My grandfather has turned 89 years old 2 months ago. He seems to have changed from then on. He always complains of seeing ants in the ceiling, or ants on the floor beside his bed. He sometimes forgets my name. Lately, he keeps on mumbling to himself and looks agitated. He doesn’t know where he is anymore, or what the present date is. I’m really worried that he is in the early stages of delirium. I think we should have him checked.
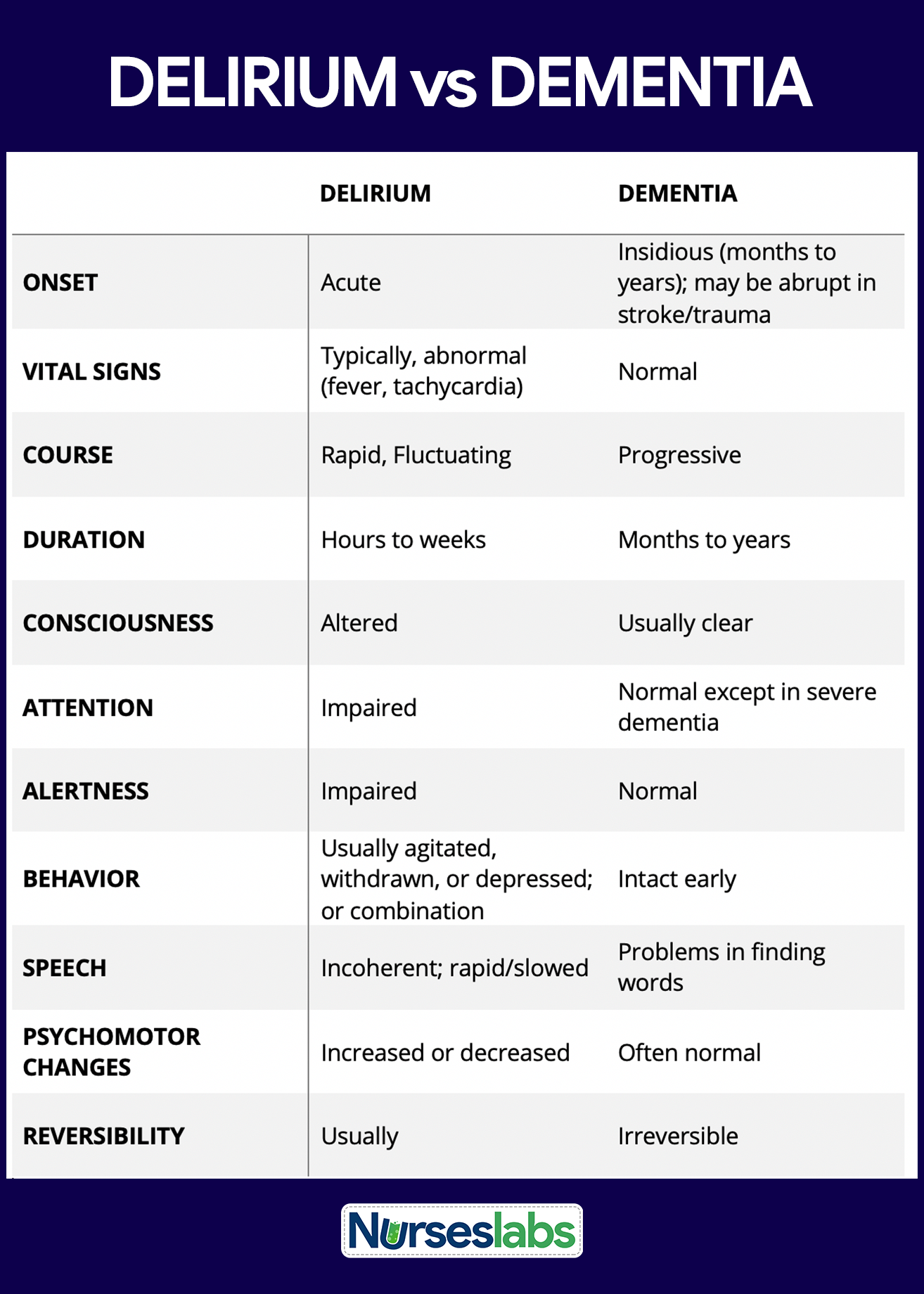
Delirium is an acute neuropsychiatric syndrome characterized by rapid-onset confusion, altered consciousness, and impaired cognitive function. It often results from underlying medical conditions, substance use, or medication effects.
This nursing guide provides a concise overview of delirium and its significance in psychiatric nursing practice.
What is Delirium?
Delirium is a disturbance of consciousness and a change in cognition that develop rapidly over a short period (DSM-IV-TR).
- Delirium is an acute and reversible condition that often occurs as a result of an underlying medical condition, substance intoxication or withdrawal, or medication side effects.
Statistics and Incidences
Delirium is common in the United States.
- In a systematic review of 42 cohorts in 40 studies, 10-31% of new hospital admissions met the criteria for delirium and the incidence of developing delirium during the admission ranged from 3-29%.
- For patients in intensive care units, the prevalence of delirium may reach as high as 80%.
- Prevalence of postoperative delirium following general surgery is 5-10% and as high as 42% following orthopedic surgery.
- As many as 80% of patients develop delirium death.
- Delirium can occur at any age, but it occurs more commonly in patients who are elderly and have compromised mental status.
- In patients who are admitted with delirium, mortality rates are 10-26%.
- Patients who develop delirium during hospitalization have a mortality rate of 22-76% and a high rate of death during the months following discharge.
Causes
The DSM-IV-TR differentiates among the disorders of delirium by their etiology, although they share a common symptom presentation. Categories of delirium include the following:
- Delirium due to a general medical condition. Certain medical conditions, such as systemic infections, metabolic disorders, fluid and electrolyte imbalances, liver or kidney disease, thiamine deficiency, postoperative states, hypertensive encephalopathy, postictal states, and sequelae of head trauma, can cause symptoms of delirium.
- Substance-induced delirium. The symptoms of delirium can be induced by exposure to a toxin or the ingestion of medications, such as anticonvulsants, neuroleptics, anxiolytics, antidepressants, cardiovascular medications, antineoplastics, analgesics, antiasthmatic agents, antihistamines, antiparkinsonian drugs, corticosteroids, and gastrointestinal medications.
- Substance-intoxication delirium. Delirium symptoms can occur in response to taking high doses of cannabis, cocaine, hallucinogens, alcohol, anxiolytics, or narcotics.
- Substance-withdrawal delirium. Reduction or termination of long-term, high dose, use of certain substances, such as alcohol, sedatives, hypnotics, or anxiolytics, can result in withdrawal delirium symptoms.
- Delirium due to multiple etiologies. Symptoms of delirium may be related to more than one general medical condition or to the combined effects of a general medical condition and substance use.
Clinical Manifestations
The following symptoms have been identified with the syndrome of delirium:
- Altered consciousness ranging from hypervigilance to stupor or semicoma.
- Extreme distractibility with difficulty focusing attention.
- Disorientation to time and place.
- Impaired reasoning ability and goal-directed behavior.
- Disturbance in the sleep-wake cycle.
- Emotional instability as manifested by fear, anxiety, depression, irritability, anger, euphoria, or apathy.
- Misperceptions of the environment, including illusions and hallucinations.
- Automatic manifestations, such as tachycardia, sweating, flushed face, dilated pupils, and elevated blood pressure.
- Incoherent speech.
- Impairment of recent memory.
Assessment and Diagnostic Findings
Laboratory tests that may be helpful for diagnosis include the following:
- Complete blood cell count with differential. Helpful to diagnose infection and anemia.
- Electrolytes. To diagnose low or high levels.
- Glucose. To diagnose hypoglycemia, diabetic ketoacidosis, and hyperosmolar nonketotic states.
- Renal and liver function tests. To diagnose renal and liver failure.
- Thyroid function studies. To diagnose hypothyroidism.
- Urine analysis. Used to diagnose urinary tract infection.
- Urine and blood drug screen. Used to diagnose toxicological causes.
- Thiamine and vitamin B12 levels. Used to detect deficiency states of these vitamins.
- Serum marker for delirium. The calcium-binding protein S-100 B could be a serum marker for delirium. Higher levels are seen in patients with delirium when compared to patients without delirium.
Medical Management
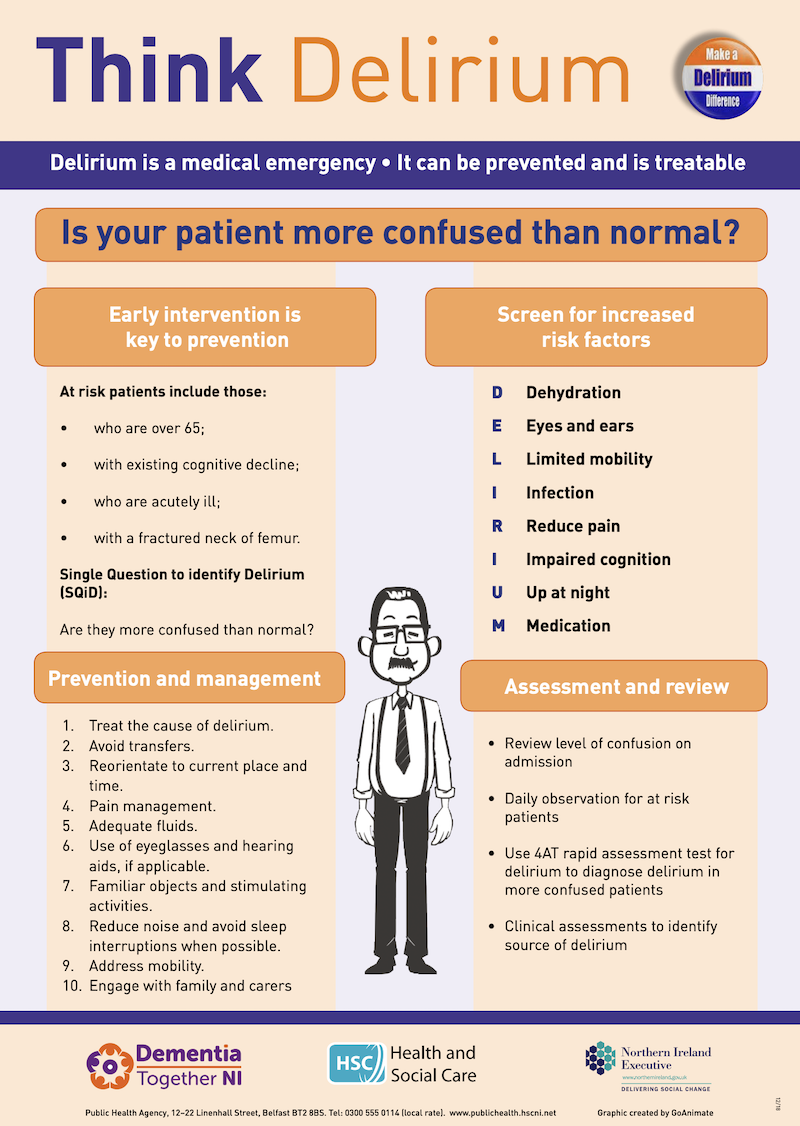
When delirium is diagnosed or suspected, the underlying causes should be sought and treated.
- Fluid and nutrition. Fluid and nutrition should be given carefully because the patient may be unwilling or physically unable to maintain a balanced intake; for the patient suspected of having alcohol toxicity or alcohol withdrawal, therapy should include multivitamins, especially thiamine.
- Reorientation techniques. Reorientation techniques or memory cues such as a calendar, clicks, and family photos may be helpful.
- Supportive therapy. The environment should be stable, quiet, and well-lighted; sensory deficits should be corrected, if necessary, with eyeglasses or hearing aids; family members and staff should explain proceedings at every opportunity, reinforce orientation, and reassure the patient.
Pharmacologic Management
Delirium that causes injury to the patient or others should be treated with medications.
- Antipsychotics. This class of drugs is the medication of choice in the treatment of psychotic symptoms of delirium.
- Benzodiazepines. Reserved for delirium resulting from seizures or withdrawal from alcohol or sedative hypnotics.
- Vitamins. Patients with alcoholism and patients with malnutrition are prone to thiamine and vitamin B12 deficiency, which can cause delirium.
- Hypnotic, miscellaneous. Agents in this class may be useful in the prevention and management of delirium (e.g. melatonin, ramelteon).
Nursing Management
Nursing management for a patient with delirium includes the following:
Nursing Assessment
Nursing assessment should include:
- Psychiatric interview. The psychiatric interview must contain a description of the client’s mental status with a thorough description of behavior, the flow of thought and speech, affect, thought processes and mental content, sensorium and intellectual resources, cognitive status, insight, and judgment.
- Serial assessment. Serial assessment of psychiatric status is necessary for determining the fluctuating course and acute changes in mental status.
Nursing Diagnosis
Sample nursing diagnoses for persons with delirium include:
- Disturbed thought processes related to delusional thinking.
- Chronic Confusion related to cognitive impairment.
- Impaired verbal communication related to cognitive impairment.
- Risk for injury related to suicidal ideations, illusions, and hallucinations.
- Impaired memory related to cognitive impairment.
- Risk for other-directed violence related to suspiciousness of others.
Nursing Care Planning and Goals
The major nursing care plan goals for delirium are:
- Client will maintain agitation at a manageable level so as not to become violent.
- Client will not harm self or others.
Nursing Interventions
Nursing interventions for patients with delirium include the following:
- Assess the level of anxiety. Assess the client’s level of anxiety and behaviors that indicate the anxiety is increasing; recognizing these behaviors, the nurse may be able to intervene before violence occurs.
- Provide an appropriate environment. Maintain a low level of stimuli in the client’s environment (low lighting, few people, simple decor, low noise level) because anxiety increases in a highly stimulating environment.
- Promote patient safety. Remove all potentially dangerous objects from the client’s environment; in a disoriented, confused state, clients may use objects to harm self or others.
- Ask for assistance from others when needed. Have sufficient staff available to execute a physical confrontation, if necessary; assistance may be required from others to provide for the physical safety of the client or primary nurse, or both.
- Stay calm and reassure the patient. Maintain a calm manner with the client; attempt to prevent frightening the client unnecessarily; Provide continual reassurance and support.
- Interrupt periods of unreality and reorient. Client safety is jeopardized during periods of disorientation; correcting misinterpretations of reality enhances the client’s feelings of self-worth and personal dignity.
- Medicate or restrain patient as prescribed. Use tranquilizing medications and soft restraints, as prescribed by physician, for protection of client and other during periods of elevated anxiety.
- Observe suicide precautions. Sit with the client and provide one-to-one observation if assessed to be actively suicidal; client safety is a nursing priority, and one-to-one observation may be necessary to prevent a suicidal attempt.
- Teach relaxation exercises to intervene in times of increasing anxiety.
- Teach prospective caregivers to recognize client behaviors that indicate anxiety is increasing and ways to intervene before violence occurs.
Evaluation
The outcome criteria include:
- Prospective caregivers are able to verbalize behaviors that indicate an increasing anxiety level and ways they may assist clients to manage their anxiety before violence occurs.
- With assistance from caregivers, the client is able to control the impulse to perform acts of violence against self or others.
Documentation Guidelines
Documentation in a patient with delirium includes:
- Individual findings include factors affecting, interactions, the nature of social exchanges, and specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
References
Sources and references for this study guide for delirium:
- Black, J. M., & Hawks, J. H. (2005). Medical-surgical nursing. Elsevier Saunders,.
- Videbeck, S. L. (2010). Psychiatric-mental health nursing. Lippincott Williams & Wilkins.
















Leave a Comment