Hydromorphone (Dilaudid) is considered a powerful opioid pain medication that is used to treat moderate to severe pain. As nurses, awareness and understanding of the potential risks and considerations when administering Dilaudid to patients is necessary since this drug can be habit-forming and should only be used under the close supervision of a healthcare provider.
What is Hydromorphone (Dilaudid)?
Hydromorphone (Dilaudid) is a powerful opioid pain medication. It is used to treat moderate to severe pain and is typically taken orally in tablet or liquid form. It works by binding to specific receptors in the brain and spinal cord, which reduces the perception of pain. Common side effects include drowsiness, nausea, and constipation. It can also cause respiratory depression and should not be used in individuals with asthma or chronic obstructive pulmonary disease (COPD). Long-term use can lead to tolerance, physical dependence, and addiction. Due to the potential for addiction and overdose, Dilaudid is a controlled substance and is only available by prescription from a healthcare provider. It should be used with caution and under close medical supervision.
Generic Name
- hydromorphone
- dihydromorphinone
Brand Names
Dilaudid is a brand name for the drug hydromorphone, a powerful opioid pain medication. It is also available in different formulations and brand names like:
- Dilaudid-HP (high potency)
- Dilaudid-5 (oral solution)
- Dilaudid-8 (oral solution)
- Hydromorphone Hydrochloride (generic name)
- Exalgo (extended-release tablet)
- Hydromorph Contin (extended-release tablet)
- Palladone (extended-release capsule)
- Jurnista
Please note that these are some of the brand names, there may be other brand names available in different countries or regions.
Drug Classification of Dilaudid
The drug classification of Dilaudid is as follows:
Therapeutic Class
- allergy, cold, and cough remedies (antitussives), opioid analgesics
Pharmacologic Class
- opioid agonists
Indications and Therapeutic Effects
Dilaudid, also known by its generic name hydromorphone, is a powerful opioid pain medication that is indicated for the relief of moderate to severe pain. Some of the common indications for Dilaudid include:
- Acute pain. Dilaudid can be used to manage pain associated with surgery, injury, or other medical conditions.
- Chronic pain. Dilaudid can be used to manage pain associated with conditions such as cancer, arthritis, or neuropathic pain.
- Pain management in palliative care. Dilaudid can be used to manage pain in patients with advanced illnesses or terminal conditions.
- Pain management in opioid-tolerant patients. Dilaudid can be used in patients who have developed tolerance to other opioid pain medications.
- Antitussive. Dilaudid is also used, in low doses, as an antitussive.
Mechanism of Action
Dilaudid (hydromorphone) is a powerful opioid pain medication that works by binding to specific receptors in the brain and spinal cord known as mu, delta, and kappa opioid receptors. When it binds to these receptors, it reduces the perception of pain and can also produce feelings of pleasure and euphoria.
The binding of Dilaudid to the mu-opioid receptors in the central nervous system (CNS) leads to an increase in the release of neurotransmitters such as dopamine and serotonin. This increase in neurotransmitters can result in the inhibition of pain perception, decreased anxiety, and increased feelings of euphoria.
Dilaudid also causes a decrease in the activity of the sympathetic nervous system which can result in decreased heart rate, blood pressure, and respiratory rate.
Additionally, Dilaudid can also cause a decrease in the activity of the gastrointestinal tract, resulting in constipation, which is a common side effect of opioid use.
Overall, Dilaudid’s mechanism of action is related to its ability to bind to opioid receptors in the brain and spinal cord, resulting in a reduction in pain perception and an increase in feelings of pleasure and euphoria.
Precautions and Contraindications
Some precautions and contraindications to consider before using Dilaudid include:
- Respiratory depression. Dilaudid can cause respiratory depression, which can be life-threatening. Patients with chronic obstructive pulmonary disease (COPD), sleep apnea, or other respiratory conditions should use Dilaudid with caution.
- Head injury or increased intracranial pressure. Dilaudid should be used with caution in patients with a head injury or increased intracranial pressure, as it can increase the risk of respiratory depression.
- Hypotension. Dilaudid can cause hypotension (low blood pressure), which can be problematic for patients with cardiovascular disease or other conditions that affect blood pressure.
- Gastrointestinal obstruction. Dilaudid should be used with caution in patients with gastrointestinal obstruction, as it can cause constipation and other gastrointestinal side effects.
- Hepatic or Renal Disease. Dilaudid is metabolized in the liver largely to hydromorphone-3-glucuronide. This metabolite accumulates in patients with kidney disease and can cause opioid neurotoxicity.
- Hypothyroidism. Dilaudid and other central nervous system depressants, sedatives, or narcotic analgesics must be avoided in patients with severe hypothyroidism because significant respiratory depression may occur.
- Addiction, abuse, and misuse. Dilaudid is a controlled substance and has a potential for addiction, abuse, and misuse. It should be used only as directed by a healthcare provider and should be kept in a secure location.
- Pregnancy and breastfeeding. Dilaudid should be used with caution during pregnancy and breastfeeding, as it can cross the placenta and may be present in breast milk.
- Drug interactions. Dilaudid can interact with other medications, such as sedatives, antidepressants, and antihistamines, which can increase the risk of respiratory depression and other side effects.
- Elderly. Dilaudid should be used with caution in elderly patients, as they may be more sensitive to the medication’s effects.
- Children. Dilaudid is not recommended for use in children under the age of 6 years.
Drug Interactions
When administering Dilaudid, the nurse should consider the following drug interactions:
Drug-Drug
Some potential drug interactions with Dilaudid include:
- Benzodiazepines. Taking Dilaudid with other central nervous system depressants, such as benzodiazepines or alcohol, can increase the risk of sedation, respiratory depression, and other CNS side effects.
- Opioids, non-benzodiazepines. Dilaudid can also interact with other opioids and potentially lead to an overdose.
- Antidepressants and antipsychotics. Dilaudid can interact with certain antidepressants and antipsychotics, which can lead to increased sedation and respiratory depression.
- Hypnotics, anxiolytics, general anesthetics, and muscle relaxants. These may cause profound sedation, respiratory depression, coma, and death
- Antibiotics and antifungals. Dilaudid can also interact with certain antibiotics and antifungals, which can lead to decreased effectiveness.
- Partial antagonists. Buprenorphine, butorphanol, nalbuphine, or pentazocine may precipitate opioid withdrawal in physically dependent patients.
- Nalbuphine or pentazocine. Nalbuphine or pentazocine may decrease analgesia.
- Drugs that affect serotonergic neurotransmitter systems. Tricyclic antidepressants, SSRIs, SNRIs, MAO inhibitors, TCAs, tramadol, trazodone, mirtazapine, 5 – HT3 receptor antagonists, linezolid, methylene blue, and triptans increase the risk of serotonin syndrome.
Drug-Natural Products
- Kava-kava, valerian, chamomile, or hops. Concomitant use of kava-kava, valerian, chamomile, or hops can increase CNS depression.
Adverse Effects
Some common side effects of Dilaudid that the nurse should consider include:
- Nausea and vomiting. Opioids like Dilaudid can slow the movement of food through the gastrointestinal tract, which can also contribute to nausea and vomiting.
- Constipation. Dilaudid slows down the movement of the muscles in the gastrointestinal tract, which can lead to constipation. Additionally, opioids can also decrease the secretion of fluid in the intestines, which can also contribute to constipation.
- Drowsiness and dizziness. The active ingredient hydromorphone is a central nervous system (CNS) depressant, which can cause drowsiness and sedation as well as dizziness. Drowsiness and dizziness can impair the individual’s ability to perform tasks such as driving or operating heavy machinery and make a person more prone to falls, so it is important to use caution when performing these activities while taking Dilaudid.
- Dry mouth. Dry mouth, also known as xerostomia, occurs when there is not enough saliva to keep the mouth moist. Opioids like Dilaudid may decrease the production of saliva by the salivary glands.
- Headache. It is thought that this may be related to changes in the levels of certain chemicals in the brain, such as serotonin, that can cause changes in blood vessels in the brain and lead to headaches.
- Sweating. Sweating caused by Dilaudid is usually not severe, but it is thought that it may be related to changes in the levels of certain chemicals in the body, such as histamine, that can cause changes in the sweat glands.
- Itching. Itching caused by Dilaudid can be mild or severe and can be accompanied by skin rash, hives, or other skin symptoms. This may be related to changes in the levels of certain chemicals in the body, such as histamine, that can cause itching sensations in the skin.
- Loss of appetite. This may be related to changes in the levels of certain chemicals in the brain, such as dopamine, that regulate appetite and feelings of hunger.
- Fatigue. This may be related to changes in the levels of certain chemicals in the brain, such as dopamine, that regulate sleep and wakefulness. Fatigue caused by Dilaudid can range from mild to severe and can be accompanied by drowsiness or difficulty staying awake.
- Weakness. This may be related to changes in the levels of certain chemicals in the brain and body that regulate muscle tone and strength. Weakness caused by Dilaudid can range from mild to severe and can affect different muscle groups in the body.
More serious side effects of Dilaudid can include:
- Respiratory depression. Respiratory depression is a major concern with all opioid medications, including Dilaudid. Opioids like Dilaudid work by binding to specific receptors in the brain and spinal cord that control breathing. When these receptors are activated by the drug, they can slow down breathing and decrease the amount of oxygen that reaches the body’s tissues.
- Confusion. This may be related to changes in the levels of certain chemicals in the brain, such as dopamine and serotonin, that regulate cognitive function, including memory and attention.
- Addiction or dependence. Although opioids like Dilaudid are excellent painkillers, when used recreationally, the euphoric high and sense of relaxation they bring can prove to be addictive. Recreational Dilaudid use can be harmful, causing devastation in many areas of a person’s life, and it can even be fatal.
- Low blood pressure. Dilaudid, like all opioids, can cause a decrease in blood pressure by decreasing the activity of the sympathetic nervous system, which helps to regulate blood pressure. This can result in a drop in blood pressure, especially when standing up (orthostatic hypotension), which can cause symptoms such as dizziness or fainting. Patients who have pre-existing low blood pressure, or who are taking medications that lower blood pressure, may be at an increased risk for experiencing hypotension with Dilaudid. Elderly patients are also at higher risk for hypotension and other side effects of Dilaudid.
- Slow heart rate. Dilaudid can cause a decrease in the activity of the sympathetic nervous system, which helps to regulate the heart rate. This can result in a slowing of the heart rate, especially when used in higher doses or in combination with other medications that can slow the heart rate. Patients who have pre-existing slow heart rates, or who are taking medications that slow the heart rate, may be at an increased risk for experiencing bradycardia with Dilaudid. Elderly patients and patients with pre-existing medical conditions, such as heart disease, may also be at higher risk for bradycardia and other side effects of Dilaudid.
- Seizures. Dilaudid can cause seizures as a side effect, especially at high doses or in individuals with a history of seizures or susceptibility to them.
- Blurred vision. This may be related to its effects on the central nervous system, including changes in the regulation of the pupils and alterations in the perception of visual information.
- Fainting. Dilaudid can cause fainting due to its effects on the central nervous system and cardiovascular system. Dilaudid can cause a decrease in blood pressure and heart rate, which can lead to dizziness and fainting, particularly in older adults or those with pre-existing medical conditions that affect blood pressure regulation. Additionally, Dilaudid may cause changes in the regulation of blood flow, leading to decreased oxygen and nutrient delivery to the brain, resulting in fainting.
Administration Considerations
Available Forms
Dilaudid is available in the following forms:
- Immediate-release tablets: 2 mg, 4 mg, 8 mg.
- Extended-release tablets (abuse-deterrent): 4 mg, 8 mg, 12 mg, 16 mg, 32 mg.
- Controlled-release capsules: 3 mg, 4.5 mg, 6 mg, 9 mg, 12 mg, 18 mg, 24 mg, 30 mg.
- Oral solution: 1 mg/mL.
- Injection: 1 mg/mL, 2 mg/mL, 4 mg/mL, 10 mg/mL.
- Suppositories: 3 mg.
Dosage for Children
Analgesic
- PO (Children <50 kg): 0.06 mg/kg every 3 – 4 hr initially, younger children may require smaller initial doses of 0.03 mg/kg. Maximum dose 5 mg.
- IV, IM, Subcut (Children <50 kg): 0.015 mg/kg mg every 3 – 4 hr as needed initially; may be increased.
Antitussive
- PO (Children >12 yr): 1 mg every 3 – 4 hr.
- PO (Children 6–12 yr): 0.5 mg every 3–4 hr.
Dosage for Adults
Analgesic
- PO (Adults ≥50 kg): Immediate-release — 4 – 8 mg every 3 – 4 hr initially (some patients may respond to doses as small as 2 mg initially); or once 24-hr opioid requirement is determined, convert to extended-release by administering total daily oral dose once daily.
- PO (Adults <50 kg): 0.06 mg/kg every 3 – 4 hr initially, younger children may require smaller initial doses of 0.03 mg/kg. Maximum dose 5 mg.
- IV, IM, Subcut (Adults ≥50 kg): 1.5 mg every 3 – 4 hr as needed initially; may be increased.
- IV, IM, Subcut (Adults <50 kg): 0.015 mg/kg mg every 3 – 4 hr as needed initially; may be increased.
- IV (Adults): Continuous infusion (unlabeled)— 0.2 – 3 mg/hr depending on previous opioid use. An initial bolus of twice the hourly rate in mg may be given with subsequent breakthrough boluses of 50 – 100% of the hourly rate in mg.
- Rect (Adults): 3 mg every 6 – 8 hr initially as needed.
- For Hepatic Impairment
- PO (Adults): Moderate hepatic impairment (extended–release)—decrease initial dose by 75%.
- For Renal Impairment
Antitussive
- PO (Adults): 1 mg every 3 – 4 hr.
Pharmacokinetics
Dilaudid (hydromorphone) has a rapid onset of action and a relatively short half-life, with a peak effect typically occurring within 30 minutes to 2 hours after administration, depending on the route of administration.
- Absorption. Dilaudid is rapidly absorbed after oral administration and has a bioavailability of approximately 100%.
- Distribution. The drug is widely distributed throughout the body and is highly protein-bound.
- Metabolism and Excretion. Dilaudid is metabolized in the liver by the cytochrome P450 enzyme system, with the primary metabolites being hydromorphone-3-glucuronide and hydromorphone-6-glucuronide. These metabolites are then excreted in the urine.
- Half-life. The elimination half-life of Dilaudid oral (immediate-release) or injection is typically 2-4 hours but may be prolonged in individuals with liver or kidney impairment. Oral (extended-release) — 8 – 15 hr.
Nursing Considerations for Dilaudid
The following are Dilaudid nursing considerations and nursing implications:
Nursing Assessment
There are several important aspects of a nursing assessment for a patient taking Dilaudid, including:
1. Assess BP, pulse, and respirations before and periodically during administration.
If the respiratory rate is <10/min, assess the level of sedation. The dose may need to be decreased by 25 – 50%. Initial drowsiness will diminish with continued use.
2. Assess the type, location, and intensity of pain.
Assess the patient’s pain level and pain type prior to and 1 hour following IM or PO and 5 min (peak) following IV administration of Dilaudid to determine its effectiveness. When titrating opioid doses, increases of 25 – 50% should be administered until there is either a 50% reduction in the patient’s pain rating on a numerical or visual analogue scale or the patient reports satisfactory pain relief. When titrating doses of short-acting hydromorphone, a repeat dose can be safely administered at the time of the peak if the previous dose is ineffective and side effects are minimal.
3. Patients on a continuous infusion should have additional bolus doses provided every 15 – 30 minutes, as needed, for breakthrough pain.
The bolus dose is usually set to the amount of drug-infused each hour by continuous infusion.
4. Assess geriatric and pediatric patients frequently.
Children and the older people are more sensitive to the effects of opioid analgesics and may experience side effects and respiratory complications more frequently.
5. Patients taking extended-release hydromorphone may require additional short-acting or rapid-onset opioid doses for breakthrough pain.
Doses of short-acting opioids should be equivalent to 10 – 20% of 24 hours total and given every 2 hours as needed.
6. Monitor for adverse effects.
Dilaudid can cause respiratory depression, sedation, and changes in blood pressure, heart rate, and mental status. Monitor these parameters regularly and report any concerning changes to the healthcare provider.
7. Assess bowel function routinely.
Establish prevention of constipation with increased intake of fluids and bulk, and laxatives to minimize constipating effects.
8. The dosage of opioid analgesics like hydromorphone should be individualized for any given patient.
Dilaudid is a potent opioid and should be used with caution in individuals with a history of substance abuse, respiratory depression, or other medical conditions. The dose should be individualized based on the patient’s pain level, tolerance to opioids, and other factors.
9. Review the patient’s medication list prior to administering Dilaudid for drug interactions.
Dilaudid can interact with other medications, including benzodiazepines, alcohol, and anti-anxiety drugs, potentially causing increased sedation or respiratory depression.
10. Prolonged use of hydromorphone may lead to physical and psychological dependence and tolerance.
This should not prevent the patient from receiving adequate analgesia. Most patients who receive hydromorphone for pain do not develop psychological dependence. Progressively higher doses may be required to relieve pain with long-term therapy.
12. Assess the risk for opioid addiction, abuse, or misuse prior to administration.
Abuse or misuse of extended-release preparations by crushing, chewing, snorting, or injecting the dissolved product will result in uncontrolled delivery of hydromorphone and can result in overdose and death. Exalgo is an abuse-deterrent formulation that is difficult to crush and, if crushed, results in a gel.
13. Monitor withdrawal symptoms.
Withdrawal symptoms may occur if Dilaudid is abruptly discontinued. Gradual tapering of the dose may be required to prevent withdrawal symptoms.
14. Reassess pain.
Dilaudid is a potent opioid and may not be appropriate for all types of pain. In some cases, non-opioid pain management strategies, such as physical therapy or nerve blocks, may be more appropriate.
15. Assess cough and lung sounds during antitussive use.
Hydromorphone depresses the cough reflex by direct effect on the cough center in the medulla. Hydromorphone depresses the respiratory reflex with a direct effect on brain stem respiratory centers.
16. Naloxone (Narcan) is the antidote if an opioid antagonist is required to reverse respiratory depression or coma.
Dilute the 0.4-mg ampule of naloxone in 10 mL of 0.9% NaCl and ad- minister 0.5 mL (0.02 mg) by IV push every 2 min. For children and patients weighing <40 kg, dilute 0.1 mg of naloxone in 10 mL of 0.9% NaCl for a concentration of 10 mcg/mL and administer 0.5 mcg every 2 min. Titrate dose to avoid withdrawal, seizures, and severe pain.
Nursing Diagnosis
The nursing diagnosis for Dilaudid (hydromorphone) use may include:
- Acute pain (Indications)
- Chronic pain (Indications)
- Ineffective breathing pattern (Side effects)
- Risk for injury (Side effects)
- Risk for constipation (Side effects)
- Deficient knowledge
Dilaudid Nursing Interventions
Nurses play an important role in the management of a patient’s pain by administering prescribed pain-relieving interventions, assessing the effectiveness of those interventions, monitoring for adverse reactions, and serving as an advocate for the patient when the prescribed intervention is ineffective. Here are several nursing interventions that can be implemented to ensure the safe and effective use of the medication:
1. Verify the patient’s identity and the medication order before administering the drug.
The nurse must confirm the patient’s identification matches the medication administration record (MAR) and medication label prior to administration to ensure that the medication is being given to the correct patient.
2. Calculate doses carefully.
Accidental overdose of opioid analgesics has resulted in fatalities. Before administering, check infusion pump settings. Medication errors with opioid analgesics are common in pediatric patients.
3. Do not confuse it with morphine or oxymorphone; fatalities have occurred. Do not confuse high-potency (HP) dose forms with regular dose forms.
Hydromorphone and morphine are not the same drugs. Hydromorphone and morphine are deemed high-risk or high-alert medications. Oxymorphone is a semisynthetic μ opioid agonist 1.2 times as potent as morphine. An Independent Double Check (IDC) must be done to avoid errors when administering all high-risk drugs.
4. Explain the therapeutic value of medication prior to administration.
This is to enhance the analgesic effect.
5. Observe the patient for any adverse reactions, such as respiratory depression, drowsiness, or confusion.
Respiratory depression is a major concern with all opioid medications, including Dilaudid. Opioids like Dilaudid work by binding to specific receptors in the brain and spinal cord that control breathing.
6. Regularly administered doses may be more effective than prn administration.
Analgesic is more effective if given before pain becomes severe.
7. Document the administration of the medication, including the time, dosage, and any observations or patient responses.
After administering medication, it is important to immediately document the administration to avoid potential errors from an unintended repeat dose.
8. Coadministration with nonopioid analgesics may have additive analgesic effects and permit lower opioid doses.
Combining opioids with other medications or nonmedication treatments, while under the care of a healthcare provider, can improve pain management and result in needing a lower dosage of opioids.
9. Medication should be discontinued gradually after long-term use.
This is to prevent withdrawal symptoms. Withdrawal occurs when an individual’s system adjusts itself to account for the presence of the drug in its tissues. When the levels of the drug drop sharply because the individual has stopped taking the drug or significantly lowered the amount taken, the person develops a number of adverse reactions.
10. Calculate appropriate dose conversions.
- 10.1. When converting from immediate-release to extended-release hydromorphone. Administer total daily oral hydromorphone dose once daily; dose of extended-release product can be titrated every 3 – 4 days.
- 10.2. To convert from another opioid to extended-release hydromorphone. Convert to total daily dose of hydromorphone and then administer 50% of this dose as extended-release hydromorphone once daily; can then titrate dose every 3 – 4 days.
- 10.3. When converting from transdermal fentanyl. Initiate extended-release hydromorphone 18 hours after removing the transdermal fentanyl patch; for each 25 mcg/hr fentanyl transdermal dose, the equianalgesic dose of extended-release hydromorphone is 12 mg once daily (should initiate at 50% of this calculated total daily dose given once daily).
11. Administer Dilaudid with food or milk.
This is to minimize GI irritation.
12. Tell the patient to swallow extended-release tablets whole; not to break, crush, dissolve, or chew.
Misuse of extended-release preparations by crushing, chewing, snorting, or injecting the dissolved product will result in uncontrolled delivery of hydromorphone and can result in overdose and death.
IV Administration of Dilaudid Nursing Considerations
1. IV Push
- Dilute with at least 5mL of sterile water or 0.9% NaCl for injection.
- Inspect solution for particulate matter.
- Slight yellow color does not alter potency.
- Store at room temperature.
- Administer slowly, at a rate not to exceed 2 mg over 3 – 5 min.
- Rapid administration may lead to increased respiratory depression, hypotension, and circulatory collapse.
2. Y-Site Compatibility
- acetaminophen, acyclovir, alemtuzumab, allopurinol, amifostine, amikacin, aminocaproic acid, aminophylline, amiodarone, amphotericin B colloidal, amphotericin B lipid complex, amphotericin B liposome, ampicillin/sulbactam, anidulafungin, argatroban, atracurium, atropine, azithromycin, aztreonam, bivalirudin, bleomycin, bumetanide, busulfan, calcium chloride, calcium gluconate, cangrelor, carboplatin, carmustine, caspofungin, cefepime, cefotaxime, cefoxitin, ceftaroline, ceftazidime, ceftriaxone, cefuroxime, chloramphenicol, chlorpromazine, ciprofloxacin, cisatracurium, cisplatin, cladribine, clindamycin, cyclophosphamide, cyclosporine, cytarabine, dacarbazine, dactinomycin, daptomycin, daunorubicin hydrochloride, dexamethasone, dexmedetomidine, dexrazoxane, digoxin, diltiazem, diphenhydramine, dobutamine, docetaxel, dolasetron, dopamine, doxorubicin, doxorubicin liposome, doxycycline, droperidol, enalaprilat, ephedrine, epinephrine, epirubicin, eptifibatide, ertapenem, erythromycin, esmolol, etoposide, etoposide phosphate, famotidine, fenoldopam, fentanyl, filgrastim, fluconazole, fludarabine, fluorouracil, foscarnet, fosphenytoin, furosemide, ganciclovir, gemcitabine, gentamicin, glycopyrrolate, granisetron, haloperidol, heparin, hetastarch, hydralazine, hydrocortisone, idarubicin, ifosfamide, imipenem/cilastatin, insulin, irinotecan, isoproterenol, ketorolac, labetalol, leucovorin, levofloxacin, lidocaine, linezolid, lorazepam, magnesium sulfate, mannitol, mechlorethamine, melphalan, meropenem, mesna, methotrexate, methyldopate, methylprednisolone, metoclopramide, metoprolol, metronidazole, micafungin, midazolam, milrinone, mitoxantrone, mitomycin, morphine, mycophenolate, nafcillin, naloxone, nesiritide, nicardipine, nitroglycerin, nitroprusside, norepinephrine, octreotide, ondansetron, oxacillin, oxaliplatin, oxytocin, paclitaxel, palonosetron, pamidronate, pancuronium, pemetrexed, penicillin G potassium, pentamidine, pentobarbital, phenylephrine, piperacillin/tazobactam, posaconazole, potassium acetate, potassium chloride, potassium phosphates, procainamide, prochlorperazine, promethazine, propofol, propranolol, quinupristin/dalfopristin, ranitidine, remifentanil, rituximab, rocuronium, scopolamine, sodium acetate, sodium phosphates, streptozocin, succinylcholine, tacrolimus, teniposide, theophylline, thiotepa, tigecycline, tirofiban, tobramycin, topotecan, trastuzumab, trimethoprim/sulfamethoxazole, vancomycin, vasopressin, vecuronium, verapamil, vinblastine, vincristine, vinorelbine, zidovudine, zoledronic acid.
3. Y-Site Incompatibility
- dantrolene, dimenhydrinate, minocycline, phenytoin, sargramostim, thiopental.
Patient Education and Teaching
When providing patients with education about Dilaudid, it’s important to follow these guidelines:
- Advise patient to take only as prescribed and not to change the dose without consulting a healthcare professional.
- Advise patient that hydromorphone is a drug with known abuse potential. Guard it against theft, and never give it to anyone other than the individual for whom it was prescribed.
- Advise patient not to crush, break, or chew the tablet, as this can cause a rapid release and increased risk of side effects
- Advise patient to call for assistance when ambulating or smoking.
- Advise patient to avoid alcohol and other central nervous system depressants while taking Dilaudid.
- Advise patient to change positions slowly to minimize orthostatic hypotension.
- Instruct patient and family members to store in a secure place, out of reach of children and pets.
- Educate patient to dispose of unused medication properly, according to the pharmacist’s instructions.
- Inform healthcare providers about all medications and supplements taken.
- Report any side effects to a physician immediately.
- Advise patient to avoid driving or operating heavy machinery until the effects of the medication are known.
- Advise patient not to stop taking Dilaudid abruptly, as this can cause withdrawal symptoms.
- Instruct patient to notify healthcare professional of all Rx or OTC medications, vitamins, or herbal products being taken and consult a healthcare professional before taking any new medications.
- Encourage patient to turn, cough, and breathe deeply every 2 hr to prevent atelectasis.
- Advise patient to notify a healthcare professional if pregnancy is planned or suspected, or if breastfeeding.
- Educate patient and family members on how and when to administer hydromorphone, discuss safe storage of medication, and how to care for infusion equipment properly.
- For children, teach parents or caregivers how to accurately measure liquid medication and to use only measuring devices dispensed with medication.
- Stress the importance of aggressive prevention of constipation with the use of hydromorphone.
Evaluation and Desired Outcomes
- Pain relief. Dilaudid is an opioid pain medication that is commonly used to treat moderate to severe pain. Its desired outcome is to effectively relieve pain.
- Analgesia (lack of pain sensation). Dilaudid works by binding to specific receptors in the brain and nervous system to reduce the perception of pain. The desired outcome is to produce a state of analgesia.
- Reduced anxiety. Dilaudid can also have a calming effect and may be used to relieve anxiety, particularly in patients with chronic pain. The desired outcome is to reduce anxiety and improve relaxation.
- Relaxation. In addition to its pain-relieving effects, Dilaudid can also produce feelings of relaxation and tranquility. The desired outcome is to promote relaxation and reduce muscle tension.
- Suppression of cough. Dilaudid depresses the cough reflex by direct effect on the cough center in the medulla. Dilaudid depresses the respiratory reflex with a direct effect on brain stem respiratory centers.
Recommended Resources
Our recommended nursing pharmacology resources and books:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase which will help support us. Thank you! For more information, check out our privacy policy.
Pharm Phlash! Pharmacology Flash Cards #1 BEST SELLER!
Test-yourself review cards put critical clinical information for nearly 400 of the top generic medications at your fingertips. And, you can count on them for accuracy, because each card is based on content from Davis’s Drug Guide for Nurses. Increase your test scores in pharmacology class.
Focus on Pharmacology (8th Edition)
Focus on Nursing Pharmacology makes challenging concepts more approachable. Engaging learning features cultivate your clinical application, critical thinking and patient education capabilities. This updated 8th edition builds on your knowledge of physiology, chemistry and nursing fundamentals to help you conceptualize need-to-know information about each group of drugs.
Pharmacology Made Incredibly Easy (Incredibly Easy! Series®)
Nursing pharmacology guide offers step-by-step guidance so you can grasp the fundamentals in enjoyable Incredibly Easy style. This is the perfect supplement to class materials, offering solid preparation for NCLEX® as well as a handy refresher for experienced nurses. Colorfully illustrated chapters offer clear, concise descriptions of crucial nursing pharmacology concepts and procedures.
Lehne’s Pharmacology for Nursing Care (11th Edition)
The Eleventh Edition of Lehne’s Pharmacology for Nursing Care provides a thorough understanding of key drugs and their implications for nursing care. This text, written by renowned nursing educators, helps you comprehend and apply pharmacology principles. A clear and engaging writing style simplifies complex concepts, making even the most challenging pharmacology content enjoyable. We recommend this book if you want a comprehensive nursing pharmacology guide.
Nursing Drug Handbook
Nursing2023 Drug Handbook delivers evidence-based, nursing-focused drug monographs for nearly 3700 generic, brand-name, and combination drugs. With a tabbed, alphabetical organization and a “New Drugs” section, NDH2023 makes it easy to check drug facts on the spot.

Pharmacology and the Nursing Process
The 10th edition of Pharmacology and the Nursing Process offers practical, user-friendly pharmacology information. The photo atlas contains over 100 unique illustrations and photographs depicting drug administration techniques. Updated drug content reflects the most recent FDA drug approvals, withdrawals, and therapeutic uses.

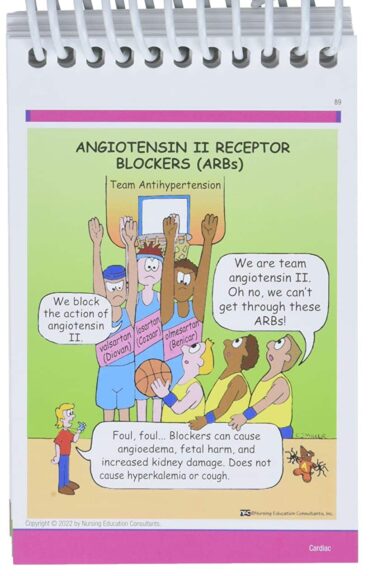
Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, and Memory Aids for Nurses
The 6th edition of Mosby’s Pharmacology Memory NoteCards: Visual, Mnemonic, & Memory Aids for Nurses incorporates illustrations and humor to make studying easier and more enjoyable. This unique pharmacology review can be utilized as a spiral-bound notebook or as individual flashcards, making it ideal for mobile study.
See Also
Here are other nursing pharmacology study guides:
- Nursing Pharmacology – Study Guide for Nurses
Our collection of topics related to nursing pharmacology - Pharmacology Nursing Mnemonics & Tips
These nursing mnemonics aim to simplify the concepts of pharmacology through the use of a simple, concise guide. - Generic Drug Name Stems Cheat Sheet
Learn about these generic drug name stems to help you make sense of drugs easier! - Common Drugs and Their Antidotes
A guide to drug antidotes that nurses should be familiar about. - IV Fluids and Solutions Guide & Cheat Sheet
Get to know the different types of intravenous solutions or IV fluids in this guide and cheat sheet. - Drug Dosage Calculations NCLEX Practice Questions (100+ Items)
Care to take the challenge? This quiz aims to help students and registered nurses alike grasp and master the concepts of medication calculation.
We have a pill for that…
Drug Guides NEW!
Individual drug guides and nursing considerations for the most common medications used in nursing pharmacology:
- Acetaminophen (Tylenol)
- Aspirin
- Atorvastatin (Lipitor)
- Enoxaparin (Lovenox)
- Furosemide (Lasix)
- Gabapentin
- Hydromorphone (Dilaudid)
- Lisinopril
- Metoprolol
- Morphine
Gastrointestinal System Drugs
Respiratory System Drugs
- Antihistamines
- Bronchodilators and Antiasthmatics
- Decongestants
- Expectorants and Mucolytics
- Inhaled Steroids
- Lung Surfactants
Endocrine System Drugs
- Adrenocortical Agents
- Antidiabetic Agents
- Glucose-Elevating Agents
- Hypothalamic Agents
- Insulin
- Parathyroid Agents: Bisphosphonates, Calcitonins
- Pituitary Drugs
- Sulfonylureas
- Thyroid Agents
Autonomic Nervous System Drugs
- Adrenergic Agonists (Sympathomimetics)
- Adrenergic Antagonists (Sympatholytics)
- Anticholinergics (Parasympatholytics)
- Cholinergic Agonists (Parasympathomimetics)
Immune System Drugs
Chemotherapeutic Agents
- Anthelmintics
- Anti-Infective Drugs
- Antibiotics
- Antifungals
- Antineoplastic Agents
- Antiprotozoal Drugs
- Antiviral Drugs
Reproductive System Drugs
Nervous System Drugs
- Antidepressants
- Antiparkinsonism Drugs
- Antiseizure Drugs
- Anxiolytics and Hypnotic Drugs
- General and Local Anesthetics
- Muscle Relaxants
- Narcotics, Narcotic Agonists, and Antimigraine Agents
- Neuromuscular Junction Blocking Agents
- Psychotherapeutic Drugs
Cardiovascular System Drugs
![Furosemide Nursing Considerations and Patient Teaching [Drug Guide]](https://nurseslabs.com/wp-content/uploads/2023/07/Furosemide-480x360.jpg)
![Lisinopril Nursing Considerations and Patient Teaching [Drug Guide]](https://nurseslabs.com/wp-content/uploads/2023/03/Lisinopril-480x360.jpg)




Leave a Comment