Ambulation is a nursing activity for patients with mobility problems due to illness, surgery, or prolonged periods of immobility. Helping patients walk safely promotes their physical recovery and prevents complications like pressure sores, respiratory problems, and muscle weakness. Nurses primarily offer support and guidance during ambulation, helping patients feel safe and comfortable. Knowing proper techniques, equipment use, and patient assessment methods is key to promoting safety and encouraging independence.
This article provides a comprehensive overview of ambulation’s importance, the preparation involved, techniques for safe ambulation assistance, and considerations for various patient populations.
What is Ambulation?
Ambulation, or the ability to walk from one location to another, is a component of recovery and independence for many patients. Assisting with ambulation refers to helping a patient walk safely, often using assistive devices such as gait belts, walkers, or canes. Depending on the patient’s condition, this assistance may vary from simple supervision to full physical support.
Importance of Ambulation
Ambulation is a fundamental part of recovery and rehabilitation. It benefits patients in numerous ways:
1. Promotes physical health. Regular ambulation helps maintain muscle strength, joint flexibility, and cardiovascular function. It reduces the risk of pressure ulcers, deep vein thrombosis (DVT), and pulmonary complications.
2. Psychological benefits. Walking and moving about can improve mood and reduce feelings of anxiety and depression. Ambulation fosters a sense of independence and control over one’s body, contributing to better mental health.
3. Enhances recovery. Early ambulation is linked to shorter hospital stays, reduced pain levels, and quicker recovery for post-operative patients. It encourages the return to normal function and activities of daily living (ADLs).
4. Prevents deconditioning. Patients who are immobile for extended periods can experience muscle atrophy and decreased endurance. Assisting with ambulation helps counteract these effects and maintain physical conditioning.
Individuals Who Require Assistance with Ambulation
Those who need help walking often face challenges related to strength, balance, coordination, or recovery from illness or surgery. Providing proper support during ambulation lessens the risk of falls and promotes independence and safety.
1. Post-Surgical Patients.
Patients recovering from surgery, especially orthopedic or abdominal procedures, often require assistance with ambulation due to pain, weakness, or limited mobility. Ambulating with support helps decrease the risk of postoperative complications such as blood clots and pneumonia.
2. Elderly Individuals.
Aging naturally leads to decreased muscle strength, balance, and coordination. Older adults often benefit from ambulation support to prevent falls and maintain independence in daily activities.
3. Neurological Patients.
Individuals with conditions such as stroke, Parkinson’s disease, or multiple sclerosis may experience impaired coordination, weakness, or paralysis. Assistance promotes their safety and supports gradual recovery of mobility.
4. Patients with Musculoskeletal Disorders.
Those with arthritis, fractures, or other bone and joint disorders may have pain or limited range of motion. Assisted ambulation allows for movement while minimizing discomfort and fall risk.
5. Postpartum Mothers.
Women recovering from childbirth, particularly cesarean delivery, may require help with initial ambulation to regain strength and prevent strain. Gradual movement also aids in circulation and uterine involution.
6. Patients with Visual or Cognitive Impairments.
Individuals who are visually impaired or have cognitive conditions such as dementia may have difficulty navigating safely. Supervised ambulation provides direction, reassurance, and prevents injury.
7. Patients on Certain Medications.
Medications such as sedatives, antihypertensives, or opioids may cause dizziness, fatigue, or orthostatic hypotension. These patients benefit from guided ambulation to reduce the risk of falls.
8. Patients in Rehabilitation Programs.
People recovering from prolonged bed rest, injury, or illness often undergo rehabilitation that includes assisted ambulation to rebuild strength, endurance, and confidence.
Assistive Devices Used in Ambulation
Several assistive devices are commonly used to support patients during ambulation. The appropriate device is determined based on the patient’s condition, strength, and balance.
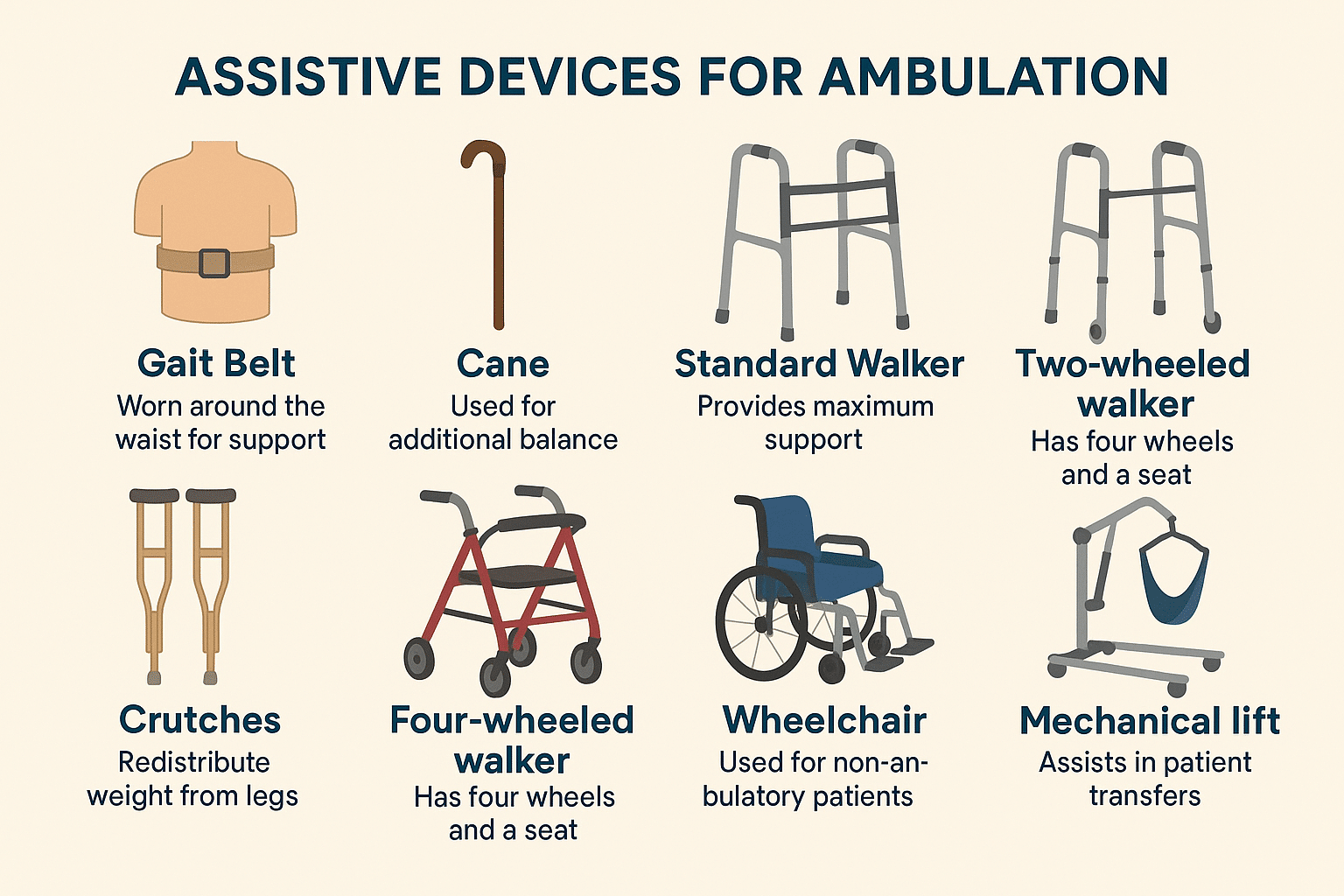
| Assistive Device | Description |
|---|---|
| Gait Belt | A strap placed around the patient’s waist to provide support and control during movement; helps the nurse maintain a secure grip and assist with balance. |
| Cane | A mobility aid used on the stronger side to offer additional balance support for slight weakness or instability. |
| Standard Walker | A sturdy frame providing maximum support; ideal for patients with significant balance or strength issues. |
| Two-Wheeled Walker (2WW) | A walker with wheels on the front legs, allowing easier forward movement while still offering support. |
| Four-Wheeled Walker (4WW) | A walker with wheels on all legs and often a seat; suited for patients with good mobility needing mild support. |
| Crutches | Typically used for patients recovering from leg injuries or surgeries; redistributes weight away from the lower limbs. |
| Wheelchair | Used for transport or for patients who cannot ambulate independently; can be used with walking sessions for rest. |
| Mechanical Lift | Used for severe immobility or high fall risk; assists in transfers and reduces caregiver strain. |
Bedside Mobility Assessment Tool (BMAT)
The Bedside Mobility Assessment Tool (BMAT) is a quick and standardized method nurses use to evaluate a patient’s mobility and determine the safest way to assist with movement. It categorizes patients into four levels based on their physical ability:
- Level 1 (Sit and Shake). Patient can sit on the edge of the bed and extend the arm to shake hands. If unable, a mechanical lift is recommended.
- Level 2 (Stretch and Point). Patient can lift one leg off the bed and point or flex the foot. If unable, use a friction-reducing device or two-person assist
- Level 3 (Stand). Patient can stand at the bedside for five seconds without assistance. If unable, consider using a walker or additional support.
- Level 4 (Walk): The patient can take a few steps with or without assistive devices. However, supervision may still be needed for safety.
| BMAT Level | Assessment Task | What the Nurse Should Do | If Patient Passes | Mobility Recommendations |
| Level 1 (Sit and Shake) | From a semi-reclined position, assist patient to sit at bedside and reach across midline to shake nurse’s hand. | Observe trunk strength, ability to follow commands, and seated balance for 2+ minutes. | Proceed to Level 2. | Use mechanical lift or total assist. If patient has bilateral non-weight-bearing or is on strict bed rest, do not proceed further. |
| Level 2 (Stretch and Point) | Ask patient to place both feet flat, stretch one leg, straighten knee, and point/flex toes. | Assess lower limb strength, control, and stability. May test one leg at a time. | Proceed to Level 3. | Use sit-to-stand lift if patient can bear weight on at least one leg. Use total lift if not. |
| Level 3 (Stand) | Ask patient to stand from seated position and hold for 5 seconds. | Observe weight-bearing on at least one leg and use of assistive devices like bedrail or cane. | Proceed to Level 4 if no device is needed. | Use non-powered or powered stand aid. If assistive device or supervision is required, remain at Level 3. |
| Level 4 (Step/Walk) | Ask patient to march in place and step forward and back at bedside. | Check for steady gait, balance, safety awareness, and turning ability. | No further levels. | Ambulate with supervision or assistive device if needed. If gait is unsteady or unsafe, revert to Level 3. |
Nursing Assessment
Before assisting with ambulation, nurses should assess the patient’s medical history, physical condition, vital signs, and readiness to ambulate. This helps provide safety, prevent complications like dizziness or falls, and determine the best time for the activity.
1. Review the patient’s chart and check for any movement or position restrictions in the physician’s orders.
Reviewing the chart helps identify any conditions or recent surgeries that could affect safe movement. This helps guide the ambulation plan to match the patient’s current clinical status.
2. Check for the presence of medical equipment such as IV lines, drains, or urinary catheters that may interfere with safe ambulation.
Awareness of attached devices helps prevent entanglement, pulling, or dislodgment during movement.
3. Assess physical readiness. Use the Bedside Mobility Assessment Tool (BMAT) as a guide.
Evaluating physical readiness helps determine whether the patient can safely participate in ambulation without risk of injury. The BMAT provides a structured, evidence-based approach to assessing mobility levels and selecting appropriate support or equipment.
4. Assess for any medication side effects, including dizziness, sedation, or unsteady gait, which could increase the risk of falls.
Certain drugs can significantly impact a patient’s balance, coordination, and awareness. For example, opioid pain relievers like morphine or hydromorphone can cause drowsiness and dizziness, while antihypertensives such as metoprolol may lead to orthostatic hypotension, increasing the risk of fainting.
5. Determine optimal time for ambulation.
Timing ambulation when the patient is well-rested and alert increases the likelihood of success. It prevents fatigue-related complications and improves participation.
6. Assess the patient’s physical size, weight, and level of mobility, as well as the nurse’s strength and ability to provide adequate support during ambulation. Consider whether additional staff or assistive equipment is needed to perform the activity safely.
Assessing the patient’s size and mobility determines the appropriate level of assistance required and helps prevent unsafe movement. Recognizing the nurse’s physical limitations and utilizing additional personnel or assistive devices when necessary supports safe and effective ambulation for both the patient and nurse.
7. Evaluate vital signs (especially BP).
Abnormal blood pressure, especially hypotension, can lead to dizziness or falls. Monitoring helps physiological stability before exertion.
8. Assess for dizziness, lightheadedness, or nausea.
Identifying symptoms like dizziness or nausea prevents ambulation-related injuries. This helps the patient feel well enough to proceed safely.
9. Prepare the following equipment
- Sphygmomanometer (BP apparatus)
- Gait belt (if needed)
- Assistive devices such as a walker, a cane, or crutches (as appropriate)
- Non-slip footwear
- Wheelchair or chair for resting, if needed
How to Assist a Patient during Ambulation
Nurses provide support and safety when assisting a patient with ambulation and monitor the patient’s response throughout the activity. The goal is to promote mobility while preventing injury or complications. The following are the steps:
1. Explain the procedure to the patient.
Explaining the purpose and steps of ambulation builds patient trust, reduces fear, and increases willingness to participate actively.
2. Check initial vital signs.
Recording pre-ambulation vitals provides a baseline to compare against later readings and helps confirm clinical readiness.
3. Assist the patient to a sitting position and dangle the feet.
Sitting with legs over the edge of the bed allows gradual adjustment in circulation, helping avoid sudden drops in blood pressure.
4. Recheck blood pressure.
A blood pressure reading significantly below normal, such as systolic below 90 mmHg or a sudden drop upon standing, is unsafe for ambulation as it may indicate orthostatic hypotension. This can lead to dizziness, fainting, or falls, so ambulation should be postponed until the patient stabilizes.
5. Ensure the patient wears appropriate, well-fitted footwear before ambulation.
Proper footwear helps prevent slips, trips, and falls during ambulation by providing adequate grip and foot support. It also promotes stability and balance, especially in patients with weakness or unsteady gait.
6. Firmly wrap the gait belt around the patient’s waist, ensuring it fits snugly but comfortably.
This allows the nurse to maintain better control and support during ambulation, helping to promote the patient’s stability and reduce the risk of falls.
7. Stand in front of the patient, securely holding both sides of the gait belt while maintaining a straight back and bending your knees.
This posture provides stability and helps the nurse lift safely, reducing the risk of injury.
8. With a slow and steady movement, guide the patient into standing while maintaining a firm grip on the gait belt.
A slow, steady movement helps the patient rise safely and prevents dizziness or sudden drops in blood pressure. Holding the gait belt firmly gives the nurse better control and supports the patient’s balance.
Ambulating a Patient with One-Nurse Assistance
1. Stand on the patient’s side and grasp the gait belt. If the patient is weak on one side, the nurse should be positioned on the weaker side for support.
Positioning on the weaker side gives the nurse better control and the ability to give direct support where it’s most needed. Holding the gait belt from behind helps stabilize the patient’s center of gravity. This approach reduces the risk of falls and promotes a safer ambulation experience.
2. Walk forward at the patient’s pace.
Walking at the patient’s natural pace prevents overexertion and anxiety. This approach maintains a steady rhythm that helps the patient feel more in control and safe throughout the ambulation.
3. If the patient has an IV pole, it should be held on the same side as the assisting nurse and guided forward during ambulation.
Holding the IV pole on the same side as the assisting nurse allows better coordination and control during ambulation. The IV pole should be used for balance assistance only, not as the main source of support.
4. Observe for weakness or dizziness and allow the patient to sit if needed.
Continuously monitoring for signs such as swaying, slowing, or verbal cues of discomfort enables early intervention. Promptly guiding the patient to sit prevents injuries and restores comfort quickly.
5. If a patient begins to fall, provide support by holding the gait belt firmly, widening the stance for stability, and guiding the descent by extending one leg and bending the knees. Let the patient slide gently to the floor in a controlled and safe manner.
This technique helps prevent injury to the patient and the nurse by safely controlling the fall. Maintaining a stable base and using proper body mechanics decreases strain and promotes a safer descent.
Ambulating a Patient with Two-Nurse Assistance
1. Stand on either side of the patient and grasp the gait belt at the back.
Standing on either side and holding the gait belt from the back provides better control and support during ambulation. This position allows the nurse to respond quickly if the patient loses balance, lessening the risk of falls.
2. Slowly guide the patient forward. Walk in unison with the patient at a steady pace.
Walking in sync with the patient guarantees consistent and smooth support. This technique lessens jarring movements and builds confidence during each step.
3. Gradually increase walking distance based on tolerance.
Starting with short distances and increasing gradually allows the body to adapt to movement. This progression strengthens endurance while avoiding fatigue or cardiovascular strain.
Post-Ambulation Care
1. After ambulating, remove the gait belt, assist the patient to a chair or bed, and provide comfort.
Helping the patient become stable and supported while sitting or lying reduces the risk of fainting or imbalance. Adding pillows or adjusting the bed height contributes to physical ease and relaxation.
2. Place the patient in a safe and comfortable position following ambulation or a fall. If resting in bed, adjust the bed to its lowest position to reduce the risk of injury from falls. Raise side rails as needed based on safety protocols, and position the call bell within easy reach.
These actions promote safety by minimizing the risk of falls and supporting patient independence. Providing access to the call bell ensures the patient can communicate needs promptly, decreasing anxiety and improving care responsiveness.
3. Offer fluids if appropriate.
Fluids can help counteract mild dehydration caused by physical activity. Encouraging small sips supports circulation and helps with recovery.
4. Remove gloves. Perform Handwashing.
Hand hygiene before and after contact protects the patient and nurse from contamination.
5. Document the procedure, including duration, distance, and patient response.
After assisting with ambulation, the nurse should document the date, time, distance ambulated, duration, and the level of assistance provided. It’s also important to record the patient’s response, any signs of fatigue, dizziness, or changes in vital signs, and whether the activity was tolerated well.
General Nursing Considerations
Nurses promote patient safety during ambulation by assessing readiness, offering support, and communicating clearly. Proper body mechanics and fostering independence help prevent injuries and support recovery.
1. Delegate ambulation to nursing assistive personnel (NAP) only if the patient is stable and the NAP is properly trained.
This promotes patient safety by confirming that the NAP can handle the situation appropriately. Clear communication and post-activity evaluation help detect issues early and guide further care.
2. Monitor for signs of fatigue.
Watching for shortness of breath, sweating, or a change in pace can signal the need to pause or terminate the ambulation. Intervening early helps protect the patient from harm.
3. Communicate clearly with the patient.
Giving calm, clear instructions supports safe movement and decreases anxiety. Open communication also reassures the patient and encourages cooperation.
4. Use proper body mechanics.
Keeping the back straight, bending the knees, and using the legs to support movement helps maintain proper body mechanics to prevent musculoskeletal injury and provide a stable support during patient ambulation.
5. Be prepared to intervene quickly.
Having a chair or support device nearby allows to respond immediately to signs of instability. Quick action prevents falls and restores the patient’s sense of safety.
6. Encourage independence when safe.
Encouraging the patient to participate in their movement builds confidence and promotes recovery. When safe, allowing patients to take the lead supports autonomy and mobility progress.
7. When assisting with a cane, place it on the patient’s stronger side. Instruct the patient to step with the stronger leg first, then move the cane and weaker leg together for better balance and coordination.
Placing the cane on the stronger side supports the weaker leg during movement. Stepping with the stronger leg first helps maintain balance and promotes a smoother, safer walking pattern.
8. Administer pain medication as prescribed for post-surgical patients before ambulation.
Pain control improves comfort and reduces hesitancy, encouraging mobility.
9. Provide assistive devices support for patients with neurological conditions such as stroke, dementia, or Parkinson’s disease.
Tailored assistance reduces fall risk and compensates for balance and coordination deficits.
10. Address fear of falling by providing reassurance and a safe environment.
Reducing fear encourages mobility and fosters patient confidence.
11. Allow for frequent rest breaks for elderly patients to prevent fatigue.
Rest periods conserve energy, enabling sustained mobility.
12. Use specialized equipment, such as crutches or walkers, to support ambulation for patients with orthopedic injuries.
Devices like crutches, walkers, or canes provide stability and compensate for limited limb function. The correct device helps lessen strain on injured areas while promoting safe movement.
13. Check the physician’s order for weight-bearing limitations for patients with orthopedic injuries (e.g., non-weight-bearing, partial, or full).
This guides how much pressure the patient can safely place on the affected limb during ambulation. Following these guidelines helps prevent further injury, supports proper healing, and ensures safe mobility.
Sources
- Kozier, B., Erb, Glenora., et al., (2018). Fundamentals of Canadian Nursing Concepts, Process, and Practice 9th Edition.
- Boynton, T. The Bedside Mobility Assessment Tool (BMAT) embedded in the new Mobility Screening and Solutions Tool (MSST): addressing inaccuracies. BMC Health Serv Res 24, 1164 (2024).
- Potter, P., et al., (2019). Essentials for Nursing Practice.
- Constantin, S., & Dahlke, S. (2018). How nurses restore and maintain mobility in hospitalised older people: An integrative literature review. International Journal of Older People Nursing, e12200.
- Costa, R. B., dos Santos, E. R., Lopes, C. T., & Bergamasco, E. C. (2015). Adequacy of the Activities in the Nursing Intervention Exercise Therapy: Ambulation for Medical-Surgical Patients With Impaired Physical Mobility. International Journal of Nursing Knowledge, 27(4), 201–204.
- King, B. J., Steege, L. M., Winsor, K., VanDenbergh, S., & Brown, C. J. (2016). Getting Patients Walking: A Pilot Study of Mobilizing Older Adult Patients via a Nurse-Driven Intervention. Journal of the American Geriatrics Society, 64(10), 2088–2094.
- King, B., Bodden, J., Steege, L., & Brown, C. J. (2020). Older adults experiences with ambulation during a hospital stay: A qualitative study. Geriatric Nursing.
- Sepulveda-Pacsi, A. L., Soderman, M., & Kertesz, L. (2016). Nurses’ perceptions of their knowledge and barriers to ambulating hospitalized patients in acute settings. Applied Nursing Research, 32, 117–121.
- Yager, M., & Stichler, J. (2015). The Effect of Early Ambulation on Patient Outcomes for Total Joint Replacement. Orthopaedic Nursing, 34(4), 197–200.





























Leave a Comment