Gastroenteritis, commonly known as the stomach flu, is a prevalent and often self-limiting gastrointestinal infection that is characterized by inflammation of the stomach and intestines, leading to symptoms such as nausea, vomiting, diarrhea, and abdominal cramps.
Gastroenteritis can be caused by various viral, bacterial, or parasitic pathogens, with viral agents being the most common cause. While typically mild and resolving on its own, gastroenteritis can lead to dehydration, especially in young children and older adults.
This article aims to serve as a comprehensive nursing guide to gastroenteritis, discussing its causes, symptoms, diagnostic methods, medical management, and nursing interventions.
What is Gastroenteritis?
Stomach flu is commonly referred to as gastroenteritis.
- Although often considered a benign disease, acute gastroenteritis remains a major cause of morbidity and mortality in children around the world, accounting for 1.34 million deaths annually in children younger than 5 years, or roughly 15% of all child deaths.
- Diarrhea may be mild, accompanied by slight dehydration, or it may be extremely severe, requiring prompt and effective treatment.
Pathophysiology
The 2 primary mechanisms responsible for acute gastroenteritis are:
- There is damage to the villous brush border of the intestine, causing malabsorption of intestinal contents and leading to osmotic diarrhea.
- There is a release of toxins that bind to specific enterocyte receptors and cause the release of chloride ions into the intestinal lumen, leading to secretory diarrhea.
- Even in severe diarrhea, however, various sodium-coupled solute co-transport mechanisms remain intact, allowing for the efficient reabsorption of salt and water.
- By providing a 1:1 proportion of sodium to glucose, classic oral rehydration solution (ORS) takes advantage of a specific sodium–glucose transporter (SGLT-1) to increase the reabsorption of sodium, which leads to the passive reabsorption of water.
Statistics and Incidences
Gastroenteritis is prevalent in areas lacking adequate clean water and sanitation facilities.
- Children in the United States experience, on average, 1.3-2.3 episodes of diarrhea each year.
- Overall, acute gastroenteritis accounts for than 1.5 million outpatient visits, 220,000 hospitalizations, and direct costs of more than $2 billion each year in the United States alone.
- Worldwide, children younger than 5 years have an estimated 1.7 billion episodes of diarrhea each year, leading to 124 million clinic visits, 9 million hospitalizations, and 1.34 million deaths, with more than 98% of these deaths occurring in the developing world.
- Although the prevalence of acute gastroenteritis in children has changed little over the past 4 decades, mortality has declined sharply, from 4.6 million in the 1970s to 3 million in the 1980s and 2.5 million in the 1990s.
Causes
Gastroenteritis may be caused by the following, yet it may be difficult to determine the causative factor in many instances:
- Infectious agents. The infectious organisms may be salmonella, Escherichia coli, dysentery bacilli, and various viruses, most notably rotaviruses.
- Contaminated food. Many diarrheal disturbances in children are caused by contaminated food or human or animal fecal waste through the oral-fecal route.
- Unsanitary water and environment. This condition is prevalent in areas lacking adequate clean water and sanitary facilities.
- Antibiotic therapy. Diarrhea may also be caused by antibiotic therapy.
Clinical Manifestations
Gastroenteritis may present the following:
- Diarrhea. Frequent, watery stools are more consistent with viral gastroenteritis, while stools with blood or mucous are indicative of a bacterial pathogen.
- Vomiting. When symptoms of vomiting predominate, one should consider other diseases such as gastroesophageal reflux disease (GERD), diabetic ketoacidosis, pyloric stenosis, acute abdomen, or urinary tract infection.
- Dysuria. Determine if there is an increase or decrease in the frequency of urination as measured by the number of wet diapers, time since last urination, color and concentration of urine, and presence of dysuria.
- Abdominal pain. In general, pain that precedes vomiting and diarrhea is more likely to be due to abdominal pathology other than gastroenteritis.
- Infection. Determine the presence of fever, chills, myalgias, rash, rhinorrhea, sore throat, cough, known immunocompromised status.
Assessment and Diagnostic Findings
The vast majority of children presenting with acute gastroenteritis do not require serum or urine tests, as they are unlikely to be helpful in determining the degree of dehydration.
- Stool exam. Stool specimens may be collected for culture and sensitivity testing to determine the causative infectious organism, if there is one.
Medical Management
Medical treatment for gastroenteritis includes:
- Oral rehydration solution. The American Academy of Pediatrics (AAP), the European Society of Pediatric Gastroenterology and Nutrition (ESPGAN), and the World Health Organization (WHO) all recommend oral rehydration solution (ORS) as the treatment of choice for children with mild-to-moderate gastroenteritis in both developed and developing countries.
- NG feeding. For patients who do not tolerate ORS by mouth, nasogastric (NG) feeding is a safe and effective alternative.
- IV rehydration. IV access should be obtained in severe dehydration and patients should be administered a bolus of 20-30 mL/kg lactated Ringer (LR) or normal saline (NS) solution over 60 minutes.
- Diet. In general, children with gastroenteritis should be returned to a normal diet as rapidly as possible; early feeding reduces illness duration and improves nutritional outcome.
Pharmacologic Management
The goals of pharmacotherapy are to reduce morbidity, prevent complications, and provide prophylaxis.
- Vaccines. In February 2006, the US Food and Drug Administration (FDA) approved the RotaTeq vaccine for the prevention of rotavirus gastroenteritis.
- Metronidazole. Metronidazole is recommended as the treatment of choice for mild-to-moderate cases of C difficile colitis.
- Antiemetics. A review of 7 randomized, controlled trials in children found that oral ondansetron reduced vomiting and the need for intravenous (IV) rehydration and hospital admission, IV ondansetron and metoclopramide reduced the number of episodes of vomiting and hospital admission, and dimenhydrinate suppository reduced the duration of vomiting.
Nursing Management
Nursing management in a child with gastroenteritis includes:
Nursing Assessment
Assessment of a child with gastroenteritis includes:
- Assess stool characteristics. In addition to basic information about the child, the interview with the family must include specific information about the history of bowel patterns and the onset of diarrheal stools, with details on the number and type of stools per day; suggest terms to describe the color and odor of stools to assist the caregiver with descriptions.
- Assess for vomiting. Inquire about recent feeding patterns, nausea, and vomiting.
- Assess for the presence of illness. Ask the caregiver about fever and other signs of illness in the child and signs of illness in any other family members.
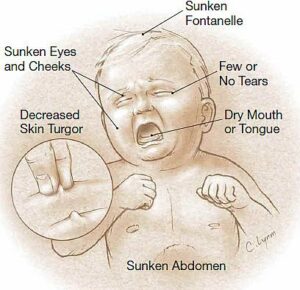
- Physical examination. The physical exam of the child includes observation of skin turgor and condition, including excoriated diaper area, temperature, anterior fontanelle, apical pulse rate, stools, irritability, lethargy, vomiting, urine, lips and mucous membranes of the mouth, eyes, and any notable physical signs.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Risk for infection related to inadequate secondary defenses or insufficient knowledge to avoid exposure to pathogens.
- Impaired skin integrity related to the constant presence of diarrheal stools.
- Deficient fluid volume related to diarrheal stools.
- Imbalanced nutrition: less than body requirements related to malabsorption of nutrients.
- Hyperthermia related to dehydration.
- Risk for delayed development related to decreased sucking when the infant is on NPO.
Nursing Care Planning and Goals
Main Article: 4 Gastroenteritis Nursing Care Plans
The major goals for a child with acute gastroenteritis are:
- Control of diarrhea.
- Minimize the risk for infection.
- Maintain good skin condition.
- Improve hydration and nutritional intake.
- Satisfy sucking needs in the infant.
- Eliminate the risk of infection transmission.
Nursing Interventions
Nursing interventions for a child with gastroenteritis are:
- Reduce infection transmission. All caregivers must wear gowns; gloves are used when handling articles contaminated with feces; place contaminated linens and clothing in specially marked containers to be processed according to facility policy; visitors are limited to family only; teach the family caregivers the principles of aseptic technique and observe them; and good handwashing must be carried out.
- Promote skin integrity. To reduce irritation and excoriation of the buttocks and genital area, cleanse those areas frequently and apply a soothing protective preparation such as lanolin A or D ointment; change diapers as quickly as possible, and placing disposable pads under the infant can facilitate easy and frequent changing.
- Prevent dehydration. Carefully count diapers and weigh them to determine the infant’s output accurately; measure each voiding in the older child; document the number and character of the stools, as well as the amount and character of any vomitus.
- Maintain adequate nutrition. Weigh the child daily on the same scale; take measurements in the early morning before the morning feeding; monitor the intake and output strictly; good mouth care is essential when the child is NPO; when oral fluids are started, the child is given oral replacement solutions; after the child tolerates these solutions, a half-strength formula may be introduced.
- Maintain body temperature. Monitor vital signs at least every 2 hours if there is a fever; follow appropriate procedures for fever reduction, and administer antipyretics and antibiotics as prescribed.
Evaluation
Goals are met as evidenced by:
- Control of diarrhea.
- Minimized risk for infection.
- Maintained good skin condition.
- Improved hydration and nutritional intake.
- Satisfied sucking needs in the infant.
- Eliminated risk of infection transmission.
Documentation Guidelines
Documentation in a child with gastroenteritis includes:
- Individual findings include factors affecting, interactions, the nature of social exchanges, and specifics of individual behavior.
- Intake and output.
- Characteristics of stool and vomitus.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.





























Leave a Comment