Strabismus, commonly known as “crossed eyes” or “squint,” is a prevalent ophthalmological condition characterized by an abnormal misalignment of the eyes. This ocular disorder affects millions of individuals worldwide, irrespective of age or gender, and has significant implications for vision and quality of life. In this article, we delve into the multifaceted aspects of strabismus, exploring its causes, assessment techniques, and contemporary management strategies.
What is Strabismus?
- Strabismus is the inward deviation of the eyes noted before the patient reaches age six (6) months.
- It is associated with the maldevelopment of stereopsis, motion processing, and eye movements.
- It is a visual problem in which the eyes are not aligned properly and point in different directions.
- To date, its exact cause has yet to be identified, and an effective treatment strategy is yet to be formulated.
Pathophysiology
The exact cause of strabismus remains unknown.
- Worth strongly believed that esotropia is an inborn and irreversible defect of fusion.
- As such, it is a primary dysfunction in the normal development of binocular sensitivity.
- This was countered by Chavasse who asserted that the neural components necessary for normal binocular vision are present in strabismic individuals at birth, but the development of fusion is eventually impeded by abnormalities of optical input (eg, monocular cataracts) or muscular output (eg, cranial nerve palsies).
- A few authors have implicated practically everything from and between the extraocular muscles to the visual cortex in the causation of strabismus.
- Although understanding the mechanisms behind strabismus has come a long way, there is still a lot of ground to cover to unearth and clearly understand such an elusive condition.
Statistics and Incidences
The incidence of strabismus in the United States and all over the world are as follows:
- Strabismus is one of the most prevalent ocular problems among children, affecting 5 in every 100 US citizens, or some 12 million people in a population of 245 million.
- A population-based study from 1965 to 1994 reports the birth prevalence of strabismus to be 25 per 10,000 or 1 in 403 live births.
- In an attempt to determine whether esotropia is present at birth or develops later in infancy, Nixon et al observed 1,219 alert infants in a normal newborn nursery at a city hospital and noted that only 40 babies (3.2%) had esotropia (intermittent esotropia in 17 patients, with 14 patients varying between esotropia and exotropia, and 9 patients with variable esotropia).
- Greenberg et al reported an annual age- and gender-adjusted childhood strabismus incidence of 111 per 100,000 patients younger than 19 years.
- By definition, strabismus is seen in infants before age 6 months.
Causes
The exact cause of strabismus has yet to be identified distinctively.
- Genetics. Tychsen and Lisberger reported in 1986 that the strabismic patient who had the most severe pursuit/motion processing asymmetry had two (2) siblings with strabismus.
- Loci susceptibility. On the other hand, there is a suggested relationship of nonsyndromic strabismus to the susceptibility loci on regions 3p26.3-26.2 and 6q24.2-25.1 and may share alleles that underlie Duane retraction syndrome.

Clinical Manifestations
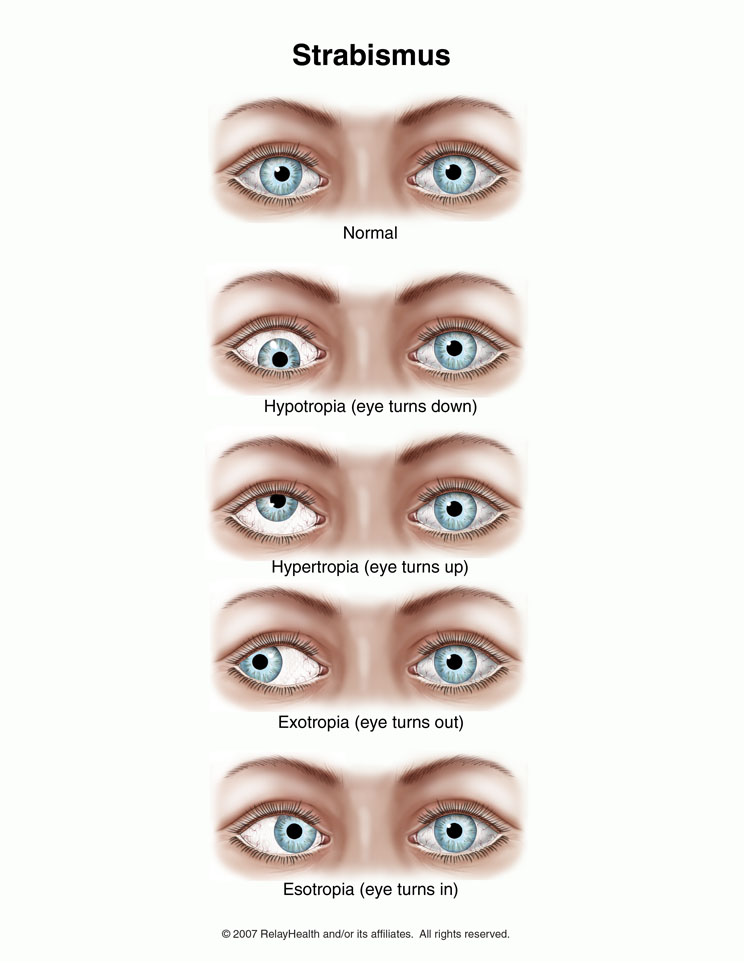
According to Tychsen, strabismus manifest with a constellation of ocular motor signs, as follows:
- Esotropia. Esotropia is in-turning of one or both eyes; it may be intermittent or constant and may occur with near fixation, distance fixation, or both.
- Pursuit asymmetry. Horizontal smooth pursuit develops for targets moving in a temporal to nasal direction before pursuit movements in a nasal to temporal direction develop; this developmental lag in nasally directed smooth pursuit is called smooth pursuit asymmetry and is only seen under monocular conditions with one eye covered.
- Latent fixation nystagmus. Latent nystagmus is a horizontal binocular oscillation that is evoked by unequal visual input to the 2 eyes; it develops primarily in humans with congenital esotropia.
- Amblyopia. Amblyopia is relatively common in patients with strabismus; Weakley et al stated that amblyopia should be suspected strongly in patients with esotropia and asymmetric inferior oblique activity, specifically in the eye with more inferior oblique overaction.
Assessment and Diagnostic Findings
Procedures to diagnose strabismus include the following:
- Alternate prism cover test. Perform the alternate prism cover test to accurately measure the angle of strabismus; this procedure gauges the full magnitude of any combined esotropia and esophoria.
Medical Management
Smaller angles of deviation may be addressed with prism lenses with or without occlusion therapy, depending on the existence of amblyopia.

- Cycloplegia. A common cycloplegic combination is 2.5% phenylephrine and 1% cyclopentolate; it is necessary to occlude one eye at a time during retinoscopy to make sure that the examiner maintains accurate alignment with the visual axis.
- Corrective lenses. Corrective lenses generally are prescribed with hyperopia greater than +2.50 diopter (D) and/or when anisometropia exceeds 1.50 D; in addition, any cylinder greater than or equal to +0.50 D should be given spectacles; on the other hand, myopia above -4.00 D warrants corrective lenses.
- Occlusion therapy. The rule of thumb observed is 1-2 weeks of high percentage (eg, 90% of waking hours) occlusion of the non- amblyopic eye per year of life, especially if a strong fixation preference for one eye is detected; the infant is reexamined after a few weeks to determine response to therapy and to ensure that occlusion-induced amblyopia has not developed in the occluded dominant eye.
- BOTOX. Botulinum toxin (BOTOX®) injection into the medial rectus has been explored as an alternative therapy to surgery; several studies have investigated the merits of such a procedure with contrasting results.
Pharmacologic Management
Very few medications are used in the treatment of strabismus; combination antibiotic-steroid ointments are prescribed for the first postoperative week. BOTOX® injection has been used as an alternative to initial or repeat surgical ocular alignment.
- Combination antibiotic-steroid ointments. Used in the first postoperative week to control any inflammation and to prevent any infection resulting from surgery, particularly in the conjunctiva.
- Neurotoxins. Botulinum toxin type A (BOTOX®) is most commonly used; inhibits transmission of nerve impulses in neuromuscular tissue.
Nursing Management
Nursing care for a child with strabismus include:
Nursing Assessment
Assessment of a child with strabismus include the following:
- History. Certain risk factors have been associated with strabismus; significant among these are prematurity, family history or secondary ocular history, perinatal or gestational complications, systemic disorders, use of supplemental oxygen as a neonate, use of systemic medications, and male sex.
- Physical exam. Strabismus may be associated with a spectrum of clinical presentations, including amblyopia, impaired binocularity, central scotomas, and incomitance.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Risk for injury related to impaired sensory function.
- Disturbed sensory perception related to structural damage.
- Knowledge deficit related to impaired vision.
- Social isolation related to the limited ability to participate in diversion activities and social activities secondary to impaired vision.
Nursing Care Planning and Goals
The major nursing care planning goals for patients with strabismus are:
- Patient will be free from injury.
- Patient will have a restored, functioning sensory perception.
- Patient and/or folks will have an understanding of the condition, the treatment, and surgery.
- Patient will be able to interact socially with others.
Nursing Interventions
Nursing interventions for a child with strabismus include the following:
- Prevent injury. Thoroughly conform patient to surroundings; put call light within reach and teach how to call for assistance; respond to call light immediately; place an injury-prone patient in a room that is near the nurses’ station; educate patient about safety ambulation at home, including the use of safety measures such as handrails in bathroom; for patients with visual impairment, educate him or caregiver to label with bright colors such as yellow or red significant places in environment that must be easily located (e.g., stair edges, stove controls, light switches).
- Patch therapy and vision therapy. In patch therapy, the child’s stronger eye is covered with a patch, forcing the weaker eye to function at a higher level; vision therapy consists of exercises performed in the eye doctor’s office under supervision to change the way the eyes process visual information; it is not concerned with strengthening the eye muscles.
- Enforce the caregiver’s knowledge. Observe and note existing misconceptions regarding material to be taught; acknowledge racial/ethnic differences at the onset of care; consider the patient’s/caregiver’s learning style, especially if the patient/caregiver has learned and retained new information in the past; include the patient/caregiver in creating the teaching plan, beginning with establishing objectives and goals for learning at the beginning of the session; provide clear, thorough, and understandable explanations and demonstrations.
Evaluation
Goals are met as evidenced by:
- Patient will be free from injury.
- Patient will have a restored, functioning sensory perception.
- Patient and/or folks will have an understanding of the condition, the treatment, and surgery.
- Patient will be able to interact socially with others.
Documentation Guidelines
- Baseline and subsequent assessment findings to include signs and symptoms.
- Individual cultural or religious restrictions and personal preferences.
- Plan of care and persons involved.
- Teaching plan.
- Client’s responses to teachings, interventions, and actions performed.
- Attainment or progress toward the desired outcome.
- Long-term needs, and who is responsible for actions to be taken.
































Leave a Comment