care provides a thorough understanding of key drugs and their implications for nursing care. This text, written by renowned nursing educators, helps you comprehend and apply pharmacology principles. A clear and engaging writing style simplifies complex concepts, making even the most challenging pharmacology content enjoyable. We recommend this book if you want a comprehensive nursing pharmacology guide.
Nursing Drug Handbook
Nursing2023 Drug Handbook delivers evidence-based, nursing-focused drug monographs for nearly 3700 generic, brand-name, and combination drugs. With a tabbed, alphabetical organization and a “New Drugs” section, NDH2023 makes it easy to check drug facts on the spot.

Pharmacology and the Nursing Process
The 10th edition of Pharmacology and the Nursing Process offers practical, user-friendly pharmacology information. The photo atlas contains over 100 unique illustrations and photographs depicting drug administration techniques. Updated drug content reflects the most recent FDA drug approvals, withdrawals, and therapeutic uses.

Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, and Memory Aids for Nurses
The 6th edition of Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, & Memory Aids for Nurses incorporates illustrations and humor to make studying easier and more enjoyable. This unique pharmacology review can be utilized as a spiral-bound notebook or as individual flashcards, making it ideal for mobile study.
See Also
Here are other nursing pharmacology study guides:
- Nursing Pharmacology – Study Guide for Nurses
Our collection of topics related to nursing pharmacology - Pharmacology Nursing Mnemonics & Tips
These nursing mnemonics aim to simplify the concepts of pharmacology through the use of a simple, concise guide. - Generic Drug Name Stems Cheat Sheet
Learn about these generic drug name stems to help you make sense of drugs easier! - Common Drugs and Their Antidotes
A guide to drug antidotes that nurses should be familiar about. - IV Fluids and Solutions Guide & Cheat Sheet
Get to know the different types of intravenous solutions or IV fluids in this guide and cheat sheet. - Drug Dosage Calculations NCLEX Practice Questions (100+ Items)
Care to take the challenge? This quiz aims to help students and registered nurses alike grasp and master the concepts of medication calculation.
We have a pill for that…
Drug Guides NEW!
Individual drug guides and nursing considerations for the most common medications used in nursing pharmacology:
- Acetaminophen (Tylenol)
- Aspirin
- Atorvastatin (Lipitor)
- Enoxaparin (Lovenox)
- Furosemide (Lasix)
- Gabapentin
- Hydromorphone (Dilaudid)
- Lisinopril
- Metoprolol
- Morphine
Gastrointestinal System Drugs
Respiratory System Drugs
- Antihistamines
- Bronchodilators and Antiasthmatics
- Decongestants
- Expectorants and Mucolytics
- Inhaled Steroids
- Lung Surfactants
Endocrine System Drugs
- Adrenocortical Agents
- Antidiabetic Agents
- Glucose-Elevating Agents
- Hypothalamic Agents
- Insulin
- Parathyroid Agents: Bisphosphonates, Calcitonins
- Pituitary Drugs
- Sulfonylureas
- Thyroid Agents
Autonomic Nervous System Drugs
- Adrenergic Agonists (Sympathomimetics)
- Adrenergic Antagonists (Sympatholytics)
- Anticholinergics (Parasympatholytics)
- Cholinergic Agonists (Parasympathomimetics)
Immune System Drugs
Chemotherapeutic Agents
- Anthelmintics
- Anti-Infective Drugs
- Antibiotics
- Antifungals
- Antineoplastic Agents
- Antiprotozoal Drugs
- Antiviral Drugs
Reproductive System Drugs
Nervous System Drugs
- Antidepressants
- Antiparkinsonism Drugs
- Antiseizure Drugs
- Anxiolytics and Hypnotic Drugs
- General and Local Anesthetics
- Muscle Relaxants
- Narcotics, Narcotic Agonists, and Antimigraine Agents
- Neuromuscular Junction Blocking Agents
- Psychotherapeutic Drugs
Cardiovascular System Drugs
![Lisinopril Nursing Considerations and Patient Teaching [Drug Guide]](https://nurseslabs.com/wp-content/uploads/2023/03/Lisinopril.jpg)


![Furosemide Nursing Considerations and Patient Teaching [Drug Guide]](https://nurseslabs.com/wp-content/uploads/2023/07/Furosemide-480x360.jpg)
![Lisinopril Nursing Considerations and Patient Teaching [Drug Guide]](https://nurseslabs.com/wp-content/uploads/2023/03/Lisinopril-480x360.jpg)





Leave a Comment