Imperforate anus is a congenital abnormality that occurs when the opening of the anus is either absent or improperly formed in newborns. This condition can range from a partial obstruction to a complete absence of the anal opening, leading to difficulties in passing stool.
Imperforate anus requires prompt recognition and appropriate nursing care, as it can significantly impact the newborn‘s health and require surgical intervention.
What is Imperforate Anus?
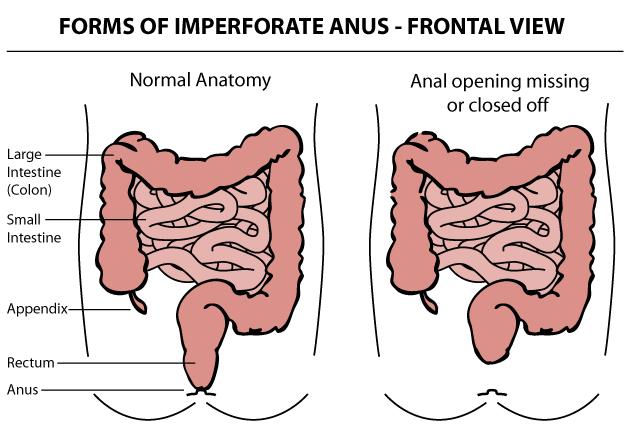
- When a malformation of the anus is present, the muscles and nerves associated with the anus often have a similar degree of malformation.
- The position and nature of these malformations made repair difficult for early surgeons; the affected organs are located deep in the pelvis and are not well visualized through abdominal incisions.
Pathophysiology
The embryogenesis of these malformations remains unclear.
- The rectum and anus are believed to develop from the dorsal portion of the hindgut or cloacal cavity when lateral ingrowth of the mesenchyme forms the urorectal septum in the midline.
- This septum separates the rectum and anal canal dorsally from the bladder and urethra; the cloacal duct is a small communication between the 2 portions of the hindgut.
- Downgrowth of the urorectal septum is believed to close this duct by 7 weeks’ gestation; during this time, the ventral urogenital portion acquires an external opening; the dorsal anal membrane opens later.
- The anus develops by a fusion of the anal tubercles and an external invagination, known as the proctodeum, which deepens toward the rectum but is separated from it by the anal membrane; this separating membrane should disintegrate at 8 weeks’ gestation.
- Interference with anorectal structure development at varying stages leads to various anomalies, ranging from anal stenosis, incomplete rupture of the anal membrane, or anal agenesis to complete failure of the upper portion of the cloaca to descend and failure of the proctodeum to invaginate.
Statistics and Incidences
Anorectal malformations occur in approximately 1 newborn per 5000 live births.
- Anorectal and urogenital malformations are rarely fatal, although some associated anomalies (cardiac, renal) can be life-threatening.
- Intestinal perforation or postoperative septic complications in a newborn with imperforate anus can result in mortality or severe morbidity.
- Malformation-related morbidity relates to associated malformations of rectal motility, anorectal innervation, and sphincteric musculature; the most common morbidity in this category is constipation; most children have mild malformations that commonly result in constipation for reasons that remain unclear.
- The most severe forms of malformation-associated morbidity are fecal and urinary incontinence.
- No known racial predilection has been reported.
- No known sex predilection has been reported.
- Most children with an anorectal malformation are identified upon routine newborn physical examination.
Clinical Manifestations
Newborns with imperforate anus are usually identified upon the first physical examination.
- Absence of stool. There is no passage of stool within a day or two of birth.
- Passing of stools in other openings. The infant may pass stools through another opening like the urethra in boys or vagina in girls.
- Swollen belly. The newborn could not pass out stools, resulting in a swollen belly.
- Absence of anal opening. The opening of the anus is missing or not in its usual place; in girls, this may be near the vagina.
Assessment and Diagnostic Findings
In the diagnosing imperforate anus the following are suggested:

- Laboratory studies. CBC count, blood typing and screening, and serum electrolyte levels should be measured in all children with imperforate anus who require operation; urinalysis should be performed to determine the presence of a rectourinary fistula in all cases in which the diagnosis cannot be made based solely on the physical examination findings.
- Sacral radiography. Two views of the sacrum, posteroanterior and lateral, should be obtained to measure sacral ratios and to look for sacral defects, hemivertebrae, and presacral masses; this should be performed before surgery.
- Abdominal ultrasonography. This study is specifically used to examine the genitourinary tract and to look for any other masses; hydronephrosis, hydrocolpos, presacral mass, abdominal mass, or any similar finding can profoundly affect management.
- Spinal ultrasonography or MRI. All children with any form of anorectal malformation, even those considered minor, should undergo screening for spinal malformations; these lesions can be diagnosed using ultrasonography prior to the ossification of the spine.
- Lateral pelvic radiography at 24 hours. Children who could not be diagnosed based solely on physical examination findings traditionally underwent invertography, which consisted of holding the baby upside down and using lateral radiography to observe the level of gas in the distal rectum; a similar, but more humane, approach is to wait 24 hours after birth to observe for possible maximal pelvic pouch distension and then to use cross-table lateral pelvic radiography with a radio-opaque marker on the anal dimple with the child in the prone position and the hips slightly raised.
- MRI. All children who have sacral defects on plain radiographs should undergo spine ultrasonography to rule out associated malformations, such as meningocele or meningomyelocele, teratoma, or mixed lesions.
- CT scanning. CT scanning presently plays no role in the routine evaluation of children with anorectal malformations.
Medical Management
Management of an infant with an imperforate anus includes:
- Nothing per orem. Newborns with imperforate anus should not be fed and should receive intravenous hydration.
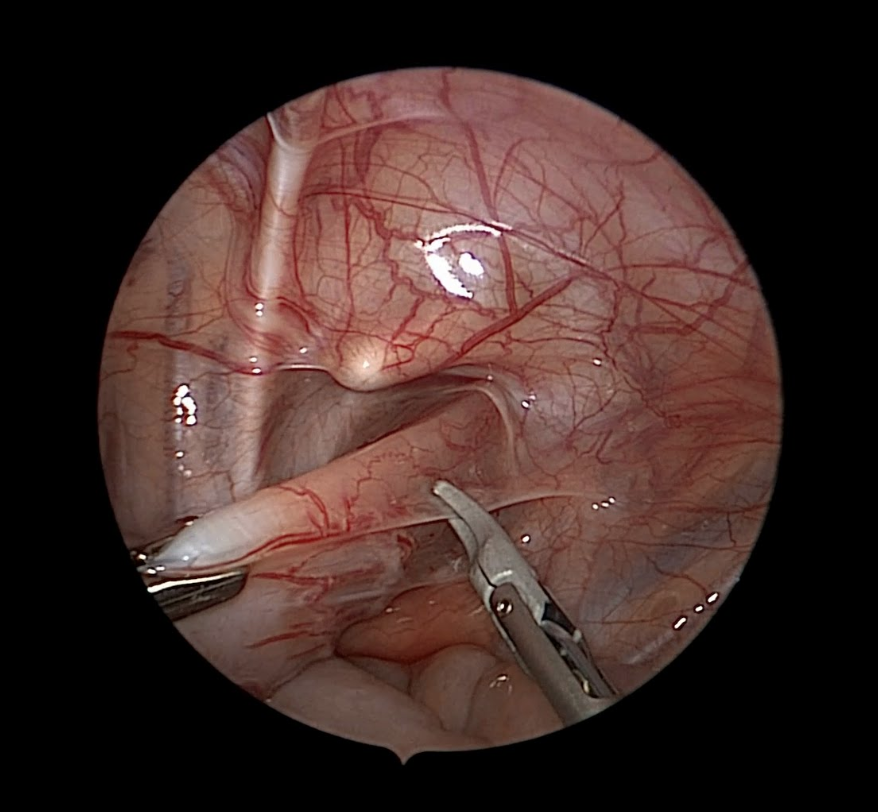
- Neonatal colostomy. A colostomy is performed in children who are not amenable to primary pull-through either because of malformation complexity (any urinary fistula in boys, vestibular fistula, and cloaca in girls, no fistula in either sex >1 cm from perineal skin) or associated comorbidity.
- Primary neonatal pull-through without colostomy. Many pediatric surgeons opt for primary pull-through in children with perineal fistulas (or no fistulas) and close (< 1 cm) rectal pouches on 24-hour lateral pelvic radiography.
- Posterior sagittal pull-through with a colostomy. This approach is used in boys with rectourinary fistula (bulbar, prostatic, or bladder-neck fistula), in girls with cloaca or vestibular fistula, and in patients of either sex who do not have a fistula when the rectal pouch is further than 1 cm on 24-hour lateral prone abdominal radiography.
- Colostomy closure. Once the wound has completely healed and postoperative dilations have achieved their goal (i.e., the neoanus is at the desired size), the colostomy may be closed in traditional surgical fashion.
- Diet. After the obstruction is relieved using colostomy, primary pull-through, or dilation, children do not require special diet; children should avoid constipating foods, such as those included in the bananas, rice, applesauce, and toast (BRAT) diet. High-fiber and laxative foods (whole-grain foods and bread, dairy, fruits, vegetables, greasy foods, spicy foods) should be encouraged.
- Activity. Children with anorectal malformations are often otherwise healthy; activity limitations are usually related only to the period around their surgical procedures.
Pharmacologic Management
Many children with anorectal malformations require medications for various reasons.
- Antibiotic prophylaxis. Urinary prophylaxis is used to mitigate the risk of urinary infection and urosepsis in children with risk factors for urinary infection such as urinary fistula, vesicoureteral reflux, or continent diversion.
- Laxatives. Common laxatives include senna products, milk of magnesia, and propylene glycol solutions (eg, MiraLax, GlycoLax).
Nursing Management
Nursing care for an infant with an imperforate anus includes:
Nursing Assessment
Assessment of an infant with an imperforate anus includes the following:
- History. Prenatal ultrasonography examination findings are often normal, although the polyhydramnios or intraabdominal cysts may suggest an imperforate anus with associated hydrocolpos or hydronephrosis.
- Physical exam. Newborns with imperforate anus are usually identified upon the first physical examination; malformations in newborns that are missed upon initial examination are often discovered within 24 hours when the newborn is observed to have distention and has failed to pass meconium and a more thorough examination is performed.
Nursing Diagnoses
Based on the assessment data the major nursing diagnoses are:
- Fluid volume deficit related to excessive loss through vomiting.
- Impaired skin integrity related to the colostomy.
- Risk for infection related to surgical procedures.
Nursing Care Planning and Goals
The major nursing care planning goals for patients with imperforate anus:
- Maintaining adequate hydration with moist mucous membranes, good skin turgor, and adequate capillary refill.
- Maintaining stable vital signs.
- Achieving adequate output of urine.
- Achieving dry and damage-free skin around the colostomy.
- Absence of infection.
Nursing Interventions
Nursing interventions for a child with imperforate anus are:
- Avoid infection. Teach the caregivers to keep the area around the colostomy clean with soap and water and to diaper the baby in the usual way; monitor white blood cell (WBC) count; and wash hands and teach patient and SO to wash hands before contact with patients and between procedures with the patient.
- Protect skin integrity. A protective ointment is useful to protect the skin around the colostomy; monitor site of impaired tissue integrity at least once daily for color changes, redness, swelling, warmth, pain, or other signs of infection; and keep a sterile dressing technique during wound care.
- Restore balanced fluid volume. Administer parenteral fluids as prescribed; consider the need for an IV fluid challenge with an immediate infusion of fluids for patients with abnormal vital signs; teach family members how to monitor output in the home; instruct them to monitor both intake and output.
Evaluation
Goals are met as evidenced by:
- Maintained adequate hydration with moist mucous membranes, skin turgor and capillary refill good.
- Maintained stable vital signs.
- Achieved adequate output of urine.
- Achieved dry and damage-free skin around the colostomy.
- Absence of infection.
Documentation Guidelines
Documentation in a patient with an imperforate anus includes the following:
- Individual findings include factors affecting, interactions, the nature of social exchanges, and specifics of individual behavior.
- Intake and output.
- Signs of infection.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.


























Leave a Comment