Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity that significantly impact daily functioning. It is one of the most common behavioral disorders affecting children, and symptoms often persist into adolescence and adulthood.
ADHD can present challenges in academic, social, and familial domains, leading to difficulties in concentration, organization, and impulse control.
What is Attention Deficit Hyperactivity Disorder (ADHD)?
- Attention-deficit/hyperactivity disorder (ADHD). ADHD is a brain disorder marked by an ongoing pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development.
- Inattention. Inattention means a person wanders off task, lacks persistence, has difficulty sustaining focus, and is disorganized; and these problems are not due to defiance or lack of comprehension.
- Hyperactivity. Hyperactivity means a person seems to move about constantly, including in situations in which it is not appropriate; or excessively fidgets, taps, or talks.
- Impulsivity. Impulsivity means a person makes hasty actions that occur in the moment without first thinking about them and that may have high potential for harm; or a desire for immediate rewards or inability to delay gratification.
Pathophysiology
Both genetic and environmental factors contribute to ADHD, “nature and nurture.”
- The neurotransmitters dopamine (DA) and norepinephrine (NE) are implicated in the pathophysiology of ADHD; dopamine is a neurotransmitter involved in reward, risk taking, impulsivity, and mood; norepinephrine modulates attention, arousal and mood.
- Brain studies on individuals with ADHD suggest a defect in the dopamine receptor D4 (DRD4) receptor gene and overexpression of dopamine transporter-1 (DAT1).
- The DRD4 receptor uses DA and NE to modulate attention to and responses to one’s environment.
- The DAT1 or dopamine transporter protein takes DA/NE into the presynaptic nerve terminal so it may not have sufficient interaction with the postsynaptic receptor.
- The implications of these limited receptor findings require further study, however, it seems clear that dopamine and norepinephrine are involved in the pathophysiology of ADHD.
Statistics and Incidences
ADHD is a valid diagnosis that affects 3% to 5% of school age children and may persist into adulthood.
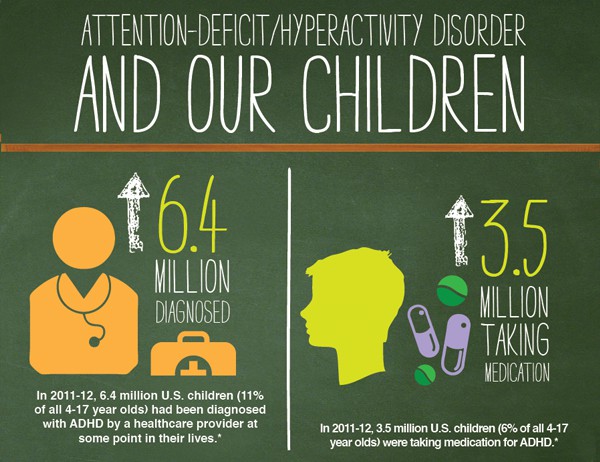
- ADHD incidence rates are 5 to 10 times greater in the United States compared with other countries.
- 8% to 10% of 30,000 children in second to fifth grade were diagnosed with ADHD in 1 Virginia school system whereas the NIH reports a lower 3% to 5% incidence.
- Cultural differences in prescribing stimulants were reported in the same study; by fifth grade, 18% to 20% of white boys were prescribed methylphenidate whereas rates were significantly lower in other ethnicities.
- One study of treatment services for ADHD nationwide found that only 50% of children with identified ADHD in real-world practice settings receive care that corresponds to guidelines of the American Academy of Child and Adolescent Psychiatry.
Causes
The cause of the disorder is unclear: developmental lag, biochemical disorders, and food sensitivities are all theories under consideration.
- Developmental lag. Children with ADHD experience a developmental delay in areas of the brain important for controlling action and attention.
- Biochemical changes. A new study at Örebro University in Sweden shows that children with ADHD have nearly 50 percent less of a protein that is important for attention and learning; the finding may mean that there are other biochemical disturbances in the brains of individuals with ADHD than was previously believed.
- Food sensitivities. Dietary studies have found a strong connection between food and ADHD symptoms, these studies are small and have their limitations, as most nutrition studies do, but they all produce remarkable results.
Clinical Manifestations
The child with ADHD may have these characteristics:
- Inattention. You might not notice it until a child goes to school; in adults, it may be easier to notice at work or in social situations; the person might procrastinate, not complete tasks like homework or chores, or frequently move from one uncompleted activity to another.
- Hyperactivity. Children with hyperactivity may fidget and squirm when seated; get up frequently to walk or run around; have trouble playing quietly or doing quiet hobbies; and talk excessively.
- Impulsivity. Symptoms of this include impatience, having a hard time waiting to talk or react, and frequently interrupt or intrude on others.
Complications
ADHD doesn’t cause other psychological or developmental problems; however, children with ADHD are more likely than others to also have conditions such as:
- Tourette syndrome. A neurological disorder characterized by repetitive muscle or vocal tics.
- Depression. Depression frequently occurs in children with ADHD.
- Oppositional defiant disorder (ODD). Generally defined as a pattern of negative, defiant and hostile behavior toward authority figures.
- Bipolar disorder. Bipolar disorder includes depression as well as manic behavior.
- Conduct disorder. This is marked by antisocial behavior such as stealing, fighting, destroying property, and harming people or animals
- Anxiety disorders. Anxiety disorder may cause overwhelming worry, nervousness.
Assessment and Diagnostic Findings
Diagnosis can be made after the child is three (3) years old but often is not made until the child reaches school age and has trouble settling into the routine of being in the classroom setting.
- Medical examination. Medical examination may help rule out other possible causes of symptoms.
- ADHD criteria from the Diagnostic and Statistical Manual of Mental Disorders. DSM-5, published by the American Psychiatric Association, has a list of the criteria that confirms the diagnosis of ADHD.
- ADHD rating scales. The ADHD Rating Scale is a parent-report or teacher-report inventory created by DuPaul and colleagues consisting of 18 questions regarding a child’s behavior over the past 6 months.
Medical Management
The therapeutic approach to ADHD has been shifting.
- Behavioral psychotherapy. Behavioral psychotherapy often is effective when used in combination with an effective medication regimen; behavioral therapy or modification programs can help diminish uncertain expectations and increase organization.
- Psychosocial interventions. A number of psychosocial treatments are effective; these include behavioral parent training (BPT) and behavioral classroom management (BCM);these are best used in conjunction with psychopharmacological approaches.
- Cognitive therapy for adults with ADHD. Metacognitive therapy involves the principles and techniques of cognitive and behavioral therapies to enhance time management; in doing so, these have made adult patients with ADHD better able to counter the anxiety and depressive symptoms they experience in task performance.
Pharmacologic Therapy
Medication is used for some children; the medications of choice are stimulants, and for adults with ADHD stimulants represent the best first-line therapeutic option.
- Stimulants. Stimulant medications, such as methylphenidate (Ritalin, Concerta) and dextroamphetamine (Dexedrine), have often been used; when given in large amounts, these medications may suppress the appetite and affect the child’s growth.
- Atomoxetine. Atomoxetine (Strattera) has become a second-line and, in some cases, first-line treatment in children and adults with ADHD because of its efficacy and classification as a nonstimulant.
- Tricyclic antidepressants. Tricyclic antidepressants (imipramine, desipramine, nortriptyline) have been found effective in numerous studies in children with ADHD; however, because of potential adverse effects, they are rarely used for this purpose.
- Modafinil. Modafinil (Provigil) has recent placebo-controlled data supporting its efficacy in children with ADHD; this medication may currently be used as a third- or fourth-line treatment.
Nursing Management
Nurses must be knowledgeable enough in taking care of patients with ADHD; environmental and behavioral settings should be taken into consideration.
Nursing Assessment
Assessment of ADHD typically involves the comprehensive evaluation of information gathered from a number of sources, including parents/carers, family members, teachers, partners and colleagues, depending on the age of the patient.
- Clinical examination. Clinical examination aims to identify the presence of other illnesses with symptoms that overlap with those of ADHD; this typically involves inspections for vision or hearing impairments, neurodevelopmental immaturity in relation to gross and fine motor functions and motor or vocal tics, and retardation.
- Interview. A healthcare professional will interview the person with suspected ADHD along with any relevant family members, carers, partners, teachers, employers or friends, to ascertain observations of symptoms/behaviours in different settings, developmental, medical and psychiatric history, and patterns of ADHD or related comorbidities present in the family.
- Observations. For children and adolescents, teachers in particular may be especially well placed to identify symptoms of ADHD in children and support symptom reports from parents.
- Rating scales. A number of rating scales are available to help assess general behaviour and psychosocial functioning, ADHD symptomatology and comorbidities.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses appropriate for the patient are:
- Defensive coping related to feelings of inadequacy and need for acceptance from others.
- Impaired social interaction related to developmental disabilities (hyperactivity).
- Altered thought processes related to personality disorders.
- Risk for parental role conflict related to children with attention deficit hyperactivity disorder.
- Risk for injury related to psychological (orientation ineffective).
- Risk for delay in growth and development related to mental illness (hyperactivity), lack of concentration.
Nursing Care Planning and Goals
The major goals for a patient with ADHD are:
- Implement appropriate memory retraining techniques, such as keeping calendar, writing list, memory cue games, mnemonic device using computers, and so forth.
- Encourage ventilation of feelings of frustration helplessness, and so forth.Refocus attention to areas of control and progress.
- Provide for / emphasize importance of pacing learning activities and having appropriate rest.
- Monitor client’s behavior and assist in using stress management techniques.
Nursing Interventions
The nurse’s role in caring for the patient with ADHD involves the following interventions:
- Accept the child or individual as what he is. Consider his condition and communicate with him as an equal.
- Approach the child at his current level of functioning. Do not use baby talk nor direct him as to his chronological age; encourage him to express his thoughts or emotions and respond to him therapeutically.
- Use simple and direct instructions. You may repeat your instructions more than once and at times, you may utilize visual aids or pictures in order for him to relate well; in educating the child, the lessons should only be brief in duration due to his short attention span.
- Implement scheduled routine every day. Make his routine predictable and something like ritualistic so that it will only be easy for him to grasp for his independent functioning.
- Avoid stimulating or distracting settings. Ensure to involve the child in his daily activities in a quiet and non-stimulating area to prevent him from becoming easily distracted and hyperactive.
- Give positive reinforcements. Every good deed done should be rewarded even with a simple smile, nod or a star’ praise him for achieving his goals for the day or a task that was finished; it is also advisable to provide immediate reinforcement since they sometimes have decrease tolerance to frustration.
- Encourage physical activity. You may encourage him to join a physical activity that he likes as this may also help him make friends with other children; allow him to exert his energy productively but do not let him get over fatigued, too; physical activity helps in getting good sleep but over fatigue might as well make him uneasy and irritable.
Evaluation
After implementation of the care plan, the result of the evaluation should include:
- Implemented appropriate memory retraining techniques, such as keeping calendar, writing list, memory cue games, mnemonic device using computers, and so forth.
- Encouraged ventilation of feelings of frustration helplessness, and so forth; refocused attention to areas of control and progress.
- Provided for / emphasized importance of pacing learning activities and having appropriate rest.
- Monitored client’s behavior and assist in using stress management techniques.
Discharge and Home Care Guidelines
Care for a child with ADHD at home includes:
- Help the child build self-esteem. Encourage a sense of belonging, confidence in learning, and an awareness of his or her own contributions.
- Help the child get the most out of school. Promoting school success will help the child academically, socially, and developmentally.
- Help the child get things done. Patience, persistence, and creative thinking can help the child learn skills and accomplish tasks at home and at school.


























Leave a Comment