Fecal analysis is a noninvasive laboratory test useful in identifying disorders of the digestive tract. These disorders may include malabsorption, inflammation, infection (bacteria, viruses, or fungi), or cancer. It is performed in combination with blood work, physical examination, x-ray imaging, and endoscopy in order to confirm these conditions. The most common test done on a stool is called fecal occult blood test (FOBT) wherein it can detect traces of blood in the feces.
Feces is a solid body waste discharged from the large intestine through the anus by the process of defecation. It is made of cellulose and other indigestible food matter, water, and bacteria. Furthermore, other substances usually found in feces include epithelial cells shed from the gastrointestinal tract, small amounts of fats, bile pigments in the form of urobilinogen, GI and pancreatic secretions, electrolytes, and trypsin. Trypsin is a proteolytic enzyme produced in the pancreas.
About 100 to 300 gram of fecal material is being excreted by an average adult daily, the residue of approximately 10 liters of liquid material that enters the GI tract each day. The laboratory analysis of feces includes macroscopic examination (volume, odor, shape, color, consistency, the presence of mucus), microscopic examination (leukocytes, epithelial cells, meat fibers), and chemical tests for specific substances (occult blood, trypsin, estimation of carbohydrates).
The role of the nurses during a stool collection and fecal analysis are as follows: proper specimen collection and handling, accurate sample identification, ensure all supplies are appropriate for collection, and timely transport of specimen to the laboratory.
This fecal analysis study guide can help nurses understand their tasks and responsibilities when collecting a stool sample.
Indications of Fecal Analysis
Stool analysis is used to:
- Aid in diagnosing disorders related to gastrointestinal (GI) bleeding or medication therapy that results in bleeding
- Assist in the diagnosis of pseudomembranous enterocolitis following the use of broad-spectrum antibiotic therapy
- Help diagnose suspected inflammatory bowel syndrome (IBS)
- Identify the cause of diarrhea of unknown origin
- Investigate disorders of protein digestion
- Screen for colorectal cancer
- Screen for cystic fibrosis
- Determine intestinal parasitic infestation, as indicated by diarrhea of unknown cause
- Evaluate the effectiveness of therapeutic regimen for intestinal malabsorption or pancreatic insufficiency
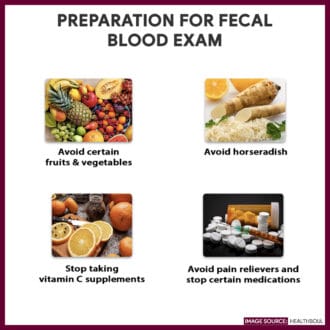
Interfering Factors
These are factors or conditions that may affect the outcome of the study:
- Medications that irritate the gastric mucosa such as non-steroidal anti-inflammatory medicines (NSAIDs), anticoagulants, colchicine, corticosteroids, phenylbutazone, and iron preparations can cause positive results for occult blood
- High doses of vitamin C (more than 250 mg per day) can cause false negative occult blood
- Dietary intake of high in red meat, certain vegetables (radish, turnips, cauliflower, broccoli), and fruits (bananas, apples, cantaloupe) can cause false-positive results for occult blood
- Constipated stools may not show any trypsin activity due to prolonged exposure to intestinal bacteria
Procedure for Stool analysis
The following are steps in collecting a stool specimen:
- Collect a fecal sample
Wear clean gloves and collect a stool specimen and put it directly in a leak-proof container with a tight-fitting lid. If the patient is bedridden, collect the specimen in a clean, dry bedpan, and then, using a tongue blade, transfer into a properly labeled container. If doing a rectal swab, insert the swab 2-3 cm through the rectal sphincter, rotate gently, and remove. Transfer swab in the container. - Fill out the test request form completely
Note on the laboratory request the patient’s demographics, stool consistency, and date and time of collection. Indicate previous or present antibiotic therapy and any pertinent history - Transport the specimen to the laboratory
Send the specimen to the laboratory immediately for processing and analysis. If a liquid or soft stool sample can’t be processed within 30 minutes of passage, placed in a preservative; If a formed stool specimen can’t be studied immediately, place it in a preservative or refrigerator.
Nursing Responsibility for Stool Analysis
The following are the nursing interventions and nursing care considerations for the patient
Before the procedure
The following are the nursing interventions prior to a stool analysis.
- Assess the patient’s level of comfort. Collecting stool specimen may produce a feeling of embarrassment and discomfort to the patient.
- Encourage the patient to urinate. Allow the patient to urinate before collecting to avoid contaminating the stool with urine.
- Avoid laxatives. Advise patient that laxatives, enemas, or suppositories are avoided three days prior to collection.
- Instruct a red-meat free and high residue diet. The patient is indicated for an occult blood test, must follow a special diet that includes generous amounts of chicken, turkey, and tuna, raw and uncooked vegetables and fruits such as spinach, celery, prunes and bran containing cereal for two (2) days before the test.
After the procedure
The nurse should note of the following nursing interventions after fecal analysis:
- Instruct patient to do handwashing. Allow the patient to thoroughly clean his or her hands and perianal area.
- Resume activities. The patient may resume his or her normal diet and medication therapy unless otherwise specified.
- Recommend regular screening. The American Cancer Society recommends yearly occult blood test as part of the screening for colorectal cancer starting at the age of 45 years old for people with average risk.
Normal Results
There are two methods where stool can be examined:
- Macroscopic examination: for appearance and color
- Microscopic examination: for cell count and presence of meat fibers; leukocyte esterase, for leukocytes; Benedict’s solution (copper sulfate) for reducing substances; guaiac, for occult blood; x-ray paper, for trypsin
| Characteristic of stool | Normal findings |
| Appearance | Solid and formed |
| Color | Brown |
| Epithelial cells | Few to moderate |
| Fecal fat | Less than 7 grams of fat per 24 hours |
| Leukocytes (white blood cells) | Negative |
| Meat fibers | Negative |
| Occult blood | Negative |
| Reducing substances | Negative |
| Trypsin | 2+ to 4 + |
Abnormal Results
Abnormal findings in a stool exam may reveal the potential medical diagnosis. These includes:
- Unusual appearance:
- Mucous: Intestinal wall inflammation
- Bloody: Excessive intestinal wall irritation or malignancy
- Frothy or bulky: Malabsorption
- Ribbonlike or slender: Obstruction
- Unusual color:
- Red: Beets and food coloring, lower GI bleed, phenazopyridine hydrochloride compounds, rifampicin
- Black: Bismuth (antacid) or charcoal ingestion, iron therapy, upper GI bleeding
- Yellow: Rhubarb
- Green: Antibiotics, biliverdin, green vegetables
- Grayish white: Barium ingestion, bile duct obstruction
- Increased:
- Blood: related to GI bleeding
- Occult blood: Diverticular disease, esophagitis, gastritis, esophageal varices, anal fissure, hemorrhoids, infectious diarrhea, inflammatory bowel disease, polyps, tumors, ulcers, Mallory-Weiss tears
- Leukocytes: Inflammation of the intestines related to bacterial infections of the intestinal wall, ulcerative colitis, shigellosis, or salmonellosis
- Epithelial cells: Inflammatory bowel disorders
- Carbohydrates/reducing substances: Inability to digest some sugar, malabsorption syndromes
- Fats: Sprue (celiac disease), cystic fibrosis related to malabsorption, pancreatitis
- pH: Related to inflammation in the intestine from colitis, cancer, or antibiotic use
- Meat fibers: Pancreatitis, impaired protein digestion
- Decreased:
- Leukocytes: Disorders resulting from toxins, cholera, viral diarrhea, amebic colitis, parasites
- Carbohydrates/reducing substances: Cystic fibrosis, sprue, malnutrition, medications such as colchicine or birth control pills
- pH: Related to poor absorption of carbohydrate or fat
- Trypsin: Malabsorption syndrome, pancreatic deficiency, cystic fibrosis
Gallery
Images related to Fecal Analysis (Stool Exam):






References and Sources
Additional resources and references for this guide:
- Anne M. Van Leeuwen, Mickey Lynn Bladh. Laboratory & Diagnostic Tests with Nursing Implications: Davis’s
- Davies, R. J., Miller, R., & Coleman, N. (2005). Colorectal cancer screening: prospects for molecular stool analysis. Nature Reviews Cancer, 5(3), 199. [Link]
- Suzanne C. Smeltzer. Brunner & Suddarth’s Handbook of Laboratory and Diagnostic Tests: Lippincott Williams & Wilkins

























Leave a Comment