Learn about the nursing care management of patients with osteoarthritis in this nursing study guide.
Table of Contents
- What is Osteoarthritis?
- Classification
- Pathophysiology
- Statistics and Epidemiology
- Causes
- Clinical Manifestations
- Prevention
- Assessment and Diagnostic Findings
- Medical Management
- Surgical Management
- Nursing Management
- See Also
What is Osteoarthritis?
Osteoarthritis (OA) is the most frequently disabling among joint disorders.
- Osteoarthritis is a degenerative joint disease or sometimes called osteoarthrosis even though inflammation may be present.
- It is the most common among the joint disorders and also the most disabling.
- OA is both overdiagnosed and trivialized; it is frequently overtreated or undertreated.
- The functional impact of OA on the quality of life, especially elderly patients, is often ignored.
Classification
Osteoarthritis is classified into two classifications, yet the distinction between the two of them is always unclear.
- Primary or idiopathic OA has no prior event or disease related to it.
- Secondary OA results from previous joint injury or inflammatory disease.
Pathophysiology
Osteoarthritis may be thought of as the result of many factors that, when combined, predispose the patient to the disease.
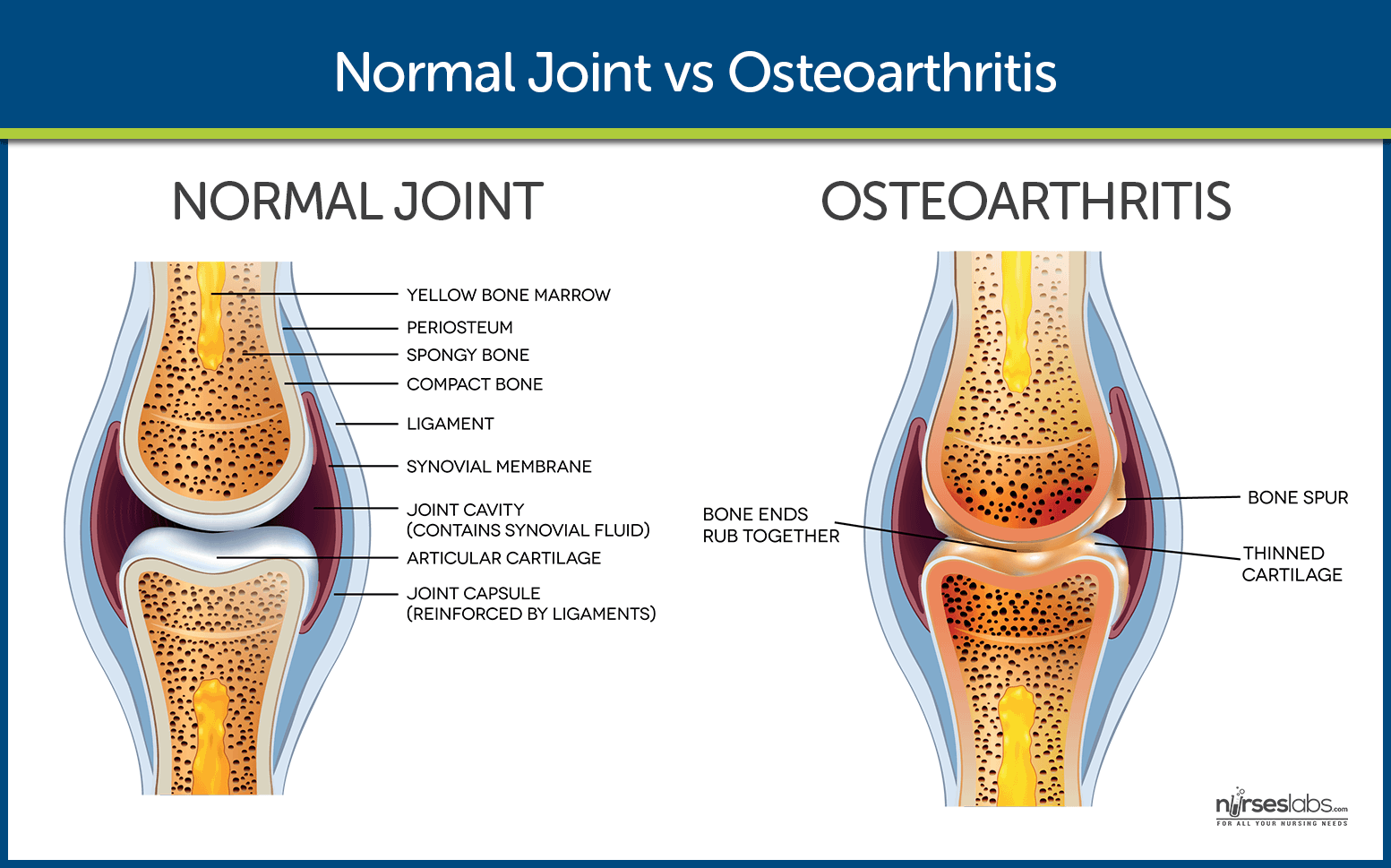
- Mechanical injury. OA starts from an injury of the articular cartilage, subchondral bone, and synovium.
- Chondrocyte response. Factors that initiate chondrocyte response include previous joint damage, genetic and hormonal factors, and others.
- Cytokines. After the chondrocyte response, the release of cytokines occurs.
- Stimulation of enzymes. Proteolytic enzymes, metalloproteases, and collagenase are stimulated, produced, and, released.
- Damage. The resulting damage predisposes to damage further as the chondrocyte is triggered to respond again.
Osteoarthritis by Osmosis
Check out this awesome pathophysiology and easy-to-understand video by Osmosis.
Statistics and Epidemiology
Osteoarthritis often begins with the third decade of life and peaks between the fifth and the sixth decades.
- By 40 years of age, 90% of the population has degenerative joint changes in their weight-bearing joints.
- Prevalence of OA is between 50% and 80% in the elderly.
- Increasing age directly relates to the degenerative process in the joint.
Causes
Understanding of osteoarthritis has been greatly expanded beyond what was previously thought of as simply “wear and tear” related to aging and the causes include:
- Increased age. Most elderly people experience osteoarthritis because the ability of the articular cartilage to resist microfracture with repetitive loads diminishes with age.
- Obesity. Obese people easily wear out their weight-bearing joints because of their increased weight.
- Previous joint damage. Having previous joint damage predisposes the patient to secondary OA.
- Repetitive use. Repetitive use due to occupational or recreational factors also causes OA.
Clinical Manifestations
Osteoarthritis has primary signs and symptoms, and that includes:
- Pain. Inflamed synovium causes the pain, stretching of the joint capsule or ligaments, irritation of the nerve endings in periosteum over osteophytes, trabecular microfracture, intraosseous, hypertension, bursitis, tendinitis, and muscle spasm.
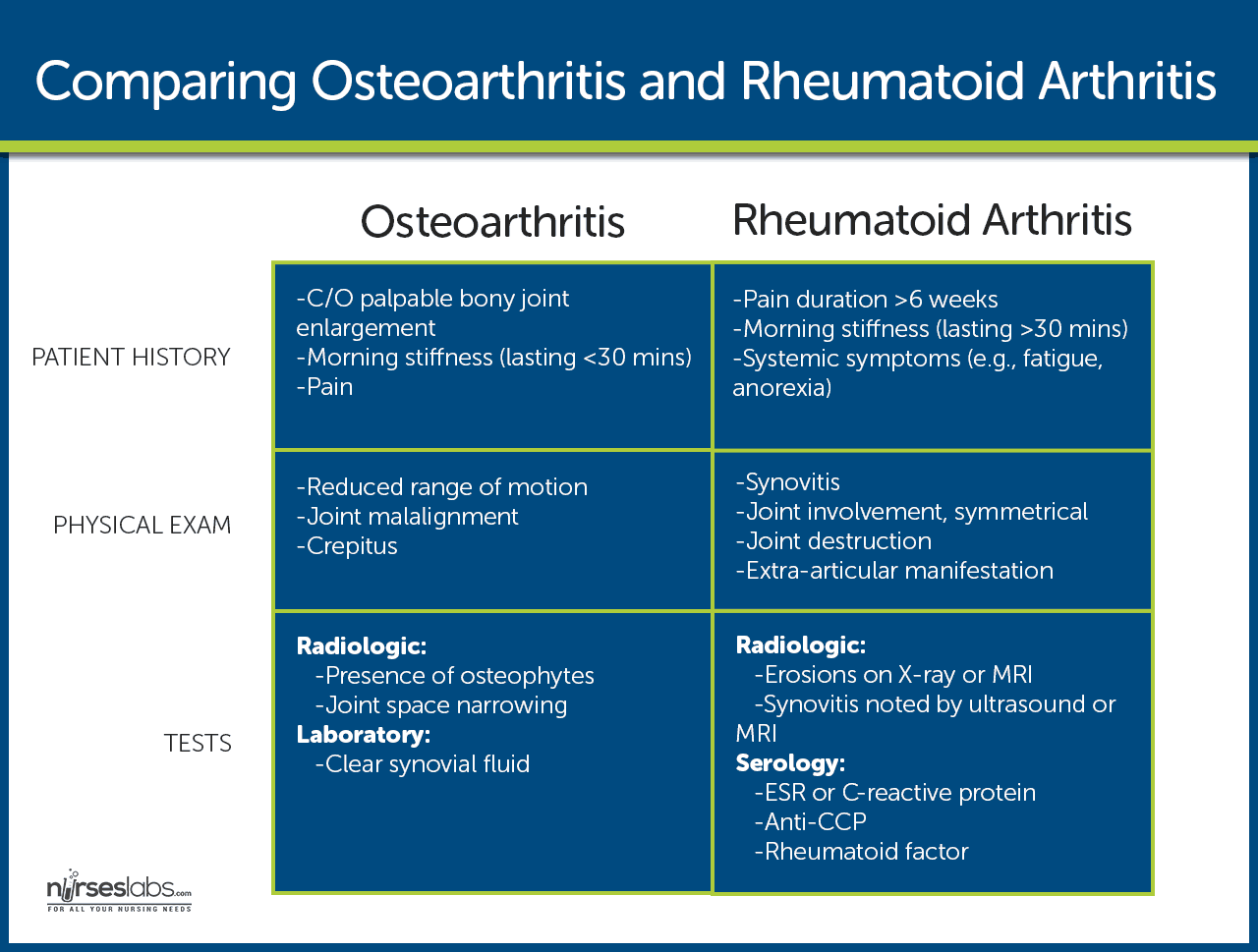
- Stiffness. Stiffness, which is mostly experienced in the morning or upon awakening, usually lasts less than 30 minutes and decreases with movement.
- Functional impairment. Functional impairment results from pain on movement and limited motion caused by structural changes in the joints.
Prevention
Although no treatment halts the degenerative process, certain preventive measures can slow the progress if undertaken early enough.
- Weight reduction. To avoid too much weight upon the joints, reduction of weight is recommended.
- Prevention of injuries. As one of the risk factors for osteoarthritis is previous joint damage, it is best to avoid any injury that might befall the weight-bearing joints.
- Perinatal screening for congenital hip disease. Congenital and developmental disorders of the hip are well known for predisposing a person to OA of the hip.
Assessment and Diagnostic Findings
Diagnosis of osteoarthritis is complicated only because of 30% of patients with changes seen on x-ray report symptoms.
- Physical assessment. Physical assessment of the musculoskeletal system reveals the tender and swollen joints.
- X-ray. OA is characterized by a progressive loss of joint cartilage, which appears on x-ray as a narrowing of the joint space.
Medical Management
Medical management involves conservative measures, physical modalities, and alternative therapies.
- Use of heat. To reduce the pain, heat application can be performed over the joints.
- Weight reduction. Weight reduction is strongly recommended for obese patients to avoid further damage to the cartilage.
- Joint rest. The patient should avoid joint overuse and rest the joints regularly.
- Orthotic devices. Devices such as splints and braces can be used to support inflamed joints.
- Pharmacologic therapy. Initial analgesic therapy is acetaminophen, while some are responsive to NSAIDs, COX-2 enzyme blockers, opioids, and intra-articular corticosteroids.
Surgical Management
In moderate to severe OA, when pain is severe or because of loss of function, surgical intervention may be used.
- Osteotomy. Osteotomy is performed to alter the distribution of weight within the joint.
- Arthroplasty. Diseased joint components are replaced in arthroplasty.
Nursing Management
Nursing management of the patient with osteoarthritis includes both nonpharmacologic and pharmacologic approaches.
Nursing Assessment
Nursing assessment for OA focuses mainly on history and physical assessment.
- Physical assessment. Assessment of the area over the affected joint may reveal tender and enlarged joints.
- Patient history. The nurse must take note of any past injury to the joints, as this is a risk factor for OA.
Diagnosis
Based on the assessment data, nursing diagnoses are:
- Acute pain related to inflammation of the synovium and irritation of the nerve endings.
- Activity intolerance related to joint pain.
- Impaired physical mobility related to joint stiffness.
Nursing Care Planning and Goals
Main Article: 4 Osteoarthritis Nursing Care Plans
After successful management, a patient with osteoarthritis will:
- Identify negative factors affecting activity intolerance and eliminate or reduce their effects when possible.
- Use identified techniques to enhance activity intolerance.
- Report measurable increase in activity intolerance.
- Report pain is relieved or controlled.
- Follow prescribed pharmacologic regimen.
- Participate in ADLs and desired activities.
Nursing Interventions
The major goals of the nursing intervention are pain management and optimal functional ability.
- Weight loss. Weight loss is an important approach to pain and disability improvement.
- Assistive devices. Canes and other ambulatory devices are very helpful for ambulation.
- Exercise. Exercises such as walking should begin moderately and increase gradually.
- Analgesic. Adequate pain management is essential to the success of an exercise program.
- Physical therapy. A referral for physical therapy for people with similar problems can be very helpful.
Evaluation
After the implementation of the care plan, success is evaluated if the client:
- Identified negative factors affecting activity intolerance and eliminate or reduce their effects when possible.
- Used identified techniques to enhance activity intolerance.
- Reported measurable increase in activity intolerance.
- Reported pain is relieved or controlled.
- Followed prescribed pharmacologic regimen.
- Participated in ADLs and desired activities.
Discharge and Home Care Guidelines
After discharge, management of OA should still continue at home.
- Exercise. Patients should plan their daily exercise for a time when the pain is least severe or plan to use a prescribed analgesic agent before exercising.
- Alternative therapies. The patient may use complementary or alternative therapies such as herbal and dietary supplements, special diets, acupuncture, acupressure, wearing copper bracelets or magnets, and participating in T’ai Chi.
- Medications. Prescribed medications by the physician should be taken compliantly, especially analgesics to avoid severe pain.
Documentation Guidelines
The focus of documentation should include:
- Level of activity.
- Causative or precipitating factors.
- Client reports of difficulty or change.
- Vital signs before, during, and following the activity.
- Description of response to pain, expectations of pain management, and acceptable level of pain.
- Prior medication use.
- Plan of care and those involved in the planning.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcomes.
- Modifications to the plan of care.
- Discharge and long-term need.
See Also
Posts related to Osteoarthritis:
It’s is very helpful for me ☺️ thanks you so much 😊
Thank you so much for this 🙂