Learn about the nursing care management of patients with benign prostatic hyperplasia in this nursing study guide.
What is Benign Prostatic Hyperplasia?
Benign prostatic hyperplasia (BPH) is one of the most common diseases in aging men.
- Benign prostatic hyperplasia (BPH) is the enlargement, or hypertrophy, of the prostate gland.
- The prostate gland enlarges, extending upward into the bladder and obstructing the outflow of urine. Incomplete emptying of the bladder and urinary retention leading to urinary stasis may result in hydronephrosis, hydroureter, and urinary tract infections (UTIs).
- The cause is not well understood, but evidence suggests hormonal involvement.
- BPH is common in men older than 40 years.
- It can cause bothersome lower urinary tract symptoms that affect quality of life by interfering with daily normal activities and sleep pattern.
Pathophysiology
The pathophysiology of BPH is as follows:
- Resistance. BPH is a result of complex interactions involving resistance in the prostatic urethra to mechanical and spastic effects.
- Obstruction. The hypertrophied lobes of the prostate may obstruct the bladder neck or urethra, causing incomplete emptying of the bladder and urinary retention.
- Dilation. Gradual dilation of the ureters and kidneys can occur.
- Schematic Diagram for Benign Prostatic Hyperplasia.
Statistics and Epidemiology
Here are the current statistics for BPH:
- BPH typically occurs in men older than 40 years of age.
- By the time they reach 60 years of age, 50% of men have BPH.
- BPH affects as many as 90% of men by 85 years of age.
- BPH is the second most common cause of surgical intervention in men older than 60 years of age.
Causes
The cause of BPH is not well understood, but testicular androgens have been implicated.
- Elevated estrogen levels. BPH generally occurs when men have elevated estrogen levels and when prostate tissue becomes more sensitive.
- Smoking. Smoking increases the risk of acquiring BPH.
- Reduced activity level. A sedentary lifestyle could also lead to the development of BPH.
- Western diet. A diet high in animal fat and protein and refined carbohydrates while low in fiber predisposes a man to BPH.
Clinical Manifestations
BPH may or may not lead to lower urinary tract symptoms; if symptoms occur, they may range from mild to severe.
- Urinary frequency. Frequent trips to the bathroom to urinate may be an early sign of a developing BPH.
- Urinary urgency. This is the sudden and immediate urge to urinate.
- Nocturia. Urinating frequently at night is called nocturia.
- Weak urinary stream. Decreased and intermittent force of stream is a sign of BPH.
- Dribbling urine. Urine dribbles out after urination.
- Straining. There is presence of abdominal straining upon urination.
Assessment and Diagnostic Findings
There are several ways to diagnose benign prostatic hypertrophy.
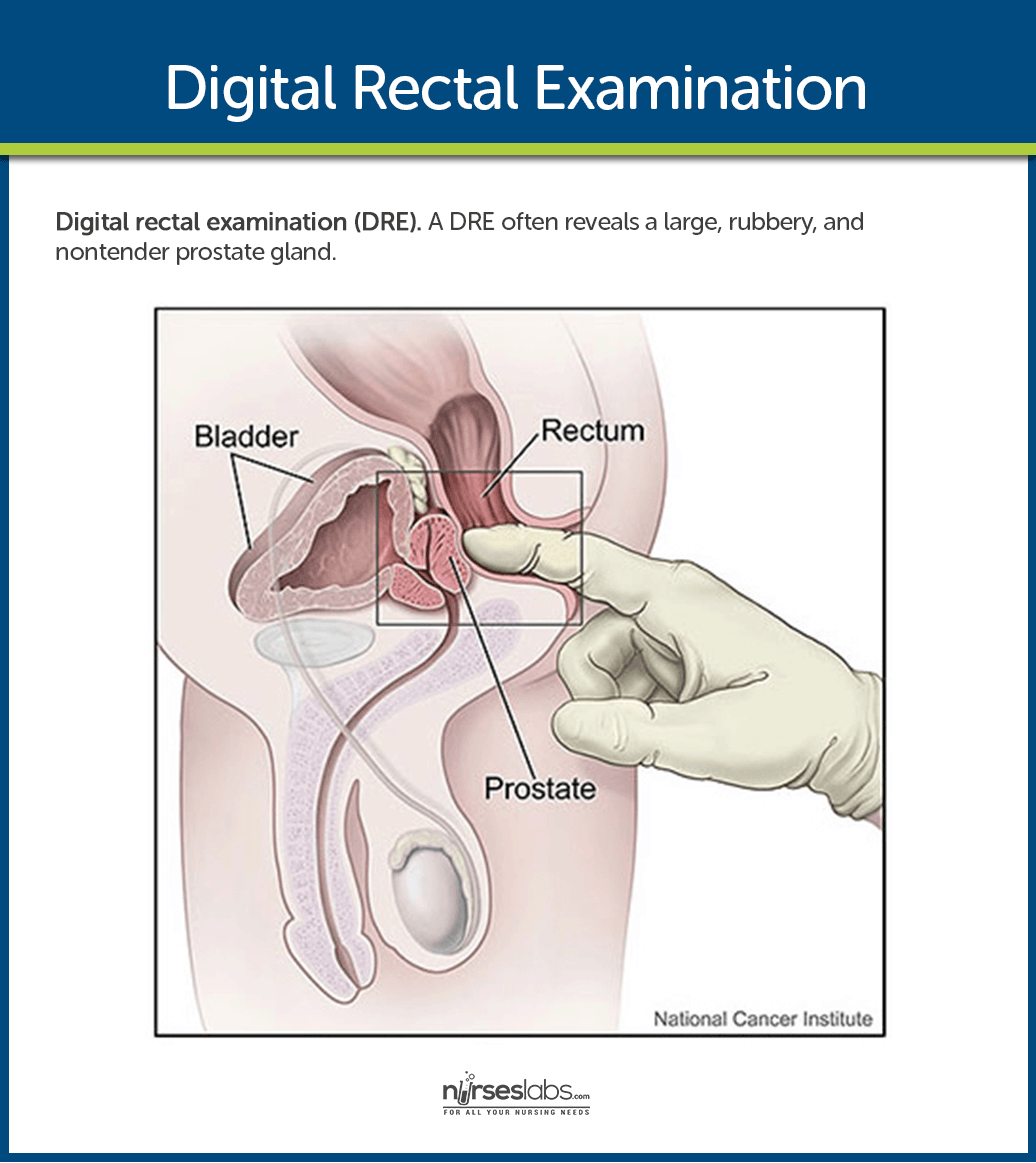
- Digital rectal examination (DRE). A DRE often reveals a large, rubbery, and nontender prostate gland.
- Urinalysis. A urinalysis to screen for hematuria and UTI is recommended.
- Prostate specific antigen levels. A PSA level is obtained if the patient has at least a 10-year life expectancy and for whom knowledge of the presence of prostate cancer would change management.
- Urinalysis: Color: Yellow, dark brown, dark or bright red (bloody); appearance may be cloudy. pH 7 or greater (suggests infection); bacteria, WBCs, RBCs may be present microscopically.
- Urine culture: May reveal Staphylococcus aureus, Proteus, Klebsiella, Pseudomonas, or Escherichia coli.
- Urine cytology: To rule out bladder cancer.
- BUN/Cr: Elevated if renal function is compromised.
- Prostate-specific antigen (PSA): Glycoprotein contained in the cytoplasm of prostatic epithelial cells, detected in the blood of adult men. Level is greatly increased in prostatic cancer but can also be elevated in BPH. Note: Research suggests elevated PSA levels with a low percentage of free PSA are more likely associated with prostate cancer than with a benign prostate condition.
- WBC: May be more than 11,000/mm3, indicating infection if patient is not immunosuppressed.
- Uroflowmetry: Assesses degree of bladder obstruction.
- IVP with post voiding film: Shows delayed emptying of bladder, varying degrees of urinary tract obstruction, and presence of prostatic enlargement, bladder diverticula, and abnormal thickening of bladder muscle.
- Voiding cystourethrography: May be used instead of IVP to visualize bladder and urethra because it uses local dyes.
- Cystometrogram: Measures pressure and volume in the bladder to identify bladder dysfunction unrelated to BPH.
- Cystourethroscopy: To view degree of prostatic enlargement and bladder-wall changes (bladder diverticulum).
- Cystometry: Evaluates detrusor muscle function and tone.
- Transrectal prostatic ultrasound: Measures size of prostate and amount of residual urine; locates lesions unrelated to BPH.
Medical Management
The goals of medical management of BPH are to improve the quality of life and treatment depends on the severity of symptoms.
- Catheterization. If a patient is admitted on an emergency basis because he is unable to void, he is immediately catheterized.
- Cystostomy. An incision into the bladder may be needed to provide urinary drainage.
Pharmacologic Management
- Alpha-adrenergic blockers (eg, alfuzosin, terazosin), which relax the smooth muscle of the bladder neck and prostate, and 5alpha reductase inhibitors.
- Hormonal manipulation with antiandrogen agents (finasteride [Proscar]) decreases the size of the prostate and prevents the conversion of testosterone to dihydrotestosterone (DHT).
- Use of phytotherapeutic agents and other dietary supplements (Serenoa repens [saw palmetto berry] and Pygeum africanum [African plum]) are not recommended, although they are commonly used.
- One herbal medication effective against BPH is Saw Palmetto.
Surgical Management
Other treatment options include minimally invasive procedures and resection of the prostate gland.
- Transurethral microwave heat treatment. This therapy involves the application of heat to prostatic tissue.
- Transurethral needle ablation (TUNA). TUNA uses low-level radio frequencies delivered by thin needles placed in the prostate gland to produce localized heat that destroys prostate tissue while sparing other tissues.
- Transurethral resection of the prostate (TURP). TURP involves the surgical removal of the inner portion of the prostate through an endoscope inserted through the urethra.
- Open prostatectomy. Open prostatectomy involves the surgical removal of the inner portion of the prostate via a suprapubic, retropubic, or perineal approach for large prostate glands.
Nursing Management
Nursing management of a patient with BPH includes the following:
Nursing Assessment
Nursing assessment focuses on the health history of the patient.
- Health history. The health history focuses on the urinary tract, previous surgical procedures, general health issues, family history of prostate diseases, and fitness for possible surgery.
- Physical assessment. Physical assessment includes digital rectal examination.
Nursing Diagnosis
Based on the assessment data, the appropriate nursing diagnoses for a patient with BPH are:
- Urinary retention related to obstruction in the bladder neck or urethra.
- Acute pain related to bladder distention.
- Anxiety related to the surgical procedure.
Nursing Care Planning & Goals
Main Article: 5 Benign Prostatic Hyperplasia (BPH) Nursing Care Plans
The goals for a patient with BPH include:
- Relieve acute urinary retention.
- Promote comfort.
- Prevent complications.
- Help patient deal with psychosocial concerns.
- Provide information about disease process/prognosis and treatment needs.
Nursing Interventions
Preoperative and postoperative nursing interventions for a patient with BPH are as follows:
- Reduce anxiety. The nurse should familiarize the patient with the preoperative and postoperative routines and initiate measures to reduce anxiety.
- Relieve discomfort. Bed rest and analgesics are prescribed if a patient experiences discomfort.
- Provide instruction. Before the surgery, the nurse reviews with the patient the anatomy of the affected structures and their function in relation to the urinary and reproductive systems.
- Maintain fluid balance. Fluid balance should be restored to normal.
Evaluation
- Reduced anxiety.
- Reduced level of pain.
- Maintained fluid volume balance postoperatively.
- Absence of complications.
Discharge and Home Care Guidelines
The patient and the family require instructions about how to promote recovery.
- Instructions. The nurse provides written and oral instructions about the need to monitor urinary output and strategies to prevent complications.
- Urinary control. The nurse should teach the patient exercises to regain urinary control.
- Avoid Valsalva maneuver. The patient should avoid activities that produce Valsalva maneuver like straining and heavy lifting.
- Avoid bladder discomfort. The patient should be taught to avoid spicy foods, alcohol, and coffee.
- Increase fluids. The nurse should instruct the patient to drink enough fluids.
Documentation Guidelines
The focus of the documentation in a patient with BPH includes:
- Degree of impairment.
- Client’s description in response to pain.
- Acceptable level of pain.
- Prior medication use.
- Level of anxiety and precipitating/aggravating factors.
- Description of feelings.
- Awareness and ability to recognize and express feelings.
- Treatment plan.
- Teaching plan.
- Client’s response to interventions, teaching, and actions performed.
- Attainment and progress toward desired outcomes.
- Modifications to plan of care.
- Referrals made.
Practice Quiz: Benign Prostatic Hyperplasia
Here’s a 5-item quiz about the study guide. Please visit our nursing test bank for more NCLEX practice questions.
1. Enlargement of the prostate gland, BPH, is usually associated with:
A. Dysuria.
B. Dilation of the ureters.
C. Hydronephrosis.
D. All of the above.
2. The incidence of BPH among men older than 60 years of age is:
A. 35%
B. 50%
C. 65%
D. 80%
3. The following are surgical procedures used in BPH except:
A. Prostatectomy.
B. TURP.
C. TUNA.
D. Circumcision.
4. A result of the digital rectal examination in a patient with BPH includes what findings?
A. Enlarged, tender prostate.
B. Large, rubbery prostate.
C. Small, nontender prostate.
D. Pus-covered prostate.
5. What is the surgical removal of the inner portion of the prostate through an endoscope inserted through the urethra?
A. Open prostatectomy.
B. TUNA.
C. DRE.
D. TURP.
Answers and Rationale
1. Answer: D. All of the above.
- D: All of the symptoms mentioned are associated with BPH.
- A: Dysuria is present in BPH.
- B: Dilation of the ureters is present in BPH.
- C: Hydronephrosis is present in BPH.
2. Answer: B. 50%.
- B: 50% of men who reach 60 years old develop BPH.
- A: The incidence of BPH among men older than 60 years of age is not 35%.
- C: The incidence of BPH among men older than 60 years of age is not 65%.
- D: The incidence of BPH among men older than 60 years of age is not 80%.
3. Answer: D. Circumcision.
- D: Circumcision is not used in BPH.
- A: Prostatectomy can be used in BPH.
- B: TURP. can be used in BPH.
- C: TUNA can be used in BPH.
4. Answer: B. Large, rubbery prostate.
- B: BPH manifests a large, nontender, rubbery prostate when assessed through DRE.
- A: The prostate in BPH is not tender.
- C: The prostate in BPH is not small.
- D: The prostate in BPH is not covered in pus.
5. Answer: D. TURP.
- D: TURP the surgical removal of the inner portion of the prostate through an endoscope inserted through the urethra.
- A: Open prostatectomy involves the surgical removal of the inner portion of the prostate via a suprapubic, retropubic, or perineal approach for large prostate glands.
- B: TUNA uses low-level radio frequencies delivered by thin needles placed in the prostate gland to produce localized heat that destroys prostate tissue while sparing other tissues.
- C: DRE is the manual palpation of the prostate via the rectum using the gloved fingers of the examiner.
See Also
Posts related to this study guide:















Leave a Comment