Decongestants cause local vasoconstriction, thereby reducing blood flow to the mucous membranes of the nasal passages and sinus cavities. Nasal decongestants (sympathomimetic amines) stimulate the alpha-adrenergic receptors, producing vascular constriction of the capillaries within the nasal mucosa. Decongestants are usually adrenergic or sympathomimetic.
Learn about the uses and nursing care plan considerations needed for patients taking decongestants in this nursing pharmacology study guide.
Decongestants: Generic and Brand Names
Here is a table of commonly encountered decongestants, their generic names, and brand names:
- Topical Nasal Decongestants
- ephedrine (Pretz-D)
- oxymetazoline (Afrin, Allerest)
- phenylephrine (Coricidin)
- tetrahydrazoline (Tyzine)
- xylometazoline (Otrivin)
- Oral Decongestants
- pseudoephedrine (Sudafed, Decofed)
- Topical Steroid Nasal Decongestants
- beclomethasone (Beclovent)
- budesonide (Pulmicort)
- dexamethasone (Decadron)
- flunisolid (Aerobid)
- fluticasone (Flovent)
- triamcinolone (Azmacort)
Disease spotlight: Sinusitis
Sinusitis occurs when the epithelial lining of the sinus cavities becomes inflamed.
- The resultant swelling often causes severe pain due to pressure against the bone, which cannot stretch, leading to blockage of the sinus passage.
- The danger of a sinus infection is that, if it is left untreated, microorganisms can travel up the sinus passages and into brain tissue.
- Symptoms of sinusitis include pain, swelling, and tenderness around the cheek, eyes, or forehead, a blocked nose, reduced sense of smell, a sinus headache, and a high temperature of 38°C.
What are decongestants?
Decongestants decrease the overproduction of secretions by causing local vasoconstriction to the upper respiratory tract.
- This vasoconstriction leads to a shrinking of swollen mucous membranes and tends to open clogged nasal passages, providing relief from the discomfort of a blocked nose and promoting drainage of secretions and improved airflow.
- Topical nasal decongestants, oral decongestant, and topical steroid nasal decongestants are classifications of decongestants.
Therapeutic actions of decongestants
The desired actions of decongestants include the following:
Topical nasal decongestants
- Imitate the effects of the sympathetic nervous system to cause vasoconstriction, leading to decreased edema and inflammation of the nasal membranes.
- Relieve the discomfort of nasal congestion that accompanies the common cold, sinusitis, and allergic rhinitis.
- Dilation of the nares to facilitate medical examination or to relieve the pain and congestion of otitis media.
Oral decongestants
- Decrease nasal congestion related to the common cold, sinusitis, and allergic rhinitis.
- Shrink the nasal mucous membrane by stimulating the alpha-adrenergic receptors in the nasal mucous membranes.
- This shrinkage results in a decrease in membrane size promoting drainage of the sinuses and improving airflow.
Topical nasal steroid decongestants
- The exact mechanism of action of topical steroids is unknown.
- Their anti-inflammatory action results from their ability to produce a direct local effect that blocks many of the complex reactions responsible for the inflammatory response.
Indication
Indications for decongestants include:
Topical nasal decongestants
- Relieves discomfort of nasal congestion associated with the common cold, sinusitis, allergic rhinitis.
- Relieves pressure of otitis media.
Oral decongestants
- Decreases nasal congestion associated with the common cold, allergic rhinitis.
- Relief of pain and congestion of otitis media.
Topical nasal steroid decongestants
- Treatment of seasonal allergic rhinitis in patients who are not obtaining a response with other decongestants or preparations.
- Relieves inflammation following removal of nasal polyps.
Pharmacokinetics
Topical nasal decongestants
- Because these drugs are applied topically, the onset of action is almost immediate and there is less chance of systemic effects.
| Route | Onset | Duration | Half-life (T1/2) | Metabolism | Excretion |
|---|---|---|---|---|---|
| Topical (nasal spray) | Immediate | 4-6h | 0.4 to 0.7 hours | Liver | Urine |
Oral decongestants
Pseudoephedrine is generally well absorbed and reaches peak levels quickly- in 20 to 45 mins.
Topical nasal steroids decongestants
The onset of action is not immediate, and these drugs may actually require up to 1 week to cause any changes.
| Route | Onset | Peak | Duration | Half-life (T1/2) |
|---|---|---|---|---|
| Topical (nasal spray) | Immediate | 10-30min | 4-6h | Not generally absorbed systemically. |
Contraindications and Cautions
The following are contraindications and cautions for the use of decongestants:
- Caution must be used when there is lesion or erosion in the mucous membrane that could lead to systemic absorption.
- Caution should also be used in patients with any condition that might be exacerbated by sympathetic activity.
- If used during pregnancy or lactation, caution is advised.
- Caution should be used in any patient who has an active infection, including tuberculosis because systemic absorption would interfere with the inflammatory and immune response.
Adverse effects
Adverse effects from the use of decongestants include:
- Rebound congestion. An adverse effect that accompanies frequent or prolonged use of the drug is a rebound congestion, technically called rhinitis medicamentosa.
- Topical nasal decongestants. Adverse effects associated with topical decongestants include local stinging and burning, which may occur the first few times the drug is used.
- Oral decongestants. Because this drug is taken systemically, adverse effects related to the sympathomimetic effects are more likely to occur, including feelings of anxiety, tenseness, restlessness, tremors, hypertension, arrhythmia, sweating and pallor.
- Topical nasal steroids decongestants. The most common adverse effects are local burning, stinging, dryness of the mucosa, and headache.
Interactions
Interactions involved in the use of decongestants include the following:
- Cyclopropane or halothane. The use of topical nasal decongestants is contraindicated with concurrent use of cyclopropane or halothane anesthesia because serious cardiovascular effects could occur.
- OTC products. Many OTC products, including cold remedies, allergy medications, and flu remedies may contain pseudoephedrine; taking many of these products concurrently can cause serious adverse effects.
- Acute infections. Because nasal steroids block the inflammatory response, their use is contraindicated in the presence of acute infections such as Candida albicans infection, tuberculosis, and any airborne infections (e.g., chicken pox, measles) because systemic absorption would interfere with the inflammatory and immune responses.
Nursing considerations
The nursing considerations in the administration of decongestants include the following:
Nursing Assessment
History taking and examination of a client using decongestants should include the following:
- Assess for possible cautions and contraindications: any history of allergy to the drug or a component of the drug vehicle; glaucoma; hypertension; diabetes; thyroid disease; coronary disease; and prostate problems; pregnancy and lactation, and acute infections, all of which could be exacerbated by the sympathomimetic effects and which require cautious use of the drug.
- Perform a physical examination to establish baseline data for assessing the effectiveness of the drug and the occurrence of any adverse effects associated with drug therapy.
- Assess skin color and temperature to assess the sympathetic response.
- Evaluate orientation and reflexes to evaluate the central nervous system (CNS) effects of the drug.
- Monitor pulse, blood pressure, and cardiac auscultation to assess cardiovascular and sympathomimetic effects.
- Evaluate respirations and adventitious breath sounds to assess the effectiveness of the drug and the potential excess effect.
- Evaluate nasal mucous membrane to monitor for lesions that could lead to systemic absorption and to evaluate the decongestant effect.
- Monitor urinary output to evaluate for urinary retention.
- Monitor temperature to monitor for the possibility of acute infection.
Nursing Diagnosis and Care Planning
Nursing diagnoses related to the use of the drug include:
- Acute pain related to GI, CNS, or local effects of the drug.
- Disturbed sensory perception (Kinesthetic) related to CNS effects.
- Deficient knowledge regarding drug therapy.
- Increased cardiac output related to sympathomimetic actions of the drug.
- Risk for injury related to the suppression of inflammatory reaction.
Nursing Implementation with Rationale
The nursing interventions for clients using decongestants are:
- Proper administration. Teach the patient the proper administration of the drug to ensure the therapeutic effect.
- Proper technique. The patient should be instructed to clear the nasal passages before use, to tilt the head back when applying the drops or spray, and to keep it tilted back for a few seconds after administration; this techniques helps to ensure contact with the affected mucous membranes and decreases the chances of letting the drops trickle down the back of the throat, which may lead to more systemic effects.
- Duration of intake. Caution the patient not to use the drug for longer than 5 days and to seek medical care if signs and symptoms persist after that time to facilitate detection of underlying medical conditions that may require treatment.
- Avoid overdosage. Caution the patient that these drugs are found in many over-the-counter preparations and that care should be taken not to inadvertently combine drugs with the same ingredients, which could lead to overdose.
- Safety measures. Provide safety measures if dizziness or sedation occurs as a result of drug therapy to prevent patient injury.
- Comfort measures. Institute other measures to help relieve the discomfort of congestion (e.g., use of a humidifier, increased fluid intake, cool environment, avoidance of smoke-filled areas) as appropriate.
- Patient teaching. Provide thorough patient teaching, including the drug name and prescribed dosage, measures to help avoid adverse effects, warning signs that may indicate problems, and the need for periodic monitoring and evaluation, to enhance patient knowledge about drug therapy and to promote compliance.
- Provide support. Offer support and encouragement to help the patient cope with the disease and the drug regimen.
- Ensure compliance. For topical nasal steroid decongestants, encourage the patient to continue using the drug regularly, even if results are not seen immediately, because benefits may take 2 to 3 weeks to appear.
- Monitor for infection. Monitor the patient for the development of acute infection that would require medical intervention; encourage the patient to avoid areas where airborne infections could be a problem because steroid use decreases the effectiveness of the immune and inflammatory responses.
Evaluation
Evaluation of a client using decongestants include:
- Monitor patient response to the drug (relief of nasal congestion).
- Monitor for adverse effects ( local stinging and burning).
- Evaluate the effectiveness of the teaching plan (patient can name drug, dosage, adverse effects to watch for, specific measures to avoid them, and measures to take to increase the effectiveness of the drug.
- Monitor the effectiveness of comfort and safety measures and compliance of the regimen.
Recommended Resources
Our recommended nursing pharmacology resources and books:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase which will help support us. Thank you! For more information, check out our privacy policy.
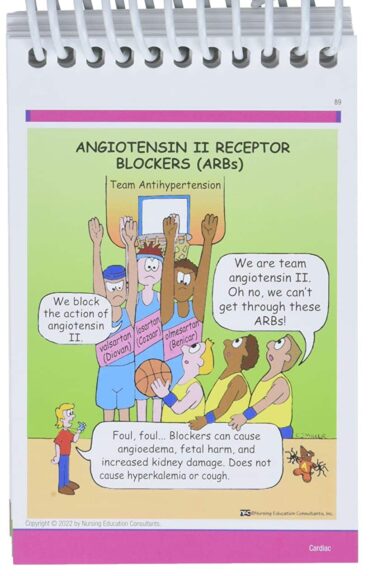
Pharm Phlash! Pharmacology Flash Cards #1 BEST SELLER!
Test-yourself review cards put critical clinical information for nearly 400 of the top generic medications at your fingertips. And, you can count on them for accuracy, because each card is based on content from Davis’s Drug Guide for Nurses. Increase your test scores in pharmacology class.
Focus on Pharmacology (8th Edition)
Focus on Nursing Pharmacology makes challenging concepts more approachable. Engaging learning features cultivate your clinical application, critical thinking and patient education capabilities. This updated 8th edition builds on your knowledge of physiology, chemistry and nursing fundamentals to help you conceptualize need-to-know information about each group of drugs.
Pharmacology Made Incredibly Easy (Incredibly Easy! Series®)
Nursing pharmacology guide offers step-by-step guidance so you can grasp the fundamentals in enjoyable Incredibly Easy style. This is the perfect supplement to class materials, offering solid preparation for NCLEX® as well as a handy refresher for experienced nurses. Colorfully illustrated chapters offer clear, concise descriptions of crucial nursing pharmacology concepts and procedures.
Lehne’s Pharmacology for Nursing Care (11th Edition)
The Eleventh Edition of Lehne’s Pharmacology for Nursing Care provides a thorough understanding of key drugs and their implications for nursing care. This text, written by renowned nursing educators, helps you comprehend and apply pharmacology principles. A clear and engaging writing style simplifies complex concepts, making even the most challenging pharmacology content enjoyable. We recommend this book if you want a comprehensive nursing pharmacology guide.
Nursing Drug Handbook
Nursing2023 Drug Handbook delivers evidence-based, nursing-focused drug monographs for nearly 3700 generic, brand-name, and combination drugs. With a tabbed, alphabetical organization and a “New Drugs” section, NDH2023 makes it easy to check drug facts on the spot.

Pharmacology and the Nursing Process
The 10th edition of Pharmacology and the Nursing Process offers practical, user-friendly pharmacology information. The photo atlas contains over 100 unique illustrations and photographs depicting drug administration techniques. Updated drug content reflects the most recent FDA drug approvals, withdrawals, and therapeutic uses.

Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, and Memory Aids for Nurses
The 6th edition of Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, & Memory Aids for Nurses incorporates illustrations and humor to make studying easier and more enjoyable. This unique pharmacology review can be utilized as a spiral-bound notebook or as individual flashcards, making it ideal for mobile study.
See Also
Here are other nursing pharmacology study guides:
- Nursing Pharmacology – Study Guide for Nurses
Our collection of topics related to nursing pharmacology - Pharmacology Nursing Mnemonics & Tips
These nursing mnemonics aim to simplify the concepts of pharmacology through the use of a simple, concise guide. - Generic Drug Name Stems Cheat Sheet
Learn about these generic drug name stems to help you make sense of drugs easier! - Common Drugs and Their Antidotes
A guide to drug antidotes that nurses should be familiar about. - IV Fluids and Solutions Guide & Cheat Sheet
Get to know the different types of intravenous solutions or IV fluids in this guide and cheat sheet. - Drug Dosage Calculations NCLEX Practice Questions (100+ Items)
Care to take the challenge? This quiz aims to help students and registered nurses alike grasp and master the concepts of medication calculation.
We have a pill for that…
Drug Guides NEW!
Individual drug guides and nursing considerations for the most common medications used in nursing pharmacology:
- Acetaminophen (Tylenol)
- Aspirin
- Atorvastatin (Lipitor)
- Enoxaparin (Lovenox)
- Furosemide (Lasix)
- Gabapentin
- Hydromorphone (Dilaudid)
- Lisinopril
- Metoprolol
- Morphine
Gastrointestinal System Drugs
Respiratory System Drugs
- Antihistamines
- Bronchodilators and Antiasthmatics
- Decongestants
- Expectorants and Mucolytics
- Inhaled Steroids
- Lung Surfactants
Endocrine System Drugs
- Adrenocortical Agents
- Antidiabetic Agents
- Glucose-Elevating Agents
- Hypothalamic Agents
- Insulin
- Parathyroid Agents: Bisphosphonates, Calcitonins
- Pituitary Drugs
- Sulfonylureas
- Thyroid Agents
Autonomic Nervous System Drugs
- Adrenergic Agonists (Sympathomimetics)
- Adrenergic Antagonists (Sympatholytics)
- Anticholinergics (Parasympatholytics)
- Cholinergic Agonists (Parasympathomimetics)
Immune System Drugs
Chemotherapeutic Agents
- Anthelmintics
- Anti-Infective Drugs
- Antibiotics
- Antifungals
- Antineoplastic Agents
- Antiprotozoal Drugs
- Antiviral Drugs
Reproductive System Drugs
Nervous System Drugs
- Antidepressants
- Antiparkinsonism Drugs
- Antiseizure Drugs
- Anxiolytics and Hypnotic Drugs
- General and Local Anesthetics
- Muscle Relaxants
- Narcotics, Narcotic Agonists, and Antimigraine Agents
- Neuromuscular Junction Blocking Agents
- Psychotherapeutic Drugs
Cardiovascular System Drugs
References and Sources
References and sources for this Decongestants Nursing Pharmacology Guide:
- Karch, A. M., & Karch. (2011). Focus on nursing pharmacology. Wolters Kluwer Health/Lippincott Williams & Wilkins. [Link]
- Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
- Lehne, R. A., Moore, L. A., Crosby, L. J., & Hamilton, D. B. (2004). Pharmacology for nursing care.
- Smeltzer, S. C., & Bare, B. G. (1992). Brunner & Suddarth’s textbook of medical-surgical nursing. Philadelphia: JB Lippincott.











Leave a Comment