In the realm of maternal care, understanding and monitoring fetal development and fetal growth are paramount for ensuring the well-being of both the mother and the developing baby. The intricate processes of fetal development, from conception to birth, lay the foundation for a healthy and successful transition into the world outside the womb. Likewise, monitoring fetal growth throughout pregnancy aids in identifying potential complications early on, enabling healthcare professionals to provide timely interventions and personalized care.
This article aims to provide nursing professionals with an essential guide to fetal development and fetal growth assessment. By delving into the latest research and evidence-based practices, we aim to equip nurses with the knowledge and skills necessary to promote optimal outcomes for expectant mothers and their unborn children.
Fetal Development
Fertilization
Fertilization is the process wherein the ovum and the spermatozoa unite at the ampullary portion of the fallopian tube, the usual site of fertilization.
- A mature ovum can only be fertilized within 24 to 48 hours after being released.
- The functional life of the spermatozoa is only 48 to 72 hours.
- The best time that fertilization would occur is 72 hours after sexual intercourse.
- The fertilized ovum is propelled along the tube through the help of the peristaltic movements of the fallopian tube and the tube’s cilia.
- The average time that the sperm can reach the cervix is within 90 seconds, and it can reach the outer fallopian tube within 5 minutes.
- If the ovum has already been penetrated by a spermatozoon, it changes its composition so that it becomes impermeable to other spermatozoa.
- After penetration, the chromosomal materials of both the ovum and the spermatozoon combine to form a zygote.
- Three factors determine the certainty of fertilization:
- the maturation of both the sperm and the ovum;
- the ability of the sperm to reach the ovum; and
- the ability of the sperm to penetrate the cell membrane and achieve fertilization.
Implantation
- The migration of the zygote towards the uterus reaches 3 to 4 days, and it is propelled by the muscular contractions in the fallopian tube.
- Mitotic cell division or cleaving starts after 24 hours. The rate of cleaving is an average of one every 22 hours.
- As the zygote reaches the uterus, it already has 16 to 50 cell divisions, and it is now called a morula because of its bumpy appearance.
- The morula floats freely along the body of the uterus within 3 to 4 days, and it becomes a blastocyst.
- The blastocyst attaches into the endometrium, and this process is called implantation, which occurs 8 to 10 days after fertilization.
- Apposition, or the brushing of the blastocyst against the endometrium, is the first part of implantation.
- Adhesion occurs afterwards as the blastocyst attaches to the surface of the endometrium, then invasion, as it settles into the folds of the endometrium.
- On the day of implantation, the woman may experience a small amount of vaginal spotting as the capillaries by the implanting blastocyst.
- As implantation occurs, the zygote now becomes an embryo.
Fetal Structures
Deciduas

- The uterine endometrium continues to thicken because of the corpus luteum that is influenced by hCG, and instead of sloughing off in a usual menstrual cycle, it becomes the deciduas.
- The deciduas are divided into three parts: basalis, capsularis, and vera.
- The decidua basalis is the innermost portion of the layer which rests directly under the embryo.
- The decidua capsularis encapsulates the trophoblast’s surface.
- The decidua vera becomes the remaining portion of the uterine lining,and sheds as the lochias.
- Eventually, the deciduas vera and capsularis fuse because of the enlarging embryo.
Chorionic Villi
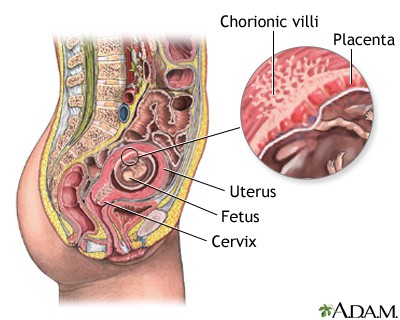
- On the 11th or 12th day, the chorionic villi start to form from the miniature villi that protrude from a single layer of cells to start the formation of placenta.
- The chorionic villi have a central core and fetal capillaries, and a double layer of trophoblast cells.
- The syncytial layer or the outer portion of the two layers produces placental hormones such as hPL, hCG, estrogen, and progesterone.
- The Langhans’ layer is the middle layer and it protects the embryo and fetus from infectious diseases. This layer appears to function as early as 12 days’ gestation.
- The layer disappears on the 20th to 24th week of gestation, however, leaving the fetus more susceptible to infections.
Placenta
The placenta, which is a Latin term for “pancake” for its appearance came from the trophoblast tissues and has a lot of functions that benefit the fetus.
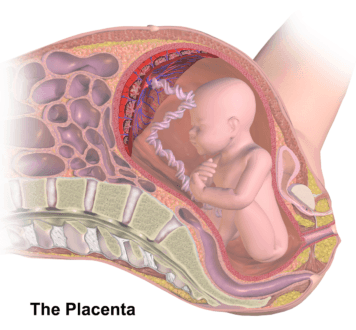
- Nutrients such as glucose, amino acids, vitamins, minerals, fatty acids, and water as well as oxygen are transported through the placenta from the maternal blood supply to the fetus.
- Placental osmosis also plays an essential part in maintaining the health of the fetus. it is impermeable to a few harmful substances, thereby it does not allow the crossing of these substances towards the fetal blood circulation.
- The syncytial layer produces various hormones that benefit both the mother and the fetus.
- The human chorionic gonadotropin is the first placental hormone to be produced, and it ensures that the corpus luteum would continue to produce estrogen and progesterone to support the pregnancy.
- Estrogen is also one of the hormones produced by the syncytial cells and it aids in the uterine growth and the development of the mammary glands in preparation for lactation.
- Progesterone is responsible for maintaining the lining of the uterus during pregnancy. It also reduces the contractility of the uterus to prevent preterm labor.
- Human placental lactogen promotes lactogenic properties and mammary growth in preparation for the lactation of the mother.
Amniotic Membranes
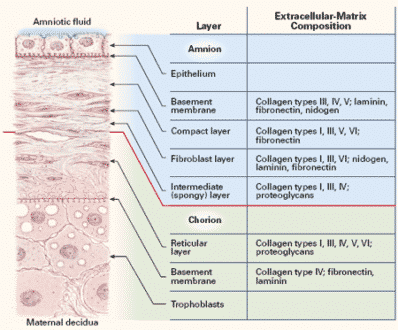
- The smooth portion of the chorionic villi eventually becomes the chorionic membrane which forms the sac that contains the amniotic fluid.
- The amniotic membrane forms under the chorion, giving an appearance that seem like they are only one membrane.
- The amniotic membrane is also responsible for producing the amniotic fluid and the phospholipids that triggers the formation of prostaglandins, the hormone that initiates uterine contractions.
Amniotic Fluid
- The normal amount of amniotic fluid is 800 to 1000 mL.
- The role of the amniotic fluid in the safety of the fetus is it protects the fetus from trauma or pressure to the mother’s abdomen. It also regulates the temperature for the fetus and aids in muscular development allowing the fetus to move freely
- The amniotic fluid also protects the umbilical cord from trauma and pressure, thereby protecting the fetal oxygen supply.
Umbilical Cord
- The amnion and chorion compose the umbilical cord which connects the embryo to the chorionic villi of the placenta.
- The main function of the umbilical cord is the transport of oxygen and nutrients from the placenta to the fetus and the return of waste products from the fetus to the placenta.
- The cord is made up of a gelatinous mucopolysaccharide called Wharton’s jelly that protects the vein and arteries from trauma.
- The umbilical cord contains only one vein, which carries blood from the placenta to the fetus, and two arteries, which carries blood from the fetus to the placenta.
Fetal Milestones
4th Week of Gestation
- Spinal cord is formed and fused at the midpoint.
- Head folds forward and is prominent.
- The back is bent, which makes the head almost touch the tail.
- A prominent bulge appears which would later form as the heart.
- Lateral wings, the body, folds forward and fuse at midline.
- Arms and legs are budlike structures.
- Eyes, ears, and nose are barely recognizable.
8th Week of Gestation
- Organogenesis is achieved and complete.
- The heart already developed a septum and valves and is beating rhythmically.
- Arms and legs have developed.
- Facial features are noticeable.
- The genital starts to form but is not yet recognizable.
- Fetal intestine is rapidly growing.
- Results of an ultrasound would show a gestational sac which confirms pregnancy.
12th Week of Gestation
- The toes and fingers already have nail beds.
- Faint fetal movements are starting.
- Early reflexes are present.
- Tooth buds are forming.
- Formation of bone ossification centers initiate.
- The genital is already recognizable through its appearance.
- Urine secretion begins but is not yet evident.
- Heartbeat could be detected by Doppler.
16th Week of Gestation
- An ordinary stethoscope could detect the fetus’ heart beat.
- Lanugo has started to form.
- The pancreas and liver are forming.
- Urine is present in the amniotic fluid.
- Fetus starts to swallow the amniotic fluid.
- Ultrasound could determine the sex of the fetus.
20th Week of Gestation
- Mother could sense spontaneous fetal movements.
- There is hair formation on the head until the eyebrows.
- The upper intestine contains meconium.
- Brown fat starts to form behind the kidneys, sternum, and posterior neck.
- Vernix caseosa also starts to form and covers the skin.
- Passive antibody transfer begins.
- The sleep and activity patterns of the fetus are evident.
24th Week of Gestation
- Lung surfactant begins to develop.
- Meconium is present at the rectum.
- Eyebrows and eyelashes are distinguishable.
- Eyelids can now open.
- Pupils react to light.
- The fetus has reached the age of viability, wherein they could survive externally if cared for in a modern intensive facility.
- Responds to sudden sounds.
28th Week of Gestation
- Surfactant is demonstrated in the amniotic fluid.
- Alveoli are starting to mature.
- Testes descend into the scrotal sac.
- Retinal blood vessels start to form but are highly susceptible to damage.
32nd Week of Gestation
- Subcutaneous fat is deposited.
- Fetus responds to sounds outside the mother’s body through movements.
- Active Moro reflex is present.
- Iron stores are starting to develop.
- Fingernails are starting to grow.
36th Week of Gestation
- Depositions of iron, carbohydrate, calcium, and glycogen stores are in the body.
- Additional subcutaneous fats are deposited.
- One or two creases are present at the sole of the foot.
- Lanugo starts to diminish.
- Some babies turn and assume a vertex presentation.
40th Week of Gestation
- Fetus now kicks very actively and hard enough to cause discomfort.
- The fetal hemoglobin is being converted to adult hemoglobin.
- Vernix caseosa is fully formed.
- Fingernails extend to the fingertips.
- The soles of the feet have creases that cover at least two-thirds of the surface.
The slow but sure development of the fetus inside a woman’s body should be monitored to ensure the delivery of a healthy and safe baby. Fetal development is a critical stage in a mother’s responsibility over her children. The role of a mother starts not only during the time that the baby is born, but most especially when she decides that she wants to conceive an offspring.
Fetal Growth Assessment
Estimating Fetal Growth
McDonald’s Rule
- McDonald’s rule is the measurement of the fundal height from the symphysis pubis.
- To measure, instruct the woman to lie supine and start measuring from the symphysis pubis to the uterine fundus.
- The distance between in centimeters depicts the week of gestation between the 20th to the 31st weeks of pregnancy.
- At 12 weeks, the uterine fundus should be at the level of the symphysis pubis.
- At 20 weeks, the uterine fundus should be at the level of the umbilicus.
- At 36 weeks, the uterine fundus should be at the level of the xiphoid process.
Fetal Movement
- Quickening or the first fetal movement that is felt by the mother usually starts at 18 to 20 weeks of pregnancy.
- A healthy fetus moves at an average of at least 10 times a day.
- In the Sandovsky method, to assess the fetal movement, ask the woman to lie in a recumbent position after a meal and record the number of fetal movements within an hour.
- In every 10 minutes, the fetus normally moves at least twice or 10 to 12 times in an hour.
- If there is less than 10 movements in an hour, the woman should repeat the procedure for the next hour.
- The Cardiff method or the “Count-to-Ten” method, the woman records the time interval between every 10 fetal movements she feels within 60 minutes.
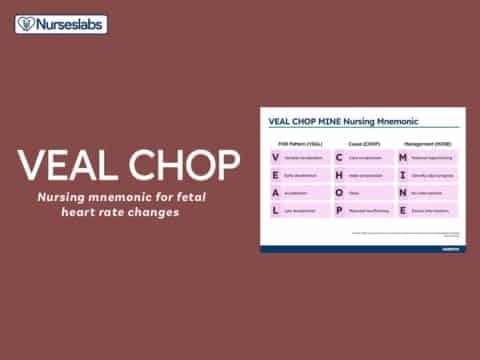
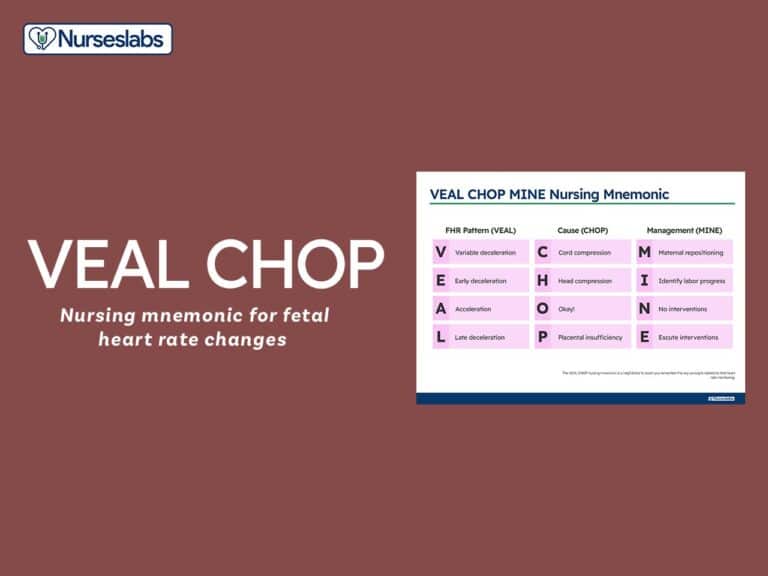
Fetal Heart Rate
Rhythm Strip Testing
- The normal fetal heart rate is 120 to 160 beats per minute.
- In rhythm strip testing, the fetal heart rate is assessed if a good baseline heart rate or a degree of variability is present.
- The results are categorized as absent (none apparent), minimal (extremely small fluctuations), moderate (a range of 6-25 beats per minute), and marked (range over 25 beats per minute).
- The rhythm strip testing is done as the woman is asked to remain in a fixed position for 20 minutes.
Nonstress Test
- In a nonstress testing, the response of the fetal heart rate is measured in response to the fetal movement.
- The woman is attached to a fetal heart rate and uterine contraction monitor.
- The woman should push the button of the monitor whenever she feels the fetus move.
- Normally, when the fetus moves, the fetal heart should increase for about 15 beats per minute and remain elevated for 15 seconds.
- The nonstress test is done for 10 to 20 minutes.
- The result is reactive if there are two accelerations of fetal heart rate lasting for 15 seconds that occurs after movement.
- The result is non reactive if there are no fetal accelerations after a fetal movement, or there is no fetal movement.
- If the nonstress test is nonreactive, a contraction stress test or biophysical profile will be scheduled.
Contraction Stress Testing
- In contraction stress testing, the fetal heart rate is assessed in conjunction with uterine contractions.
- The woman is attached to an external uterine contraction and fetal heart rate monitor.
- The woman is instructed to roll a nipple between her fingers and thumb to produce uterine contractions.
- Within a 10-minute window, three contractions with a duration of 40 seconds or longer must be present.
- The test is negative or normal if there are no decelerations in the fetal heart rate during contractions.
- It is positive or abnormal if there is a late deceleration at the end of a contraction and even after the contraction.
Ultrasonography
- Ultrasonography measures the response of sound waves against solid objects.
- It can diagnose a pregnancy of 6 weeks’ gestation, confirm the presence, size, and location of the placenta, establish that the fetus is growing, detect any gross anomalies, establish the fetal sex, and determine the presentation and position of the fetus.
- The woman has to have a full bladder at the time of the procedure.
- Have the woman drink a full glass of water every 15 minutes 90 minutes before the procedure until the start of the procedure.
- Ultrasonography is also used to predict fetal maturity by the measurement of the biparietal diameter of the fetal head.
- Placental grading can also be done through ultrasound as 0 (12 to 24 weeks), 1 (30 to 32 weeks), 2 (36 weeks), and 3 (38 weeks).
- The amount of amniotic fluid present can also be detected through ultrasonography and is also a way to estimate fetal health.
Electrocardiography
- As early as the 11th week of pregnancy, fetal ECG can be recorded.
- However, fetal ECG is inaccurate before the 20th week as the fetal electrical conduction is still weak.
Magnetic Resonance Imaging
- MRI does not have any harmful effects to both the mother and the fetus, and is now largely considered as one of the preferred fetal assessment techniques.
- MRI can diagnose complications like ectopic pregnancy and trophoblastic disease or H-mole because fetal movements could hide the findings later in pregnancy.
Maternal Serum Alpha Fetoprotein
AFP is found in the amniotic fluid and the maternal serum and is produced by the fetal liver.
- MSAFP levels start to increase at 11 weeks’ gestation and increases steadily until term.
- The MSAFP level is abnormally high if there is a spina bifida defect or abdominal defect.
- The MSAFP level is low if the fetus has a chromosomal defect such as Down syndrome.
- The MSAFP is assessed at the 15th week of pregnancy and can detect 85% to 90% of neural tube defects and 80% of Down syndrome.
Amniocentesis
Amniocentesis is the aspiration of amniotic fluid from the pregnant uterus for examination.
- The test is typically done between the 14th and 16th weeks of pregnancy so that there is a generous amount of amniotic fluid present.
- Before the procedure, instruct the woman to void, and then place her on a supine position.
- Fetal heart rate and uterine contraction monitors are attached to the woman, and blood pressure and fetal heart rate are taken.
- An ultrasound is performed first to determine the position of the fetus and the location of a pocket of amniotic fluid and the placenta.
- Antiseptic solution is applied to the abdomen and local anesthetic is injected.
- Inform the woman that she might feel pressure as the needle is introduced, but do not advise her to take a deep breath and hold it in.
- About 15 mL of amniotic fluid is aspirated.
- Amniotic fluid is analyzed for AFP, bilirubin determination, chromosome analysis, color, fetal fibronectin, inborn errors of metabolism, lecithin-sphingomyelin ratio, and phosphatidylglycerol and desaturated phosphatidylcholine.
Biophysical Profile
- The biophysical profile combines five parameters into one assessment.
- Fetal heart rate and breathing measure short-term central nervous system function.
- The amniotic fluid volume measures long-term adequacy of placental function.
- The biophysical profile is more accurate than any other single assessment method.
- The score ranges from 2-10, with 10 as the highest.
- If the fetus has a score of 8 to 10, it is doing well.
- If the score is 6, this is considered suspicious.
- A score of 4 denotes that fetus might be in jeopardy.
- The assessment is similar to that of an Apgar scoring, and it is commonly called as fetal Apgar.
Fetal assessment is just one of the many assessments that a pregnant woman must undergo to ensure the health of the fetus and even her own health. Undergoing these tests can give comfort to the mother regarding the status of her baby’s health, and compliance of her health care provider’s orders is the key to a healthy and safe pregnancy.



















Leave a Comment