Lumbar puncture, also known as spinal tap, is an invasive procedure where a hollow needle is inserted into the space surrounding the subarachnoid space in the lower back to obtain samples of cerebrospinal fluid (CSF) for qualitative analysis. Most of the disorders of the central nervous system are diagnosed in relation to the changes in the composition and dynamics of the CSF.
A lumbar puncture may also be used to measure CSF, instill medications, or introduce a contrast medium into the spinal canal. The procedure usually takes around 30 to 45 minutes and can be done on an outpatient basis at a hospital or clinic.
One of the responsibilities of the nurse during a lumbar puncture is to provide information and instructions before, during, and after the procedure. It will decrease fear and anxiety among the patient and their families, and it will also lessen the occurrence of potential complications post-lumbar puncture.
Table of Contents
- Indication
- Contraindication
- Equipment
- Procedure
- Nursing Responsibility for Lumbar Puncture
- Normal Results
- Abnormal Results
- Complications
- Gallery
- References
Indication
Lumbar puncture is indicated for the following reasons:
- Measure cerebrospinal fluid (CSF) pressure
- Assist in the diagnosis of suspected CNS infections (bacterial or viral meningitis, meningoencephalitis), intracranial or subarachnoid hemorrhage, and some malignant disorders
- Evaluate and diagnose demyelinating or inflammatory CNS processes such as Multiple Sclerosis, Guillan-Barré Syndrome (GBS), Acute Disseminated Encephalomyelitis (ADEM)
- Infuse medications which include spinal anesthesia before surgery, contrast material for diagnostic imaging such as CT-myelography, and chemotherapy drugs directly into the spinal canal
- Treat normal pressure hydrocephalus, cerebrospinal fistulas, and idiopathic intracranial hypertension (IIH).
- Placement of a lumbar CSF drainage catheter
Contraindication
Absolute contraindications for lumbar puncture are as follows:
- Increased intracranial pressure due to a brain tumor. Cerebral or cerebellar herniation with severe neurological deterioration may occur after the withdrawal of CSF fluid.
- Skin infection near the puncture site. The presence of skin infection near the site of the lumbar puncture increases the risk of contamination of infected material into the CSF.
- Severe degenerative vertebral joint disease. There will be difficulty in passing the needle through the degenerated arthritic interspinal space.
- Severe coagulopathy. Due to the significant risk of epidural hematoma formation.
Equipment
The lumbar puncture kit contains:
- Sterile gloves
- Sterile drapes and procedure tray
- Sterile gauze pads
- Aseptic solution: povidone-iodine solution (Betadine)
- Local anesthetic: Lidocaine 1% solution
- 25G needle
- 10ml syringe (1)
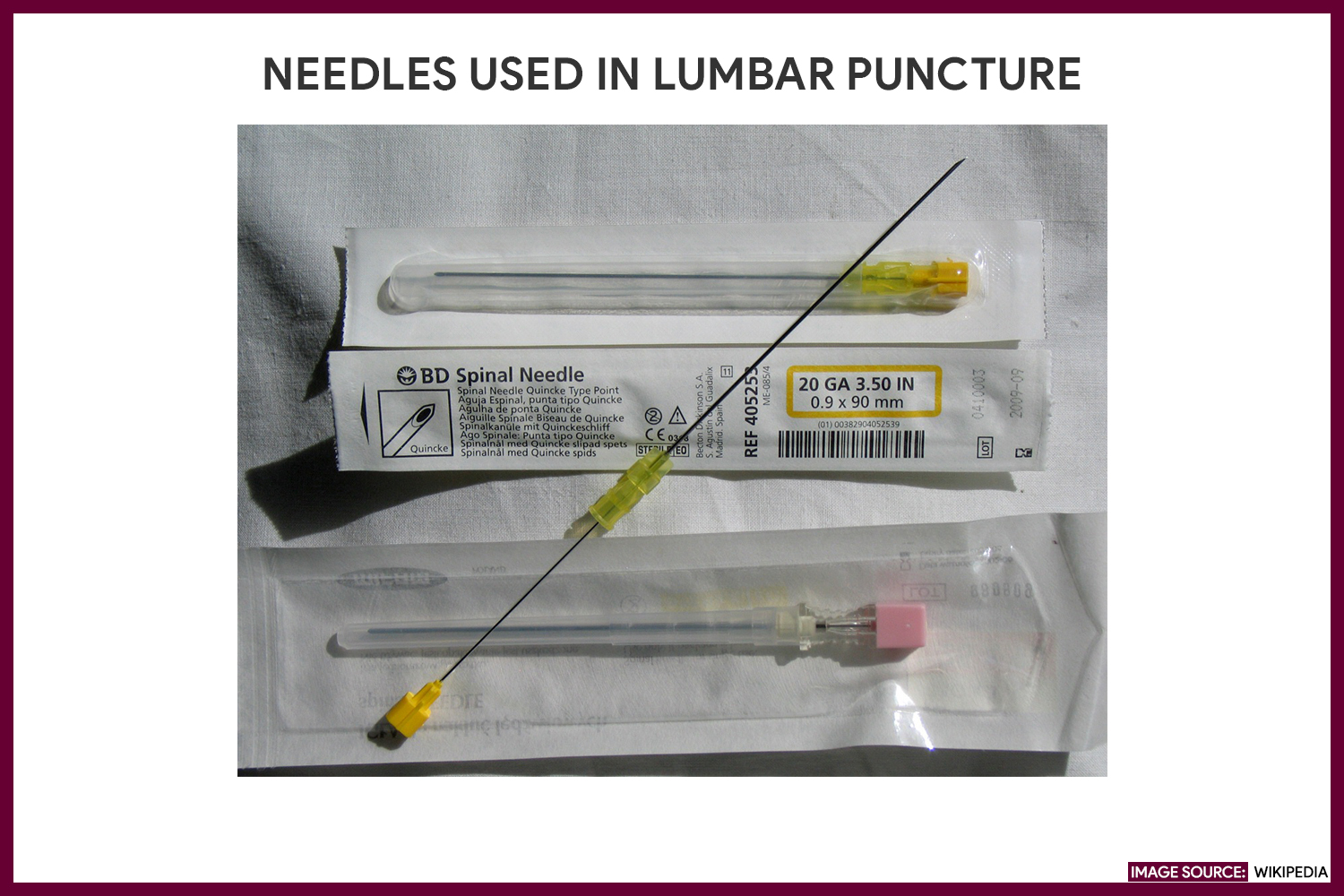
- Spinal needle with stylet (size 22G or 25G)
- CSF tube (2 to 4)
- Stopcock
- Manometer tubing
Procedure
The step-by-step procedure for a lumbar puncture (spinal tap) is as follows:
- Position the patient in a fetal position.
The patient is positioned on his side at the edge of the bed with his knees drawn up to his abdomen and chin tucked against his chest (fetal position) or sitting while leaning over a bedside table. When the patient is positioned supine, pillows are provided to support the spine on a horizontal plane.
- Sterilize the site of insertion.
The skin site is prepared and draped, and a local anesthetic is injected.
- Insert the spinal needle.
The spinal needle is inserted in the midline between the spinous processes of the vertebrae (usually between the third fourth or fourth and fifth lumbar vertebrae).
- Remove the stylet from the needle.
The stylet is removed from the needle. CSF will drip out of the needle if it’s properly positioned. A stopcock and manometer are attached to the needle to measure the initial (opening) CSF pressure.
- Collect specimen.
Specimens are collected and placed in the appropriate containers.
- Remove the needle.
The needle is removed, and a small sterile dressing is applied.
Nursing Responsibility for Lumbar Puncture
The following are the nursing interventions and nursing care considerations for a patient indicated for lumbar puncture:
Before the procedure
The following are the nursing interventions prior to a lumbar puncture:
- Explain the procedure to the patient. Explain to the patient the purpose of lumbar puncture, how and where it’s done, and who will perform the procedure.
- Obtain informed consent. Make sure the patient has signed a consent form if required by the institution.
- Reinforce diet. Advise the patient that fasting is not required.
- Promote comfort. Instruct the patient to empty the bladder and bowel before the procedure.
- Establish baseline assessment data. Do vital signs monitoring and neurologic assessment of the legs by assessing the patient’s movement, strength, and sensation.
- Place the client in a lateral decubitus position. Assist the client to assume a lateral decubitus (fetal) position, near the side of the bed with the neck, hips, and knees drawn up to the chest. An alternative position is to have the patient sit on the edge of the bed while leaning over a bedside table.
- Instruct to remain still. Explain that he or she must lie very still throughout the procedure. Any unnecessary movement may cause traumatic injury.
After the procedure
The nurse should note the following nursing interventions post-lumbar puncture:
- Apply brief pressure to the puncture site. Pressure will be applied to avoid bleeding, and the site is covered by a small occlusive dressing or band-aid.
- Place the patient flat on the bed. The patient remains flat on the bed for 4 to 6 hours depending on the physician. He or she may turn from side to side as long as the head is not elevated.
- Monitor vital signs, neurologic status, and intake and output. Take vital signs, measure intake, and output, and assess neurologic status at least every 4 hours for 24 hours to allow further evaluation of the patient’s condition.
- Monitor the puncture site for signs of CSF leakage and drainage of blood. Signs of CSF leakage include positional headaches, nausea and vomiting, neck stiffness, photophobia (sensitivity to light), sense of imbalance, tinnitus (ringing in the ear), and phonophobia (sensitivity to sound).
- Encourage increased fluid intake. An increased amount of fluid intake (up to 3,000 ml in 24 hours) will replace CSF removed during the lumbar puncture.
- Label and number the specimen tube correctly. Ensure all samples are properly labeled and sent to the laboratory immediately for further evaluation.
- Administer analgesia as ordered. Headaches after the procedure can last for a few hours or days and are usually treated with analgesics.
Normal Results
CSF samples for analysis with normal values typically range as follows:
- Pressure: 70 to 180 mm H20.
- Appearance: CSF is normally clear and colorless.
- CSF total protein: 15-45 mg/dL
- Gamma globulin: 3 to 12% of the total protein
- CSF glucose: 50 to 80 mg/dl
- CSF cell count: Normal CSF contains no red blood cells (RBCs), and the white blood cell (WBC) count is 0-5 WBCs per microliter (all mononuclear)
- CSF Chloride: 118 to 130 mEq/L
- Gram stain: No microorganism (bacteria, fungi, or virus) is present.
Abnormal Results
These are the abnormal findings that can be found in CSF analysis:
- Pressure:
- Increased intracranial pressure (ICP) occurs as a result of a tumor, hemorrhage, or trauma-induced edema.
- Decreased intracranial pressure (ICP) may reveal a spinal subarachnoid obstruction.
- Appearance:
- Cloudy appearance indicating infection.
- Yellow to reddish appearance indicating spinal cord obstruction or intracranial hemorrhage.
- Brown to orange appearance indicating increased protein levels or RBC breakdown.
- CSF Protein:
- Increased protein indicating tumor, trauma, diabetes mellitus, or blood in cerebrospinal fluid (CSF).
- Decreased protein indicates rapid CSF production.
- Gamma globulin:
- Increased gamma globulin indicates a demyelinating disease such as multiple sclerosis, neurosyphilis, or Guillan-Barré Syndrome.
- CSF Glucose:
- Increased glucose indicates high blood sugar (hyperglycemia).
- Decreased glucose indicates low blood sugar (hypoglycemia), bacterial or fungal infection, tuberculosis, or meningitis.
- CSF cell count:
- Increased white blood cells in the CSF suggest meningitis, tumor, abscess, acute infection, stroke, or demyelinating disease.
- Red blood cells in the CSF indicate bleeding into the spinal fluid or the result of a traumatic lumbar puncture.
- CSF Chloride:
- Decreased chloride indicating infected meninges.
- Gram stain:
- Gram-positive or Gram-negative organisms indicate bacterial meningitis.
Complications
The possible complications after a lumbar puncture are:
- Post-lumbar puncture headache. The most common complication of LP occurs due to the leakage of CSF from the puncture site or into the tissues around it. The pain is aggravated while sitting, standing, or coughing and resolves after lying down.
- Back pain. Pain or discomfort in the lower back may happen as a result of trauma to the local soft tissue.
- Pain or numbness. A feeling of tingling sensation and numbness in the lower back and legs is felt temporarily.
- Bleeding. Bleeding is usually noted in the area of the punctured site, or in some rare cases into the subarachnoid, subdural, or epidural space.
- Brainstem herniation: The increased pressure caused by the removal of CSF during LP will cause a sudden shifting of brain tissue that can lead to the compression or herniation of the brainstem.
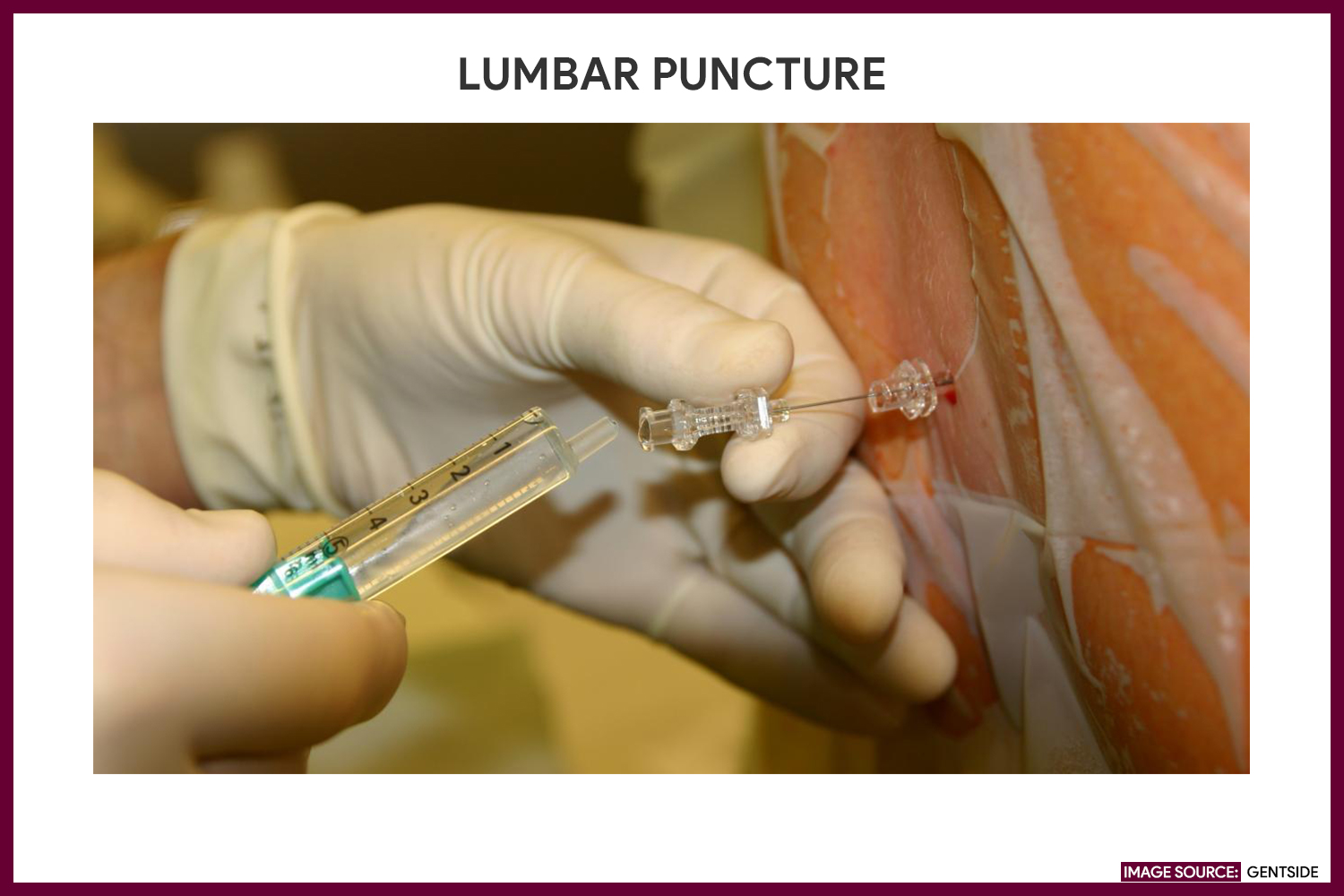
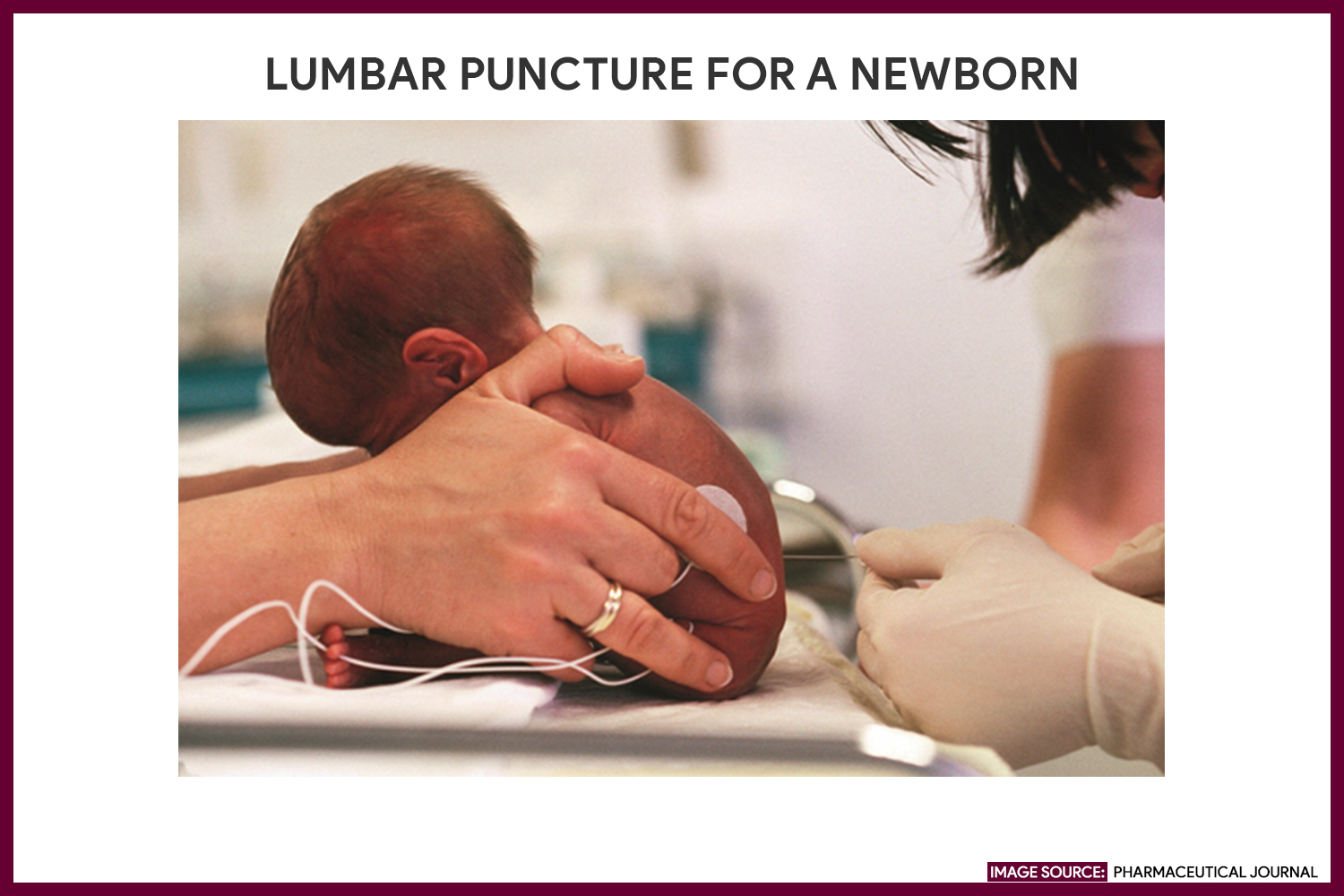
Gallery
Images related to lumbar puncture:
References
Additional resources and references for this guide:
- Lumbar puncture. (2018). Retrieved from https://www.nhs.uk/conditions/lumbar-puncture/
- Chernecky, C., & Berger, B. (2013). Laboratory tests and diagnostic procedures. St. Louis, Mo.: Elsevier/Saunders.
- Sempere, A. P., Berenguer-Ruiz, L., Lezcano-Rodas, M., Mira-Berenguer, F., & Waez, M. (n.d.). [Lumbar puncture: Its indications, contraindications, complications and technique]. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/17918111
- Wright BL, e. (2018). Cerebrospinal fluid and lumbar puncture: a practical review. – PubMed – NCBI. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22278331



The information I needed to know about lumber puncture was very good and helpful. Thank you so much!
It was well detailed and easily to understand, and as a nurse I will be able to render proper nursing care for the patient will undergo with lumbar puncture procedure.