Hydrocele is a common and generally benign condition characterized by the accumulation of fluid in the sac surrounding the testicles (the tunica vaginalis). This results in a painless swelling or enlargement of the scrotum, often affecting males of all ages, but more commonly found in newborns and older men.
Hydroceles can be classified as either communicating or non-communicating, depending on whether there is a connection between the tunica vaginalis and the abdominal cavity. While most hydroceles are not harmful, they may cause discomfort or cosmetic concerns.
What is Hydrocele?
A few of the genitourinary conditions may affect the infant in the first year of life.
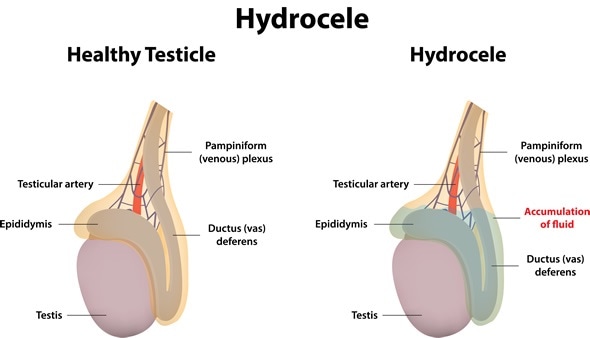
- A hydrocele is a collection of peritoneal fluid that accumulates in the scrotum through a small passage called the processus vaginalis.
- This processus is a finger-like projection in the inguinal canal through which the testes descend.
- A hydrocele is a fluid collection within the tunica vaginalis of the scrotum or along the spermatic cord.
- These fluid collections may represent persistent developmental connections along the spermatic cord or an imbalance of fluid production versus absorption.
- The description of the abdominal cavity parietes to the tunica vaginalis is attributed to Galen in 176 AD; however, the clear description of the inguinal anatomy and its relationship to groin hernias and hydroceles was not recorded until the 19th century.
Pathophysiology
The pathophysiology of hydroceles requires an imbalance of scrotal fluid production and absorption; this imbalance can be divided further into exogenous fluid sources or intrinsic fluid production.
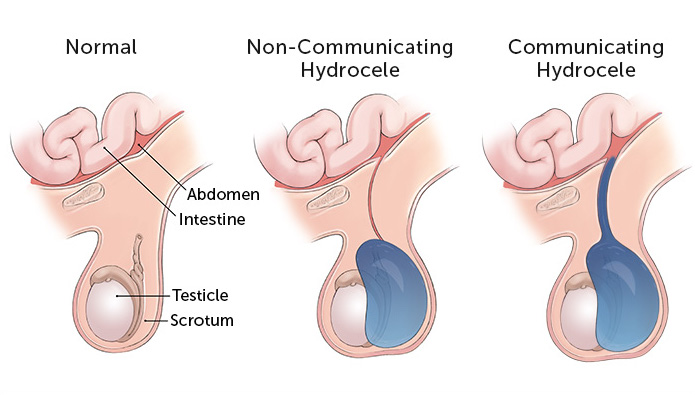
- Alternatively, hydroceles can be divided into those that represent persistent communication with the abdominal cavity and those that do not.
- Fluid excesses are from exogenous sources (the abdomen) in communicating hydroceles, whereas noncommunicating hydroceles develop increased scrotal fluid from abnormal intrinsic scrotal fluid shifts.
- With communicating hydroceles, simple Valsalva maneuvers probably account for the classic variation in size during day-sleep cycles.
- Noncommunicating hydroceles may result from increased fluid production or impaired fluid absorption.
- Sudden onset of scrotal hydrocele in older children has been noted after viral illnesses; in such cases, viral-mediated serositis may account for the net increased fluid production.
- Posttraumatic hydroceles likely occur secondary to increased serosal fluid production due to underlying inflammation.
- Although rare in the United States, filarial infestations are a classic cause of decreased lymphatic fluid absorption resulting in hydroceles.
Statistics and Incidences
In endemic tropical regions, scrotal hydrocele may occur in males of any age as a result of filariasis, especially from Wuchereria bancrofti infection.
- A patent processus vaginalis is found in 80-90% of term male infants at birth.
- This frequency rate steadily decreases until age 2 years, at which point it appears to plateau at approximately 25-40%.
- Indeed, autopsy series of men have identified a frequency rate of 20% of the processus vaginalis remaining patent until late in life.
- However, clinically apparent scrotal hydroceles are evident in only 6% of term males beyond the newborn period.
- The incidence of hydroceles in men is less well known.
Causes
The causes of hydroceles are legion.
- Patency of processus vaginalis. In children, most hydroceles are of the communicating type, in which patency of the processus vaginalis allows peritoneal fluid to flow into the scrotum, particularly during Valsalva maneuvers.
- Infection. In the adult population, filariasis, a parasitic infection caused by Wuchereria bancrofti, accounts for most causes of hydroceles worldwide, affecting more than 120 million people in more than 73 countries.
- Iatrogenic causes. Following laparoscopic or transplant surgery in males, inadequate irrigation fluid aspiration may cause hydroceles in patients with a patent processus vaginalis or a small hernia.
Clinical Manifestations
Hydroceles typically manifest as the following:
- Palpable fullness. Hydroceles typically manifest as a soft nontender fullness within the hemiscrotum.
- Transillumination. When the scrotum is investigated with a focused beam of light, the scrotum transilluminates, revealing a homogeneous glow without internal shadows.
- Swelling. Hydroceles of the canal of Nuck in female patients typically present as soft, nontender inguinal or labial swelling.
Assessment and Diagnostic Findings
Simple hydroceles are diagnosed on clinical grounds.
- Laboratory studies. Few laboratory tests, if any, are warranted specifically for simple hydroceles, communicating or noncommunicating; concomitant medical conditions may be indications for preoperative laboratory studies; laboratory studies may be indicated to exclude other surgical or medical conditions that may be in the differential diagnosis.
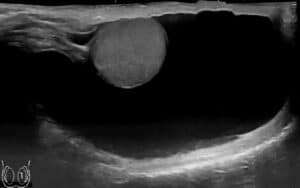
- Ultrasonography. Ultrasonography provides excellent detail of the testicular parenchyma; spermatoceles can be clearly distinguished from hydroceles on sonograms; if a testicular tumor is a diagnostic consideration, ultrasonography is an excellent screening study.
- Duplex ultrasonography. Duplex studies may provide substantial information regarding testicular blood flow when a hydrocele may be associated with chronic torsion.
- Plain abdominal radiography. Plain radiography may be useful for distinguishing an acute hydrocele from an incarcerated hernia; gas overlying the groin may indicate an incarcerated hernia.
Surgical Management
Surgical therapy can be divided into three approaches: inguinal, scrotal, and sclerotherapy.
- Inguinal. The inguinal approach, with ligation of the processus vaginalis high within the internal inguinal ring, is the procedure of choice for pediatric hydroceles; if a testicular tumor is identified on testicular ultrasonography, an inguinal approach with high control/ligation of the cord structures is mandated.
- Scrotal. The scrotal approach, with excision or eversion and suturing of the tunica vaginalis, is recommended for chronic noncommunicating hydroceles; this approach should be avoided upon any suspicion for underlying malignancy.
- Sclerotherapy. An additional adjunctive, if not definitive, procedure, is scrotal aspiration and sclerotherapy of the hemiscrotum using tetracycline or doxycycline solutions; recurrence after sclerotherapy is common, as is significant pain and epididymal obstruction, making this treatment a last resort in poor surgical candidates with symptomatic hydroceles and in men in whom fertility is no longer an issue.
Nursing Management
Nursing care management for a patient with hydrocele includes the following:
Nursing Assessment
Assessment of a child with hydrocele includes:
- Physical examination. The scrotum is enlarged on both sides; a smooth, cystic feeling mass completely surrounding the testicle and not involving the spermatic cord is characteristic of a hydrocele.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Excess fluid volume related to the collection of fluid in the scrotal sac.
- Acute pain related to the presence of postoperative wound.
- Risk for infection related to surgical incision.
- Impaired urinary elimination related to postoperative wound.
- Fear/Anxiety related to the surgical procedure.
Nursing Care Planning and Goals
Nursing care planning and goals for a patient with hydrocele includes:
- The patient or the caregivers will be able to acknowledge feelings and identify healthy ways to deal with them.
- The patient will be able to appear relaxed, and is able to rest/sleep appropriately.
- The caregivers will be able to identify individual risk factors and interventions to reduce potential for infection.
- The caregivers will be able to maintain safe aseptic environment for the child.
- The patient will be able to demonstrate adequate fluid balance, as evidenced by stable vital signs, palpable pulses of good quality, normal skin turgor, moist mucous membranes, and individually appropriate urinary output.
- The patient will be able to report relief from pain.
- The patient’s wound will be able to achieve timely healing.
Nursing Interventions
The nursing interventions appropriate for the child are:
- Health education. Provide preoperative education, including visit with OR personnel before surgery when possible; discuss anticipated things that may concern patient: masks, lights, IVs, BP cuff, electrodes, bovie pad, feel of oxygen cannula or mask on nose or face, autoclave and suction noises, child crying.
- Reduce risk for infection. Verify that preoperative skin, vaginal, and bowel cleansing procedures have been done as needed depending on specific surgical procedure; apply sterile dressing to prevent environmental contamination of fresh wound; and administer antibiotics as indicated.
- Monitor fluid volume. Measure and record I&O (including tubes and drains); monitor vital signs noting changes in blood pressure, heart rate and rhythm, and respirations; and resume oral intake gradually as indicated.
- Relief from pain. Evaluate pain regularly (every 2 hrs noting characteristics, location, and intensity (0–10 scale); note presence of anxiety or fear, and relate with nature of and preparation for procedure; assess causes of possible discomfort other than operative procedure; and provide additional comfort measures: backrub, heat or cold applications.
Evaluation
Goals are met as evidenced by:
- The patient or the caregivers acknowledged their feelings and identified healthy ways to deal with them.
- The patient appeared relaxed, and is able to rest/sleep appropriately.
- The caregivers identified individual risk factors and interventions to reduce potential for infection.
- The caregivers maintained a safe aseptic environment for the child.
- The patient demonstrated adequate fluid balance, as evidenced by stable vital signs, palpable pulses of good quality, normal skin turgor, moist mucous membranes, and individually appropriate urinary output.
- The patient reported relief from pain.
- The patient’s wound achieved timely healing.
Documentation Guidelines
Documentation in a patient with hydrocele should involve:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Intake and output.
- Signs of infection.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcome.
































Leave a Comment