Betty Neuman (September 11, 1924 – May 28, 2022) was a nursing theorist who developed the Neuman Systems Model, a widely used conceptual framework that presents a holistic view of patients. She dedicated many years to perfecting this system’s model, which views patients as open systems interacting with stressors in their environment. Neuman drew on theories from various disciplines and applied her clinical and teaching expertise to develop the Neuman Systems Model, which has been adopted in nursing curricula and practice worldwide.
Biography of Betty Neuman
Early Life
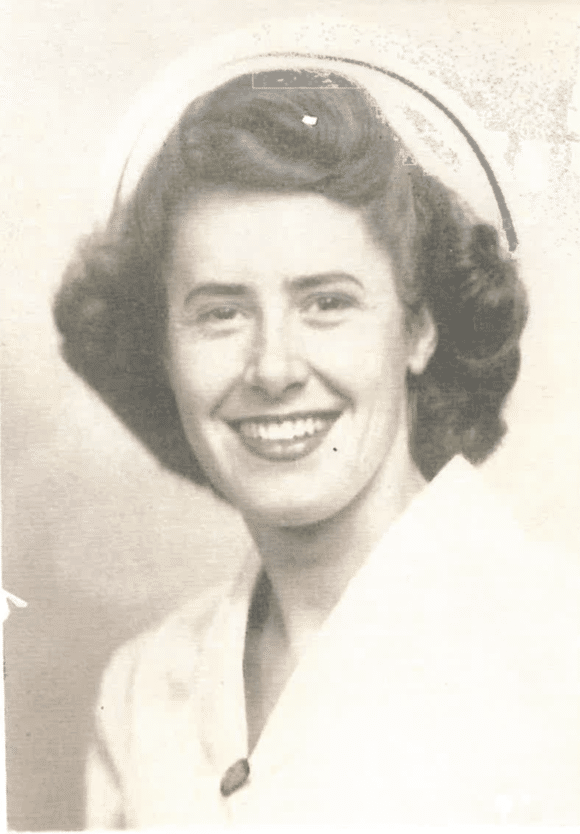
Betty Neuman was born on September 11, 1924, near Lowell, Ohio. She grew up on a farm, an upbringing that encouraged her desire to help people in need. Her interest in nursing began early as a young girl; she helped care for her ailing father, an experience that fostered compassion and set her on the path to a career in healthcare.
Family Background
Neuman’s father, a farmer, passed away at age 36. Her mother, a self-taught midwife, frequently traveled to care for others, influencing Neuman’s dedication to nursing. Betty was the middle child with two brothers.Betty Neuman was married and had a daughter in 1959. Aside from nursing, she also worked briefly as a fashion model and learned to fly a plane, reflecting her adventurous spirit and versatility.
Education
Neuman attended a one-room schoolhouse before earning her Registered Nurse diploma from Peoples Hospital School of Nursing in Akron, Ohio, in 1947. She later completed a Bachelor’s degree in Public Health and Psychology at UCLA in 1957, a Master’s degree in Mental Health and Public Health Consultation in 1966, and a PhD in Clinical Psychology from Pacific Western University in 1985.
Nursing Career of Betty Neuman

Betty Neuman’s early career took her to California, where she gained broad experience in nursing. She worked as a hospital staff nurse and head nurse at Los Angeles County General Hospital, served as a school nurse and an industrial (occupational health) nurse, and became a clinical instructor at the University of Southern California Medical Center in Los Angeles.
Neuman’s career flourished as she took on leadership roles and developed innovative nursing programs. She was appointed department chair at UCLA’s School of Nursing graduate program and later developed the first community mental health nursing program for graduate students in the Los Angeles area.
In 1985, she was also among the first to establish the role of nurse counselor in community crisis centers alongside her colleague Donna Aquilina. Furthermore, she maintained a private practice as a marriage and family therapist, specializing in Christian counseling.
Her contributions to the nursing profession were widely recognized, and she earned fellowships from the American Association of Marriage and Family Therapy and the American Academy of Nursing. In 1988, Neuman founded the Neuman Systems Model Trustees Group, Inc. to preserve and promote her model’s application in health care. Even after stepping down from leadership in 2009, she continued serving as a consultant, reflecting her lifelong commitment to nursing innovation and holistic care.
Works and Contributions of Betty Neuman
In 1970, while teaching at UCLA, Betty Neuman designed a preliminary nursing conceptual model to help students consider client variables beyond the limitations of the traditional medical model. She shared her early concepts with other nursing theorists, such as Joan Riehl-Sisca and Sr. Callista Roy, who incorporated Neuman’s ideas into their 1971 book, Conceptual Models for Nursing Practice. By 1972, Neuman had compiled a draft of her own model.
A decade of refinement followed. In 1982, Neuman published the first edition of her book The Neuman Systems Model: Application to Nursing Education and Practice, which formally presented her model to the nursing world. She continued to revise and expand the theory in subsequent editions and publications. As a prolific speaker and author, Neuman spent countless hours teaching the model’s concepts to students, clinicians, and fellow educators. She consulted nationally and internationally on implementing the model in nursing curricula and clinical practice settings.

Awards and Honors of Betty Neuman

Betty Neuman played many roles throughout her life: nurse, educator, health counselor, therapist, author, speaker, and researcher, and received numerous honors for her contributions. She was awarded several honorary doctorates (for example, an Honorary Doctorate of Letters from Neumann College in 1992 and an Honorary Doctorate of Science from Grand Valley State University in 1998). She was named an honorary member of the Fellowship of the American Academy of Nursing.
Neuman was honored by Walsh University’s Byers School of Nursing with a Distinguished Service Medal for her outstanding service to others. At the first annual Nursing Research Day at Walsh University, the Neuman Award (named in her honor) was presented to recognize outstanding service in the nursing profession. These accolades reflect the profound impact of her work on the nursing profession worldwide.

Death
In her final years, Betty Neuman resided near Seattle, Washington, having relocated there to be closer to her family. Even in retirement, she remained engaged with the nursing community, offering guidance and support through the Neuman Systems Model Trustees Group, which she established to preserve and promote her holistic approach to nursing care. Her dedication to integrating physiological, psychological, sociocultural, developmental, and spiritual factors in patient care continued to influence nursing education and practice worldwide. She passed away peacefully on May 28, 2022, at the age of 97.
Betty Neuman’s Nursing Theory
Three words often used to describe stress are inevitable, painful, and intensifying. Stress is generally subjective, and individuals may perceive similar events in very different ways. Betty Neuman’s nursing theory was built around people’s relationship to stress, their responses to it, and the reconstitution (recovery) factors that follow stressful events.
The Neuman Systems Model offers a comprehensive, holistic, systems-based perspective for nursing, with a focus on maintaining the flexibility and stability of the client system in the face of stressors. It presents a method of nursing that is proactive about preventing stress or minimizing its effects through appropriate interventions. In Neuman’s model, the client system’s responses to actual or potential environmental stressors are the central concern, and nursing actions are aimed at maintaining system stability through primary, secondary, and tertiary prevention.
What is the Neuman Systems Model?
Betty Neuman’s model views a person (or client) as an open system that is constantly interacting with both internal and external environments. She described the Neuman Systems Model as “a unique, open-system-based perspective that provides a unifying focus for approaching a wide range of concerns… A client system in interaction with the environment delineates the domain of nursing concerns.” In other words, any system (whether an individual, family, group, or community) can be considered a client in this model, and the boundary of that system plus its interaction with the environment is where nursing has influence.
The Neuman Systems Model conceptualizes the client holistically by identifying five variables that make up the client system: physiological, psychological, sociocultural, developmental, and spiritual aspects. These variables are seen as interrelated components of the whole person (or group) and are considered simultaneously in care, rather than in isolation. The model emphasizes that the client system is dynamic and constantly changing, moving along a wellness–illness continuum in response to environmental interactions.
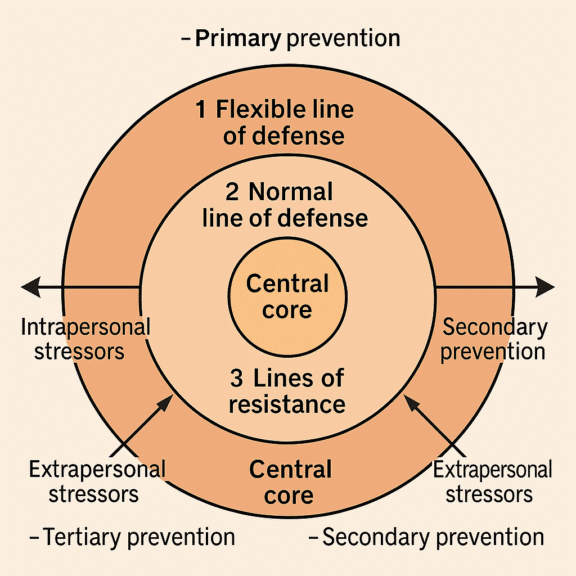
At the core of the client system is a basic structure or central core (sometimes called the basic survival factors common to all human beings, such as innate or genetic features, strengths, and weaknesses of the system). Surrounding this core are protective mechanisms known as lines of defense and lines of resistance. Neuman envisioned these as concentric circles or layers:
- The normal line of defense is the client’s normal state of wellness. It’s the standard level of health that the system has evolved to. This standard line of defense acts as a baseline for assessing any health deviation.
- The flexible line of defense is like a protective buffer, a dynamic “accordion-like” barrier at the outer boundary of the system that expands or contracts to protect the normal line of defense from invasion by stressors. It’s the first line of protection; for example, healthy lifestyle practices can act as a flexible defense against potential stress.
- The lines of resistance are internal mechanisms that activate when a stressor has penetrated the normal line of defense. These are protective factors inside the system (such as the immune response or coping mechanisms) that attempt to stabilize the client and foster a return to a steady state.
Assumptions of the Neuman Systems Model
Neuman’s Systems Model is built on a set of assumptions—accepted truths—that guide its perspective. These include:
- Holistic Client. Each client/client system is unique, a composite of the five variables in a certain configuration. The client’s response to stressors will vary within a normal range of reactions.
- Stressors are Ubiquitous. Many known, unknown, and universal stressors exist, and each has a differing potential to disturb the client’s usual stability (normal line of defense). The particular interrelationships of a client’s variables at any given time will affect how much the flexible line of defense can protect against a stressor.
- Normal Stability Range. Each client system has an established normal line of defense, the normal range of responses to the environment. This can be used as a standard for measuring health deviations. Wellness is the condition in which the system’s needs are met and energy is sufficient for stability.
- Penetration of Defenses. If the flexible line of defense can no longer protect the system, a stressor will breach the normal line of defense. When this happens, the system’s balance is threatened, and a reaction occurs.
- Dynamic Nature. Whether in a state of wellness or illness, the client system is a dynamic composite of the interrelations of its variables. The system is in a constant state of energy exchange with the environment. Input of energy (e.g., food, support, education) and output of energy (e.g., work, growth, healing processes) are continuously occurring.
- Lines of Resistance. Implicit within each client system are internal resistance factors (lines of resistance) that activate when stressors breach the normal line of defense. These factors help the system attempt a return to stability by restoring the wellness state.
- Prevention as Intervention. Neuman’s model assumes that prevention is the primary nursing intervention. It can occur at three levels:
- Primary prevention occurs before the system reacts to a stressor. It involves strengthening the flexible line of defense by promoting client wellness and protecting against stressors (for example, through health promotion, risk factor reduction, and education).
- Secondary prevention occurs after the system has reacted to a stressor. It focuses on treating symptoms, strengthening the internal lines of resistance, and preventing further damage by eliminating or reducing the stressor. The goal here is to regain optimal stability as quickly as possible.
- Tertiary prevention occurs after secondary interventions, when the client is moving back toward stability (reconstitution is in progress). Tertiary prevention supports the rehabilitative processes, using education or adaptive measures to maintain wellness or protect the system’s new balance. Tertiary prevention often leads back into primary prevention in a continuous cycle, as maintaining stability will involve ongoing wellness strategies.
- These assumptions set the stage for how a nurse using the Neuman Systems Model would assess a patient, identify problems, and plan care. Essentially, the nurse looks holistically at the client system, identifies actual or potential stressors and the state of the client’s lines of defense, and then implements preventive interventions at the appropriate level to either prevent stressors from occurring, manage the reaction, or support recovery.
Major Concepts of Neuman Systems Model
In the Neuman Systems Model, the four metaparadigm concepts of nursing (human being, environment, health, and nursing) are specifically defined, along with additional key concepts unique to the systems model (such as open system, basic structure, lines of defense, etc.). Below are the major concepts and Neuman’s definitions of them.
Human Being (Client System)
The human being (or client) is viewed as an open system that interacts with internal and external environmental forces or stressors. The person is in a constant state of change, moving toward a dynamic state of system stability or toward varying degrees of illness at any given time. The client system can be an individual, a family, a group, a community, or even a social issue; any defined system that can be the focus of nursing care. Neuman’s model, therefore, can apply from the micro level (one person) to the macro level (society), which gives it great flexibility.
Environment
The environment is the totality of internal and external forces surrounding the client, and it is integral to the system’s function. Neuman identifies three types of environments that influence the client system.
- Internal environment. All forces or stressors that are within the client system boundaries. These could be internal psychological processes, internal physiologic conditions, or any other internal factors.
- External environment. All forces or stressors outside the client system. This includes interpersonal interactions (close external factors, such as family, friends, or caregivers) and extrapersonal factors (more distant or broad external factors, such as community conditions, financial situations, or societal policies).
- Created environment. This refers to the environment that the client unconsciously establishes and which symbolizes their perceptions. It’s a buffer that the client uses to support protective coping. For example, a person’s sense of hope or spiritual faith might create an environment that helps cushion the impact of stress.
These environmental factors constantly interact with the client system. A key point is that the environment and the system have a reciprocal relationship: the environment affects the system (through stressors), and the system can, in turn, have effects on its environment (through output, such as influencing family or community).
Health
In Neuman’s model, health is defined as the degree of system stability and is seen as a continuum from wellness to illness. Optimal wellness is when the client’s needs are fully met and the variables are in harmony, that is, the system is stable and negentropic (gaining energy and complexity). Illness, on the other hand, represents a state where needs are not met, and the system is entropic (losing energy and moving toward disorganization). Death is the extreme end of illness, when the system lacks the energy needed to sustain life.
Thus, health in the Neuman Systems Model isn’t simply the absence of disease; it is the client’s position on the wellness-illness spectrum at any point in time. Nursing actions within this model aim to move the client toward the wellness end of the spectrum by strengthening defenses and reducing stressors.
Nursing
Neuman defined the role of nursing as concerned with the whole person. Nursing’s primary aim is to help the client system retain or regain stability in the face of stressors. This involves accurately assessing the effects of environmental stressors on the client and identifying appropriate preventive interventions. In practice, the nurse using Neuman’s model will.
- Determine the client’s baseline normal defense line (i.e., their usual state of health).
- Assess actual and potential stressor factors (intra-, inter-, and extrapersonal) that might penetrate the client’s defenses.
- Evaluate the client’s flexible line of defense; for instance, how strong are the client’s immediate coping mechanisms or support systems at the moment?
- Identify symptoms or reactions that indicate a stressor has broken through (if it has).
- Plan interventions at the proper prevention level.
- Primary prevention to protect the client against a stressor (e.g., health promotion activities, risk education, fortifying resources).
- Secondary prevention to alleviate or treat symptoms after a stressor reaction (e.g., providing care or medication, crisis intervention, removing the stressor).
- Tertiary prevention to support rehabilitation and return to wellness after treatment (e.g., teaching lifestyle modifications after an illness, providing ongoing support groups).
Overall, nursing actions are geared toward helping the system adapt, adjust, and reconstitute after stress, to maintain optimal stability of the client system. Because the model is holistic, the nurse considers all five client variables in the plan of care and works to conserve the client’s energy by reducing the demands (stressors) placed on the system.
Open System
An open system is a system in which there is a continuous flow of input (from the environment) and output (from the system), as well as ongoing feedback loops. All living organisms, including human beings and groups, are considered open systems in Neuman’s model. This means they are not isolated: they exchange energy, matter, and information with their environment. Because of this openness, the system is subject to constant change. Stability is an ongoing process rather than a fixed point. Understanding the client as an open system underpins why prevention and adaptation are so important; change is constant and cannot be avoided, so the focus is on how to deal with change (stress) healthily.
Basic Structure and Energy Resources
The basic structure (or central core) of the client system comprises the fundamental survival factors common to all humans. These include the innate or genetic features, strengths, and weaknesses of the system’s components, as well as the basic system’s energy resources. Some examples might be the individual’s temperature regulation ability, genetic predispositions, ego structure, or physiologic integrity of organs; core aspects without which the system would not survive.
Around this basic core are the lines of defense and resistance, as previously described, which protect the core. Neuman’s model implies that the basic structure has certain energy resources an inherent energy supply that the person has for maintaining life processes and wellness. When stressors impact the system, they can affect these energy resources. Part of the nursing goal is to protect and restore the basic structure’s energy by preventing stressors from depleting it. (Neuman mentioned various energy sources in her model; later scholars have noted it would be helpful if all such energy sources were clearly enumerated, as this could generate specific interventions to support a client’s energy needs.)
Client Variables
As noted earlier, Neuman considers five client variables that must be addressed simultaneously for a holistic understanding of the client system.
- Physiological variable. The physical structure and bodily functions of the client (e.g., oxygenation, nutrition, sleep, etc.).
- Psychological variable. Mental processes and emotional aspects (e.g., cognition, emotions, self-esteem, mindset).
- Sociocultural variable. The effects of social and cultural conditions (e.g., relationships, family structure, cultural beliefs, economic factors).
- Developmental variable. The life development stage and associated tasks (e.g., infant, adolescent, adult, older adult; each stage has different typical stressors and needs).
- Spiritual variable. The influence of spiritual or religious beliefs and values (e.g., hope, faith, meaning-making). Neuman was one of the theorists who explicitly included spirituality as a key component of a person’s system.
Defense Lines
Flexible line of defense
The flexible line of defense is described as a protective, dynamic buffer for the client’s normal wellness state. Neuman often visualized it as a layer beyond the normal line of defense, imagine a band or outer ring that can expand or contract. Its function is to temporarily absorb or offset the impact of stressors, preventing them from penetrating the normal line of defense. The flexibility of this line can be influenced by various factors, including an individual’s overall health, coping style, social support, sleep patterns, and nutrition, among others. For example, a well-rested, well-supported person may have a “thicker”, more flexible defense and can handle more stress without becoming ill. In contrast, exhaustion or isolation might thin that defense.
Normal line of defense
The normal line of defense represents the client’s normal or habitual level of wellness. It’s essentially the standard state of equilibrium for that system, developed over time. This line can be thought of as the level of health or adaptation to which the system has evolved and usually maintains. It can change over long periods: for instance, someone who has managed a chronic illness for years might have a new “normal” baseline that includes that condition. The normal line of defense is what the flexible line of defense is trying to protect. When stressors reach this level, the system’s stability is directly threatened, and symptoms of stress or illness will appear unless the lines of resistance can counteract them.
Lines of resistance
The lines of resistance are internal protective mechanisms that activate in response to stressors penetrating the normal line of defense. Think of these like the body’s immune response or a person’s problem-solving abilities kicking in during a crisis. They are strengths or factors within the client that help restore stability. For example, an immune system fighting off infection, the mobilization of psychological coping mechanisms, or the recruitment of extra help from the community could all be seen as lines of resistance in action. If these lines of resistance succeed, the system may re-establish stability (perhaps at the cost of energy). If they fail, the core of the system can be damaged.
Subconcepts of Neuman Systems Model
The Neuman Systems Model also elaborates several subconcepts, many of which we have described above in context. These include the nature of stressors, the idea of stability as the outcome of successful coping, the degree of reaction indicating system instability, the processes of entropy and negentropy in moving along the wellness-illness continuum, the exchange of input/output between the system and environment, and the concept of reconstitution as the system’s return to stability. Moreover, Neuman emphasizes “prevention as intervention,” highlighting that preventive measures at the primary, secondary, and tertiary levels are the primary nursing actions to maintain system stability.
Stressors and Client Perception
Stressors are defined in Neuman’s model as any environmental forces (internal or external) that have the potential to disrupt the stability of the system. Stressors can arise from:
- Intrapersonal sources (originating within the client, such as a thought or a pathological process),
- Interpersonal sources (arising from interactions immediately outside the client, e.g., family conflicts),
- Extrapersonal sources (distal external factors, such as financial troubles or societal policies).
Importantly, Neuman recognized that a stressor may produce either a positive or negative outcome once it impacts the client system. A distinctive aspect of Neuman’s theory is the emphasis on the client system’s perception of each stressor, the same stressor might be perceived as beneficial (a positive challenge) or as noxious (a threat), or a combination of both. It is this perception that largely determines the system’s response and the needed nursing interventions. For example, one patient might view a new diagnosis as a motivator to improve health (a positive stressor). In contrast, another might feel overwhelmed and discouraged by the same diagnosis (a negative stressor). In practice, the nurse assesses the client’s perception of the stressor to set appropriate wellness goals and prevention-as-intervention strategies to achieve those goals.
When a stressor penetrates the flexible line of defense and encounters the normal line of defense, the client system is said to have a reaction. The degree to which the system is affected is called the degree of reaction, essentially measuring how much the stressor disrupts the system’s stability. If the system’s lines of resistance are effective, they may reduce the degree of reaction by fighting off the stressor’s impact.
Health as a Continuum: Negentropy and Entropy
Neuman described health as a continuum of wellness to illness, where wellness is the condition in which all system parts are in harmony (optimal stability), and illness is a state of instability or energy depletion. A move toward wellness is associated with increasing organization and energy (what Neuman called negentropy), whereas movement toward illness reflects disorganization and energy loss (entropy). (It should be noted that Neuman’s use of the term entropy differs somewhat from the strict scientific definition, which assumes a closed system, some scholars have critiqued this, but within the model, entropy denotes the process of breaking down toward illness or death, and negentropy denotes the process of growing or healing toward wellness.)
Reconstitution
If sufficient interventions and energy are available to the client system, it will eventually return to a state of reconstitution. Reconstitution is the process and outcome of the system returning to stability after a stressor has been removed. After effective treatment or intervention, the system may be restored to its standard line of defense, or it might establish a new, adjusted level of stability that could be at, above, or below the previous normal line. Recent nursing scholarship has further clarified that reconstitution should be understood as both a process (the journey of recovery) and an outcome (the achieved level of stability) following an encounter with stressors. In other words, reconstitution encompasses both the active recovery trajectory of the client system and the ultimate outcome of that recovery. The client’s health after reconstitution may even improve (to a higher wellness level) if growth occurs, or deteriorate if damage persists.
Strengths and Weaknesses
Betty Neuman originally designed her model specifically for nursing, but she acknowledged that other health disciplines could also utilize it. This broad applicability is both a strength and a potential weakness.
Strengths
- Versatility. The Neuman Systems Model is highly flexible and can be applied in all areas of nursing, from bedside clinical practice to nursing administration and education. Its concepts are broad enough to guide nursing care in various settings and with various populations.
- Holistic View. Neuman provides a truly holistic view of the client, one that is equally applicable whether the “client” is one person, a family, a community, or another aggregate. This encourages nurses to think beyond the individual and consider larger systems when appropriate.
- Logical Structure. The model, often depicted in a diagram of concentric circles and lines, is logically consistent in illustrating how different components (lines of defense, stressors, etc.) relate to one another. Once the framework is understood, it offers a clear mental map for assessing and planning care.
- Preventive Focus. Neuman’s emphasis on primary prevention (and health promotion) is a notable strength. It aligns with modern healthcare’s focus on preventive care and maintaining community health, rather than only treating illness after it occurs.
- Defined Components. Most of the model’s components have readily understandable definitions, which makes it relatively straightforward for nurses to learn and use after initial study. The concept of stressors, lines of defense, and other related ideas resonates with practical experiences in patient care.
Weaknesses
- Need for Clarity. A major noted weakness of the model has been the need for further clarification of terms and concepts. Some aspects of the theory, such as the distinction between interpersonal and extrapersonal stressors or the nature of the “created environment,” are confusing or overlapping and require clear delineation.
- Not Nursing-Specific. Because the model is so broadly applicable (even to other disciplines), some critics argue it may not be specific enough to nursing. If other health professionals can use the model interchangeably, it might not highlight what is unique about nursing’s contribution (this is a philosophical debate about whether a nursing model should be exclusive to nursing or not).
- Abstract Level. Like many grand theories, the Neuman Systems Model is a fairly abstract concept. Beginner nurses or students might find it challenging to directly apply such a high-level model to day-to-day clinical problems without additional guidance or practice in translating concepts to actions.
- Defense Lines Complexity. The idea of three levels of defense (flexible line, normal line, lines of resistance) is conceptually useful, but in reality, an individual’s response to stress may not segregate neatly into “lines.” Some have found Neuman’s depiction somewhat complex or not clearly evidenced, arguing that people have myriad coping responses that don’t necessarily fit into layered levels. It can take experience to intuitively grasp how to assess “lines of defense” in a real patient.
- Entropy Concept Misalignment. As noted earlier, Neuman’s use of the term entropy (and negentropy) has been critiqued as inconsistent with the strict scientific definition (which applies to closed systems). While this is a technical point, it constitutes a weakness in that it can confuse those who notice the discrepancy. The model’s intent is clear, describing trends toward illness or wellness, but the terminology could be improved for accuracy.
Analysis of the Neuman Systems Model
The Neuman Systems Model has been analyzed and used for many decades, and over time, both supporters and critics have weighed in on it. In evaluating the model.
The three types of defense lines Neuman describes (flexible, normal, resistance) were innovative, but some analysts feel these were not clearly explained in terms of how they operate in reality. Essentially, people resist stress with a variety of reactions (physiological reflexes, coping behaviors, etc.), and Neuman’s layered concept is one way to organize those, though it may over-complicate what could be seen as a continuum of responses.
Neuman’s inclusion of various energy resources in the basic structure opened up ideas for interventions (e.g., how can we boost a patient’s energy or coping reserves?). However, Neuman did not list specific “energies” exhaustively, which leaves the concept somewhat open-ended. Subsequent theorists have suggested identifying particular energy sources (such as immune strength, spiritual well-being, and social support) to make the model more actionable.
The model’s holistic view is very consonant with nursing’s values, treating health and illness as a continuum and acknowledging the interplay of multiple factors. This holistic emphasis remains a strong point, aligning with modern integrative healthcare approaches. Neuman’s idea that movement toward health is negentropic (building energy and organization) and toward illness is entropic is a creative way to frame the wellness-illness continuum. While, as mentioned, the terminology can be scientifically debated, the practical notion that illness drains energy and health is built by energy input is easy to grasp. It has intuitive appeal in nursing care planning.
Recent Developments
In the years since Neuman introduced her model, nursing scholars have continued to expand upon and clarify its concepts. Recognizing the earlier criticisms about vague or overlapping terms, contemporary nursologists have published updated analyses of key concepts.
For instance, the idea of stressors has been revisited to provide a more nuanced definition, emphasizing the client’s perception of stressors as positive or negative, and how that perception guides the choice of interventions.
Likewise, the concept of reconstitution (the recovery after stress) has been examined in depth, highlighting that it should be understood both as a process the client undergoes and as an outcome state of stability. These scholarly efforts have helped refine the theoretical definitions and enhance the model’s clarity for practitioners.
Despite any weaknesses, the Neuman Systems Model remains highly influential and continues to be applied in modern nursing practice and research. Its enduring relevance is demonstrated by the breadth of current applications and interpretations.
Neuman Systems Model and Schizophrenia
In mental health and caregiving, for example, Neuman’s model has been used to understand how severe illnesses affect not only patients but also their family caregivers. A 2017 study applied the Neuman Systems Model to the experience of caregivers of people with schizophrenia, illustrating how the model provides a comprehensive view of caregiver stress and can guide interventions to empower those caregivers in coping with their situation.
Application of NSM in COVID-19
During the global COVID-19 pandemic, nurses turned to Neuman’s framework to handle new challenges. Case studies have shown that the Neuman Systems Model can effectively guide nursing care for patients with COVID-19 by systematically addressing intrapersonal, interpersonal, and extrapersonal stressors associated with the illness, and by planning interventions at all prevention levels (from infection control education to acute care and rehabilitation). One such case report concluded that NSM is a valuable framework for delivering high-quality nursing care to patients with COVID-19.
NSM for Nurse Resilience
The model’s focus on stress and prevention has also been applied to the well-being of nurses themselves. In the face of high workplace stress and burnout rates in healthcare, NSM has been proposed as a conceptual foundation for building nurse resilience. Because the model focuses on identifying and mitigating stressors, it provides a framework for structuring resilience-building strategies for nurses. For instance, researchers have used Neuman’s model to explore and promote coping mechanisms that help nurses maintain their stability (wellness) amid occupational stress. By treating the nurse as the “client system,” interventions can be designed to strengthen nurses’ flexible lines of defense (like social support and self-care practices) and reinforce lines of resistance (like coping skills) against job-related stressors.
Summary
In summary, Betty Neuman’s Systems Model has stood the test of time as a valuable nursing theory. It has evolved through scholarly refinement but remains grounded in the core idea of holistic client care and proactive prevention of stress-related problems. Neuman’s legacy continues through ongoing research, international Neuman Systems Model symposia, and the countless nurses and students who use her model to inform and improve their practice. Her work has not only provided a unifying language for discussing patient care in terms of systems and stressors but has also inspired generations of nurses to approach patient care with an eye toward all the factors influencing health. The Neuman Systems Model, with its comprehensive approach to wellness, continues to guide nursing actions in our modern, complex healthcare environment, honoring Dr. Neuman’s vision of keeping clients as stable and healthy as possible in the face of life’s many stressors.
Recommended Resources
Recommended books and resources to learn more about nursing theory:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
- Nursing Theorists and Their Work (10th Edition) by Alligood
Nursing Theorists and Their Work, 10th Edition provides a clear, in-depth look at nursing theories of historical and international significance. Each chapter presents a key nursing theory or philosophy, showing how systematic theoretical evidence can enhance decision making, professionalism, and quality of care. - Knowledge Development in Nursing: Theory and Process (11th Edition)
Use the five patterns of knowing to help you develop sound clinical judgment. This edition reflects the latest thinking in nursing knowledge development and adds emphasis to real-world application. The content in this edition aligns with the new 2021 AACN Essentials for Nursing Education. - Nursing Knowledge and Theory Innovation, Second Edition: Advancing the Science of Practice (2nd Edition)
This text for graduate-level nursing students focuses on the science and philosophy of nursing knowledge development. It is distinguished by its focus on practical applications of theory for scholarly, evidence-based approaches. The second edition features important updates and a reorganization of information to better highlight the roles of theory and major philosophical perspectives. - Nursing Theories and Nursing Practice (5th Edition)
The only nursing research and theory book with primary works by the original theorists. Explore the historical and contemporary theories that are the foundation of nursing practice today. The 5th Edition, continues to meet the needs of today’s students with an expanded focus on the middle range theories and practice models. - Strategies for Theory Construction in Nursing (6th Edition)
The clearest, most useful introduction to theory development methods. Reflecting vast changes in nursing practice, it covers advances both in theory development and in strategies for concept, statement, and theory development. It also builds further connections between nursing theory and evidence-based practice. - Middle Range Theory for Nursing (4th Edition)
This nursing book’s ability to break down complex ideas is part of what made this book a three-time recipient of the AJN Book of the Year award. This edition includes five completely new chapters of content essential for nursing books. New exemplars linking middle range theory to advanced nursing practice make it even more useful and expand the content to make it better. - Nursing Research: Methods and Critical Appraisal for Evidence-Based Practice
This book offers balanced coverage of both qualitative and quantitative research methodologies. This edition features new content on trending topics, including the Next-Generation NCLEX® Exam (NGN). - Nursing Research (11th Edition)
AJN award-winning authors Denise Polit and Cheryl Beck detail the latest methodologic innovations in nursing, medicine, and the social sciences. The updated 11th Edition adds two new chapters designed to help students ensure the accuracy and effectiveness of research methods. Extensively revised content throughout strengthens students’ ability to locate and rank clinical evidence.
See Also
Recommended site resources related to nursing theory:
- Nursing Theories and Theorists: The Definitive Guide for Nurses MUST READ!
In this guide for nursing theories, we aim to help you understand what comprises a nursing theory and its importance, purpose, history, types or classifications, and give you an overview through summaries of selected nursing theories.
Other resources related to nursing theory:
- Betty Neuman: Neuman Systems Model
- Dorothea Orem: Self-Care Deficit Theory
- Dorothy Johnson: Behavioral System Model
- Faye Abdellah: 21 Nursing Problems Theory
- Florence Nightingale: Environmental Theory
- Hildegard Peplau: Interpersonal Relations Theory
- Ida Jean Orlando: Deliberative Nursing Process Theory
- Imogene King: Theory of Goal Attainment
- Jean Watson: Theory of Human Caring
- Lydia Hall: Care, Cure, Core Nursing Theory
- Madeleine Leininger: Transcultural Nursing Theory
- Martha Rogers: Science of Unitary Human Beings
- Myra Estrin Levine: The Conservation Model of Nursing
- Nola Pender: Health Promotion Model
- Sister Callista Roy: Adaptation Model of Nursing
- Virginia Henderson: Nursing Need Theory
References
Recommended resources and references for this nursing theories guide.
- Alligood, M. R. (2013). Nursing Theory-E-Book: Utilization & Application. Elsevier Health Sciences.
- Neuman, B. (1996). The Neuman systems model in research and practice. Nursing Science Quarterly, 9(2), 67-70. [Link]
- Neuman, B. (1995). The Neuman systems model (3rd ed.). In McEwen, M. and Wills, E. (Ed.). Theoretical basis for nursing. USA: Lippincott Williams & Wilkins.
- Neuman, B. (various editions); Fawcett, J., & DeSanto-Madeya, S. (2013); Turney & Kaylor (2015); Provencher, H. et al. (2025); and other contemporary nursing literature and case studies as cited above.
External Links
- NeumanSystemsMode.org. Official webpage of Betty Neuman.
Biography was written by Wayne, G., Updated by Martin, P.


















Leave a Comment