Hydrocephalus, a complex neurological condition, poses significant challenges for healthcare professionals, particularly nurses, in providing specialized care to individuals affected by this condition. Characterized by the abnormal accumulation of cerebrospinal fluid within the brain, hydrocephalus can result in elevated intracranial pressure, leading to various neurological impairments.
Nurses play a crucial role in the multidisciplinary team, actively contributing to the assessment, management, and support of patients with hydrocephalus throughout their healthcare journey.
What is Hydrocephalus?
Hydrocephalus affects hundreds of thousands of Americans, in every stage of life, from infants to the elderly.
- The term hydrocephalus is derived from two words: “hydro,” meaning water, and “cephalus,” referring to the head.
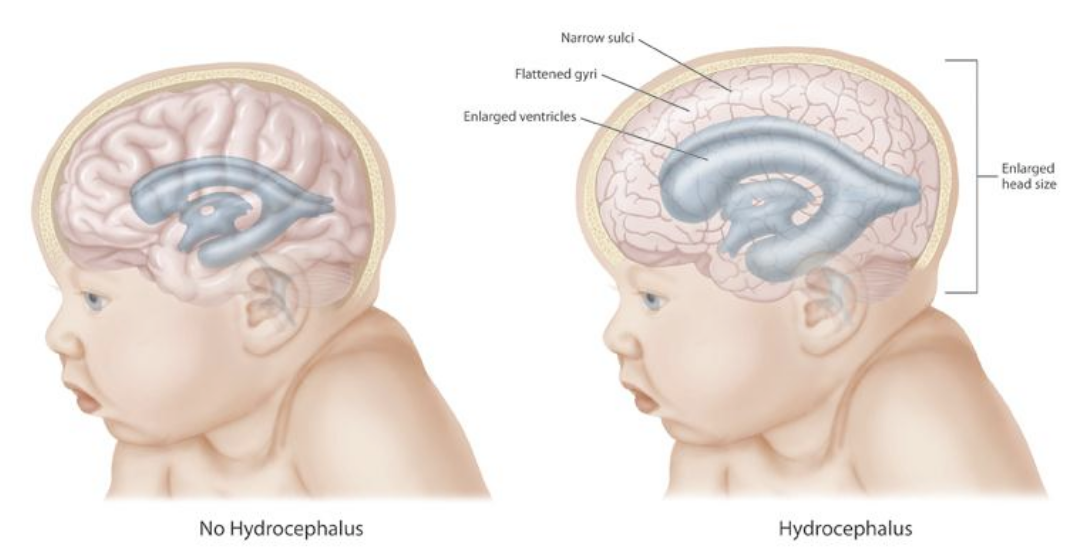
- Hydrocephalus is a neurological condition characterized by the abnormal accumulation of cerebrospinal fluid (CSF) within the brain’s ventricles, leading to an increase in intracranial pressure. This condition can occur at any age and may result from various underlying causes, such as congenital malformations, infections, tumors, or traumatic brain injuries.
- This condition could also be termed a hydrodynamic CSF disorder.
Classification
There are two types of hydrocephalus:
- Noncommunicating. In the noncommunicating type of congenital hydrocephalus, an obstruction occurs in the free circulation of CSF.
- Communicating. In the communicating type of hydrocephalus, no obstruction of the free flow of the CSF exists between the ventricles and the spinal theca; rather, the condition is caused by defective absorption of CSF, thus causing increased pressure on the brain or spinal cord.
Pathophysiology
The pathophysiology of hydrocephalus occurs as follows:
- Normally, a delicate balance exists between the rate of formation and absorption of CSF.
- In hydrocephalus, this balance is disturbed.
- CSF is formed mainly in the lateral ventricles by the choroid plexus and is absorbed into the venous system through the arachnoid villi.
- CSF circulates within the ventricles and the subarachnoid space.
- An obstruction may occur in the free circulation of CSF; this blockage causes increased pressure on the brain or spinal cord.
- The site of obstruction may be at the foramen of Monro, the aqueduct of Sylvius, the foramen of Luschka, or the foramen of Magendie.
- If there is no obstruction, the condition may be caused by defective absorption of CSF, thus causing increased pressure on the brain or spinal cord.
Statistics and Incidences
Hydrocephalus cases are affecting the entire world every day.
- The incidence of congenital hydrocephalus is 3 per 1, 000 live births; the incidence of acquired hydrocephalus is not known exactly due to the variety of disorders that may cause it.
- Incidence of acquired hydrocephalus is unknown.
- Shunt dependence occurs in 75% of all cases of treated hydrocephalus and in 50% of children with communicating hydrocephalus.
- Incidence is equal in males and females.
- Incidence of human hydrocephalus presents a bimodal age curve; one peak occurs in infancy and is related to the various forms of congenital malformations.
- Adult hydrocephalus represents approximately 40% of total cases of hydrocephalus.
Causes
Causes usually are genetic factors and how the fetus develops.
- Obstruction. The most common problem is a partial obstruction of the normal flow of CSF, either from one ventricle to another or from the ventricles to other spaces around the brain.
- Poor absorption. Less common is a problem with the mechanisms that enable the blood vessels to absorb CSF; this is often related to inflammation of brain tissues from disease or injury.
- Overproduction. Rarely, the mechanisms for producing CSF create more than normal and more quickly than it can be absorbed.
Clinical Manifestations
Clinical features of hydrocephalus are influenced by the patient’s age, the cause of the hydrocephalus, the location of the obstruction, its duration, and its rapidity of onset.
- Poor feeding. The infant with hydrocephalus has trouble in feeding due to the difficulty of his condition.
- Large head. An excessively large head at birth is suggestive of hydrocephalus.
- Bulging of the anterior fontanelles. The anterior fontanelle becomes tense and bulging, the skull enlarges in all diameters, and the scalp becomes shiny and its veins dilate.
- Setting sun sign. If pressure continues to increase without intervention, the eyes appear to be pushed downward slightly with the sclera visible above the iris- the so-called setting sun sign.
- High-pitched cry. The intracranial pressure may increase and the infant’s cry could become high-pitched.
- Irritability. Irritability is also caused by an increase in the intracranial pressure.
- Projectile vomiting. An increase in the intracranial pressure can cause projectile vomiting.
Assessment and Diagnostic Findings
Examination in infants may include the following:

- Computed tomography (CT) scanning. CT scan is used to assess the size of ventricles and other structures.
- Magnetic resonance imaging (MRI). MRI is used to assess for Chiari malformation or cerebellar or periaqueductal tumors.
- Ultrasonography through anterior fontanelle in infants. This study assesses for subependymal and intraventricular hemorrhage; to follow infants for possible progressive hydrocephalus.
- Skull radiography. To detect erosion of sella turcica, or “beaten copper cranium” (or “beaten silver cranium”)—the latter can also be seen in craniosynostosis; (after shunt insertion) to confirm correct positioning of installed hardware.
- MRI cine. To measure CSF stroke volume (SV) in the cerebral aqueduct; however, such measurements don’t appear to be useful in predicting response to shunting.
- Diffusion tensor imaging (DTI). To detect differences in fractional anisotropy and mean diffusivity of the brain parenchyma surrounding the ventricles; allows recognition of microstructural changes in periventricular white matter region that may be too subtle on conventional MRI.
- Radionuclide cisternography (in NPH). To assess the prognosis with regard to possible shunting—however, due to its poor sensitivity in predicting shunt response when the ventricular to total intracranial activity (V/T) ratio is less than 32%, this test is no longer commonly used.
Medical Management
The goal of treatment in clients with hydrocephalus is to reduce or prevent brain damage by improving the flow of CSF which may include surgery to provide shunting for drainage of the excess fluid from the ventricles to an extracranial space such as the peritoneum or right atrium (in older children) or management with medications to reduce ICP if progression is slow or surgery is contraindicated.
Pharmacologic Therapy
The following medications are used to treat hydrocephalus.
- Diuretics. Acetazolamide (ACZ) and furosemide (FUR) treat posthemorrhagic hydrocephalus in neonates; both are diuretics that also appear to decrease secretion of CSF at the level of the choroid plexus.
- Anticonvulsants. Helps to interfere impulse transmission of cerebral cortex and prevent seizures.
- Antibiotics. Culture and sensitivity dependent for shunt infections such as septicemia, ventriculitis, meningitis, or given as a prophylactic treatment.
Surgical Management
Surgical intervention is the only effective means of relieving brain pressure and preventing additional damage to the brain tissue.

- Surgery. Surgical treatment is the preferred therapeutic option in patients with hydrocephalus.
- Ventriculoperitoneal (VP) shunt. A ventriculoperitoneal (VP) shunt is a medical device that relieves pressure on the brain caused by fluid accumulation.
- Ventriculoatrial (VA) shunt. Ventriculoatrial shunt placement enables cerebrospinal fluid (CSF) to flow from the cerebral ventricular system to the atrium of the heart.
- Lumboperitoneal shunt. Only used for communicating hydrocephalus, CSF fistula, or pseudotumor cerebri).
- Torkildsen shunt (rarely). Effective only in acquired obstructive hydrocephalus.
- Ventriculopleural shunt (second-line therapy). Used if other shunt types contraindicated.
Nursing Management
Managing a child with hydrocephalus warrants skill and compassion for nurses and all the members of the healthcare team.
Nursing Assessment
Accurate information is essential in the assessment of the child with hydrocephalus.
- Head circumference. Measurement of the newborn‘s head is essential.
- Neurologic and vital signs. Obtaining accurate vital and neurologic signs is necessary before and after surgery.
- Check the fontanelles. If the fontanelles are not closed, carefully observe them for any signs of bulging.
- Monitor increase in intracranial pressure. Observe, report, and document all signs of IICP.
- History taking. If the child has returned for revision of an existing shunt, obtain a complete history before surgery from the family caregiver to provide a baseline of the child’s behavior.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Risk for Injury related to increased ICP.
- Risk for Impaired Skin Integrity related to pressure from physical immobility.
- Risk for Infection related to the presence of a shunt.
- Risk for Delayed Growth and Development related to impaired ability to achieve developmental tasks.
- Anxiety related to the family caregiver’s fear of the surgical outcome.
- Deficient Knowledge related to the family’s understanding of the child’s condition and home care.
Nursing Care Planning and Goals
Main Article: 5 Hydrocephalus Nursing Care Plans
The goals for the care of the newborn with hydrocephalus include:
- Preventing injury.
- Maintaining skin integrity.
- Preventing infection.
- Maintaining growth and development.
- Reducing family anxiety.
Nursing Interventions
Nursing interventions for the newborn with hydrocephalus include:
- Preventing injury. At least every 2 to 4 hours, monitor the newborn’s level of consciousness; check the pupils for equality and reaction; monitor the neurologic status, and observe for a shrill cry, lethargy, or irritability; measure and record the head circumference daily, and keep suction and oxygen equipment convenient at the bedside.
- Promoting skin integrity. After a shunting procedure, keep the newborn’s head turned away from the operative site until the physician allows a change in position; reposition the newborn at least every 2 hours, as permitted; inspect the dressings over the shunt site immediately after the surgery, every hour for the first 3 to 4 hours, and then at least every 4 hours.
- Preventing infection. Closely observe for and promptly report any signs of infection; perform wound care thoroughly as ordered, and administer antibiotics as prescribed.
- Promoting growth and development. The newborn needs social interaction and needs to be talked to, played with, and given the opportunity for activity; and provide toys appropriate for his mental and physical capacity.
- Reducing family anxiety. Explain to the family the condition and the anatomy of the surgical procedure in terms they can understand; encourage them to express their anxieties and ask questions; and give accurate, nontechnical answers that are easy to understand.
- Providing family teaching. Demonstrate care of the shunt to the family caregivers and have them perform a return demonstration; provide them with a list of signs and symptoms that should be reported, and discuss appropriate growth and development expectations for the child, and stress realistic goals.
Evaluation
Goals met are evidenced by:
- Prevention of injury.
- Maintenance of skin integrity.
- Prevention of infection.
- Maintenance of growth and development.
- Reduction of family anxiety.
Documentation Guidelines
Documentation for a patient with hydrocephalus includes:
- Individual risk factors including recent or current antibiotic therapy.
- Insertion sites, character of drainage.
- Signs and symptoms of infectious process.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress towards desired outcomes.
- Modifications to plan of care.
- Discharge needs.
































Leave a Comment