Some complications of pregnancy only develop during the instance that the woman is pregnant, while others have already been there even before the pregnancy has started. These complications are just roadblocks towards a healthy pregnancy, and we are the drivers who should carry our passengers, our patients, to safety by avoiding these roadblocks. Pregnancy-induced hypertension (PIH), also known as gestational hypertension or pregnancy-related high blood pressure, is one such condition that demands careful monitoring and expert nursing care.
This article aims to provide nursing professionals with a comprehensive guide to understanding, identifying, and managing pregnancy-induced hypertension. By delving into the pathophysiology, risk factors, and clinical manifestations of PIH, we seek to equip nurses with the knowledge and skills necessary to provide optimal care for mothers facing this challenge.
What is Pregnancy Induced Hypertension?
- Pregnancy induced hypertension (PIH) is a condition wherein vasospasm occurs during pregnancy in both the small and large arteries in the body.
- Also known as gestational hypertension.
- Pregnancy Induced Hypertension is a form of high blood pressure in pregnancy.
- It occurs in about 5 percent to 8 percent of all pregnancies.
- It is a condition in which vasospasm occurs during pregnancy in both small and large arteries. With high blood pressure, there is an increase in the resistance of blood vessels. This may hinder blood flow in many different organ systems in the expectant mother including the liver, kidneys, brain, uterus, and placenta.
- Originally, it was called toxaemia because researchers pictured a toxin of some kind being produced by the woman in response to the foreign protein of the growing fetus, the toxin leading to the typical symptoms. No such toxin has ever been identified.
Pathophysiology
- Increased cardiac output occurs with pregnancy, and it can injure the epithelial cell of the arteries.
- Prostaglandin, a vasodilator, may also contribute to the injury.
- Reduced responsiveness of the blood vessels to the blood pressure is lost.
- There is vasoconstriction, and blood pressure increases.
Classifications
Gestational Hypertension
- A woman is said to have Gestational Hypertension when she develops an elevated blood pressure (140/90 mmHg) but has no proteinuria or edema.
- Perinatal mortality is not increased with simple gestational hypertension, so no drug therapy is necessary.
- Systolic blood pressure greater than 30 mmHg and diastolic blood pressure greater than 15 mmHg above pregnancy values.
- No edema, no proteinuria and blood pressure returns to normal after birth.
Mild Preeclampsia
- A woman is said to be mildly preeclamptic when her blood pressure rises to 140/90 mmHg, taken on two occasions at least six (6) hours apart.
- Systolic blood pressure greater than 30 mmHg and diastolic blood pressure greater than 15 mmHg above pregnancy values.
- In addition to hypertension, a woman has proteinuria (1+ or 2+ on a reagent test strip on a random sample).
- A weight gain of more than 2 lbs/week in the second trimester or 1 lb/week in the third trimester usually indicates abnormal tissue fluid retention.
Severe Preeclampsia
- A woman has passed from mild to severe preeclampsia when her blood pressure has risen to 160 mmHg systolic and 110 mmHg diastolic or above on at least two occasions 6 hours apart at bed rest.
- Marked proteinuria. 3+ or 4+ on a random urine sample or more than 5 g in a 24-hour sample and extensive edema are also present.
- With the severe preeclampsia, the extreme edema will be noticeable as puffiness in a woman’s face and hands.
- It is most readily palpated over bony surfaces. The woman may manifest oliguria (altered renal function), elevated serum creatinine (more than 1.2 mg/dL); cerebral or visual disturbances (blurred vision); thrombocytopenia and epigastric pain.
Eclampsia
This is the most severe classification of PIH. A woman has passed into this stage when cerebral edema is so acute that seizure or coma occurs. With eclampsia, the maternal mortality is high from cause such as cerebral hemorrhage, circulatory collapse or renal failure. The fetal prognosis in eclampsia is poor because of hypoxia and consequent fetal acidosis. The manifestations are the same accompanied by seizures.
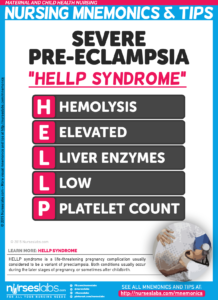
HELLP Syndrome
HELLP syndrome is a complication of severe preeclampsia or eclampsia. HELLP syndrome is a group of physical changes including the breakdown of red blood cells, changes in the liver and low platelets (cells found in the blood that are needed to help the blood to clot in order to control bleeding).
Risk Factors
There are certain factors that contribute to the occurrence of pregnancy induced hypertension.
- Women of color. Hypertension is most common to these women due to genetic makeup of their race.
- Multiple pregnancies. Women who have undergone multiple pregnancies are more compromised with hypertension.
- Primiparas who are 20 years and older. This group has an increased risk for pregnancy induced hypertension than women who are 40 years old and above.
- Women from low socioeconomic backgrounds. These women may have a poor diet due to their low socioeconomic background, which could contribute greatly to hypertension.
- Underlying disease. This disease might contribute to the occurrence of pregnancy induced hypertension.
Signs and Symptoms
These signs and symptoms, once detected, would indicate pregnancy induced hypertension
- Hypertension. An increase in the usual blood pressure of the woman is the first indicator of this disease.
- Proteinuria. Protein leaks out during this condition and can be detected in the urine.
- Edema. Since protein has already leaked out and it is responsible for containing water inside the vessels, edema starts to occur.
Diagnostic Tests
Diagnostic tests would be ordered by the physician to determine the presence of pregnancy induced hypertension.
- Urinalysis. This is one of the most common diagnostic tests that determine the presence of protein in the urine. This is usually indicative of pregnancy induced hypertension.
Medical Management
Medications and other therapies are instituted by the physician to reverse pregnancy induced hypertension.
- Antiplatelet therapy. There is an increased tendency for platelets to cluster along the vessel walls, so a mild antiplatelet agent is ordered by the physician.
- Administer medications to prevent eclampsia. To avoid progression of the disease to eclampsia, hydralazine, nifedipine, and labetalol may be prescribed to reduce hypertension.
Surgical Management
No surgical interventions are needed to manage pregnancy induced hypertension. They can be managed by medications and interventions imposed or ordered by health care providers.
Nursing Care Plan and Management
Nurses also have a role in reducing the blood pressure of the patient. These are just simple interventions but could create a dramatic effect when applied properly.
Please visit 7 Preeclampsia & Gestational Hypertensive Disorders Nursing Care Plans for a comprehensive nursing care plan and management guide.

















Leave a Comment