Nephrotic syndrome is a significant kidney disorder characterized by a combination of clinical features, including increased protein excretion in the urine (proteinuria), low levels of albumin in the blood (hypoalbuminemia), high levels of cholesterol and triglycerides, and edema (swelling) in various parts of the body. It is not a specific disease but rather a set of symptoms that can arise from different underlying kidney conditions, such as minimal change disease, focal segmental glomerulosclerosis, and membranous nephropathy, among others.
This article aims to provide a comprehensive overview of nephrotic syndrome, exploring its pathophysiology, causes, clinical manifestations, diagnostic evaluation, management strategies, and the critical role of nursing care in supporting individuals living with this complex kidney disorder.
What is Nephrotic Syndrome?
Nephrotic syndrome has a course of remissions and exacerbations that usually lasts for months.
- Nephrotic syndrome, or nephrosis, is defined by the presence of nephrotic-range proteinuria, edema, hyperlipidemia, and hypoalbuminemia.
- Nephrotic syndrome can affect individuals of all ages, but it is more commonly diagnosed in children, especially between the ages of 2 and 6 years.
- While nephrotic-range proteinuria in adults is characterized by protein excretion of 3.5 g or more per day, in children it is defined as protein excretion of more than 40 mg/m2/h or a first-morning urine protein/creatinine of 2-3 mg/mg creatinine or greater.
Pathophysiology
In a healthy individual, less than 0.1% of plasma albumin may traverse the glomerular filtration barrier. Amounts above 500 mg/day point to glomerular disease.
- The glomerular capillaries are lined by a fenestrated endothelium that sits on the glomerular basement membrane, which in turn is covered by glomerular epithelium, or podocytes, which envelops the capillaries with cellular extensions called foot processes.
- In between the foot processes are the filtration slits; these three structures—the fenestrated endothelium, glomerular basement membrane, and glomerular epithelium—are the glomerular filtration barrier.
- Filtration of plasma water and solutes is extracellular and occurs through the endothelial fenestrae and filtration slits.
- The importance of the podocytes and the filtration slits is shown by genetic diseases: in congenital nephrotic syndrome of the Finnish type, the gene for nephrin, a protein of the filtration slit, is mutated, leading to nephrotic syndrome in infancy; similarly, podocin, a protein of the podocytes, may be abnormal in a number of children with steroid-resistant focal glomerulosclerosis.
- The glomerular structural changes that may cause proteinuria are damage to the endothelial surface, the glomerular basement membrane, or the podocytes; one or more of these mechanisms may be seen in any one type of nephrotic syndrome.
- Albuminuria alone may occur or, with greater injury, leakage of all plasma proteins (ie, proteinuria) may take place.
- There are two current hypotheses for the formation of edema in nephrotic syndrome: the underfill hypothesis holds that the loss of albumin leading to lower plasma colloid pressure is the cause; the overfill hypothesis states that the edema is due to primary renal sodium retention.
Statistics and Incidences
Nephrotic syndrome is present in as many as 7 children per 100, 000 population younger than 9 years of age.
- The average age of onset is 2.5 years, with most cases occurring between the ages of 2 and 6 years.
- In the United States, the reported annual incidence rate of nephrotic syndrome is 2-7 cases per 100,000 children younger than 16 years.
- In children younger than 8 years at onset, the ratio of males to females varies from 2:1 to 3:2 in various studies.
- In children, nephrotic syndrome may occur at a rate of 20 cases per million children.
- Because diabetes is a major cause of nephrotic syndrome, American Indians, Hispanics, and African Americans have a higher incidence of nephrotic syndrome than white persons.
- There is a male predominance in the occurrence of nephrotic syndrome, as for chronic kidney disease in general.
Causes
There are two causes of nephrotic syndrome: primary and secondary.
- Primary. Common primary causes of nephrotic syndrome include kidney diseases such as minimal-change nephropathy, membranous nephropathy, and focal glomerulosclerosis.
- Secondary. Secondary causes include systemic diseases such as diabetes mellitus, lupus erythematosus, and amyloidosis.
Clinical Manifestations
The first sign of nephrotic syndrome in children is usually swelling of the face; this is followed by swelling of the entire body.
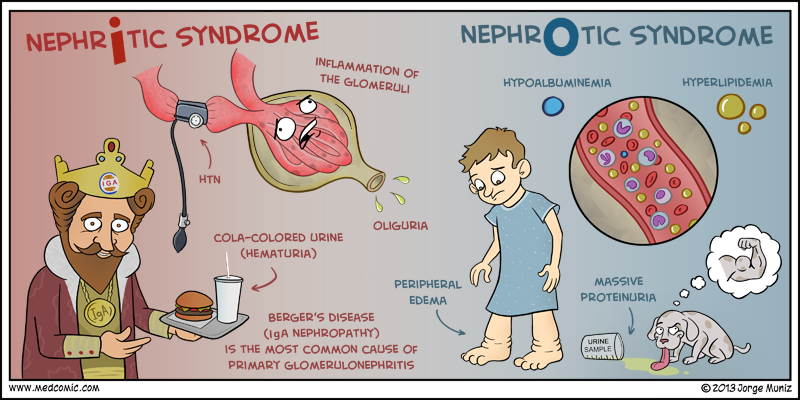
- Edema. Edema is the salient feature of nephrotic syndrome and initially develops around the eyes and legs; with time, the edema becomes generalized and may be associated with an increase in weight, the development of ascites, or pleural effusions.
- Malnutrition. Malnutrition may become severe, however, the generalized edema masks the loss of body tissue, causing the child to present a chubby appearance and to double his or her weight.
- Irritability and loss of appetite. Anorexia, irritability, and loss of appetite develop.
- Immunosuppression. These children are generally susceptible to infection, and repeated acute respiratory conditions are the usual pattern.
- Proteinuria. Albumin leaks out due to structural damage, leading to proteinuria.
- Respiratory tract infection. A history of a respiratory tract infection immediately preceding the onset of nephrotic syndrome is frequent.
- Allergy. Approximately 30% of children with nephrotic syndrome have a history of allergy.
Assessment and Diagnostic Findings
In order to establish the presence of nephrotic syndrome, laboratory tests should confirm (1) nephrotic-range proteinuria, (2) hypoalbuminemia, and (3) hyperlipidemia. Therefore, initial laboratory testing should include the following:
- Urine studies. First-morning urine protein/creatinine is more easily obtained than 24-hour urine studies, is possibly more reliable, and excludes orthostatic proteinuria; a urine protein/creatinine ratio of more than 2-3 mg/mg is consistent with nephrotic-range proteinuria.
- Blood studies. Serum albumin levels in nephrotic syndrome are generally less than 2.5 g/dL; serum sodium levels are low in patients with INS because of hyperlipidemia (pseudohyponatremia), as well as dilution due to water retention; on the CBC, an increased hemoglobin and hematocrit indicate hemoconcentration and intravascular volume depletion; the platelet count is often increased.
- Genetic testing. Patients with infantile or congenital nephrotic syndrome should have testing for mutations in NPHS1 and WT1; if test results are normal, then testing for mutations in NPHS2 and PLCE1 should be considered.
Medical Management
The management of nephrotic syndrome is a long process with remissions and recurrence of symptoms common.
- Corticosteroid therapy. The general consensus now is daily induction steroid treatment for 6 weeks, followed by alternate-day maintenance therapy for another 6 weeks.
- Diuretic therapy. Diuretic therapy may be beneficial, particularly in children with symptomatic edema; loop diuretics, such as furosemide (starting at 1-2 mg/kg/d) may improve edema; their administration, however, should be handled with care because plasma volume contraction may already be present, and hypovolemic shock has been observed with overly aggressive therapy.
- Home monitoring. Home monitoring of urine protein and fluid status is an important aspect of management; all patients and parents should be trained to monitor first morning urine proteins at home with urine dipstick; urine testing at home is also useful in monitoring response (or non-response) to steroid treatment.
- Diet. A sodium-restricted diet should be maintained while a patient is edematous and until proteinuria remits; during severe edema, careful and modest fluid restriction may be appropriate, but the patient must be monitored closely for excessive intravascular volume depletion.
- Activity. A normal activity plan is recommended.
Pharmacologic Management
Prednisone is the first-line therapy for children with nephrotic syndrome. Other immunosuppressive medications may be useful in those whose symptoms fail to respond to standard corticosteroid therapy or in those who have frequent relapses.
- Glucocorticoids. All glucocorticoids are effective; however, prednisone or prednisolone is used most commonly; their specific mode of action in nephrotic syndrome is unknown.
- Diuretics. Diuretics promote excretion of water and electrolytes by the kidneys; these agents are used to treat heart failure or hepatic, renal, or pulmonary disease when sodium and water retention has resulted in edema or ascites.
- Plasma protein. This agent is used to supplement diuresis in patients with edema; it increases oncotic pressure and thereby promotes a fluid shift from interstitial tissues.
- Immunosuppressive agents. This agent is used to supplement diuresis in patients with edema; it increases oncotic pressure and thereby promotes a fluid shift from interstitial tissues.
Nursing Management
The nursing management of a child with nephrotic syndrome include the following.
SEE ALSO: 6 Nephrotic Syndrome Nursing Care Plans for a comprehensive nursing care plan and management guide
Nursing Assessment
Assess for the following:
- Edema. Observe for edema when performing physical examination of the child with nephrotic syndrome.
- Weigh and measure. Weigh the child and record the abdominal measurements to serve as a baseline.
- Vital signs. Obtain vital signs, including blood pressure.
- Pitting edema. Note any swelling about the eyes or the ankles and other dependent parts.
- Skin. Inspect the skin for pallor, irritation, or breakdown; examine the scrotal area of the male child for swelling, redness, and irritation.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Excess fluid volume related to fluid accumulation in tissues and third spaces.
- Risk for imbalanced nutrition: less than body requirements related to anorexia.
- Risk for impaired skin integrity related to edema.
- Fatigue related to edema and disease process.
- Risk for infection related to immunosuppression.
- Deficient knowledge of the caregiver related to disease process, treatment, and home care.
- Compromised family coping related to care of a child with chronic illness.
Nursing Care Planning and Goals
The major nursing care planning goals for the child with nephrotic syndrome are:
- Relieving edema.
- Improving nutritional status.
- Maintaining skin integrity.
- Conserving energy.
- Preventing infection.
Nursing Interventions
Nursing interventions for a child with nephrotic syndrome are:
- Monitoring fluid intake and output. Accurately monitor and document intake and output; weigh the child at the same time every day, on the same scale in the same clothing; measure the child’s abdomen daily at the level of the umbilicus.
- Improving nutritional intake. Offer a visually appealing and nutritious diet; consult the child and the family to learn which foods are appealing to the child; serving six small meals my help increase the child’s total intake better.
- Promoting skin integrity. Inspect all skin surfaces regularly for breakdown; turn and position the child every 2 hours; protect skin surfaces from pressure by means of pillows and padding; protect overlapping skin surfaces from rubbing by careful placement of cotton gauze; bathe the child regularly; a sheer dusting of cornstarch ma be soothing to the skin.
- Promoting energy conservation. Bed rest is common during the edema stage of the condition; balance the activity with rest periods and encourage the child to rest when fatigued; plan quiet, age-appropriate activities that interest the child.
- Preventing infection. Protect the child from anyone with an infection: staff, family, visitors, and other children; handwashing and strict medical asepsis are essential; and observe for any early signs of infection.
Evaluation
Goals are met as evidenced by:
- Relief from edema.
- Improvement of nutritional status.
- Maintenance of skin integrity.
- Conservation of energy.
- Prevention of infection.
Documentation Guidelines
Documentation in a patient with nephrotic syndrome include:
- Temperature and other assessment findings, including vital signs.
- Causative and contributing factors.
- Impact of condition on personal image and lifestyle.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress towards desired outcomes.
- Modifications to plan of care.


















Leave a Comment