Enterobiasis (also called pinworm, seatworm, or threadworm infection) is a prevalent and highly contagious parasitic infestation caused by the nematode Enterobius vermicularis. This parasitic worm primarily affects the human gastrointestinal tract, particularly the large intestine and rectum. Pinworm infection is most common in children and is often transmitted through the ingestion or inhalation of pinworm eggs.
This nursing note provides an overview of enterobiasis, exploring its transmission, clinical features, diagnostic approaches, medical and nursing management, and the importance of practicing good hygiene and preventive measures to control and prevent its spread in communities and households.
What is Enterobiasis?

- Enterobius vermicularis is a small nematode. This common helminthic infestation has an estimated prevalence of 40 million infected individuals in the United States.
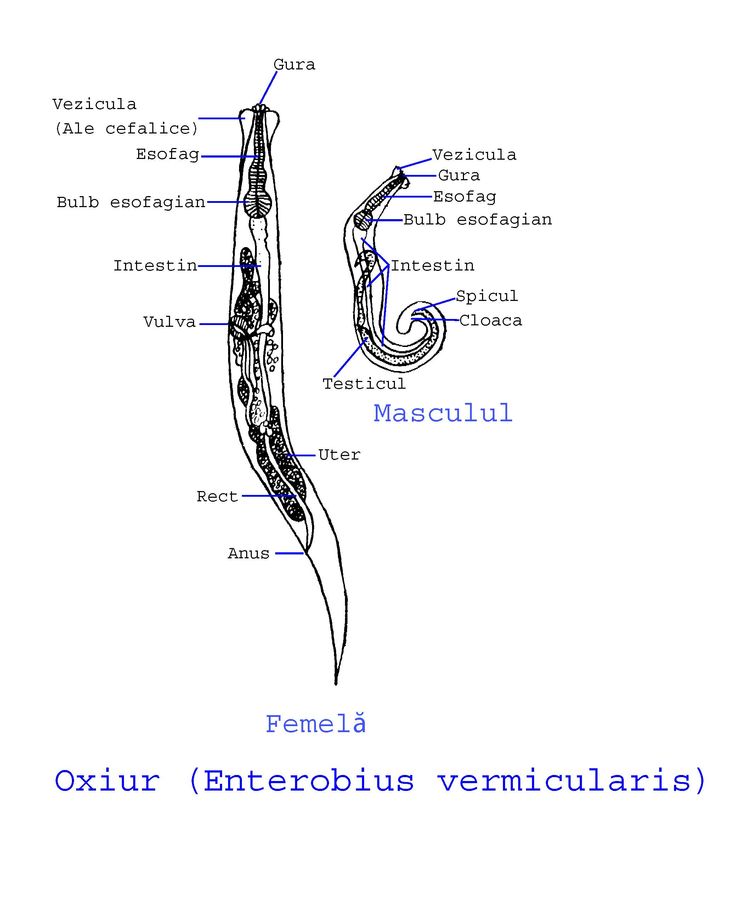
- The pinworm is a white thread-like worm that invades the cecum and may enter the appendix.
- The female nematode averages 10 mm X 0.7 mm, whereas males are smaller.
- Article contaminated with pinworm eggs spread pinworms from person to person.
- All socioeconomic levels are affected; infestation often occurs in family clusters. The infestation does not equate with poor home sanitary measures (an important point when discussing therapy).
Pathophysiology
The life cycle of these worms is 6 to 8 weeks, after which reinfestation commonly occurs without treatment.
- E. vermicularis is an obligate parasite; humans are the only natural host.
- Fecal-oral contamination via hand-mouth contact or via fomites (toys, clothes) are common methods of infestation.
- After ingestion, eggs usually hatch in the duodenum within 6 hours.
- Worms mature in as little as 2 weeks and have a lifespan of approximately 2 months.
- Adult worms normally inhabit the terminal ileum, cecum, vermiform appendix, and proximal ascending colon; the worms live free in the intestinal lumen.
- The female worm migrates to the rectum after copulation and, if not expelled during defecation, migrates to the perineum (often at night) where an average of 11,000 eggs are released.
- Eggs become infectious within 6-8 hours and, under optimum conditions, remain infectious in the environment for as long as 3 weeks.
Statistics and Incidences
The incidence of enterobiasis is highest in school-age children and next highest in preschoolers.
- Prevalence is approximately 5-15% in the general population; however, this rate has declined in recent years; prevalence rates are probably higher in institutionalized individuals; humans are the only known host.
- Infestation rate increases with increased population density, and with personal habits such as thumb sucking.
- E. vermicularis infestation occurs worldwide. Prevalence data vary by country.
- A study that aimed to determine the extent of enterobiasis, strongyloidiasis, and other helminth infections in infants, preschool-aged, and school-aged children from rural coastal Tanzania reported that Enterobius vermicularis infections were found in 4.2% of infants, 16.7%, of preschool-aged children, and 26.3% of school-aged children.
- Secondary bacterial skin infection may develop from vigorous scratching to relieve pruritus.
- The people most likely to be infected with pinworms are children younger than 18 years, people who take care of infected children, and people who are institutionalized; in these groups, the prevalence can reach 50%.
Clinical Manifestations
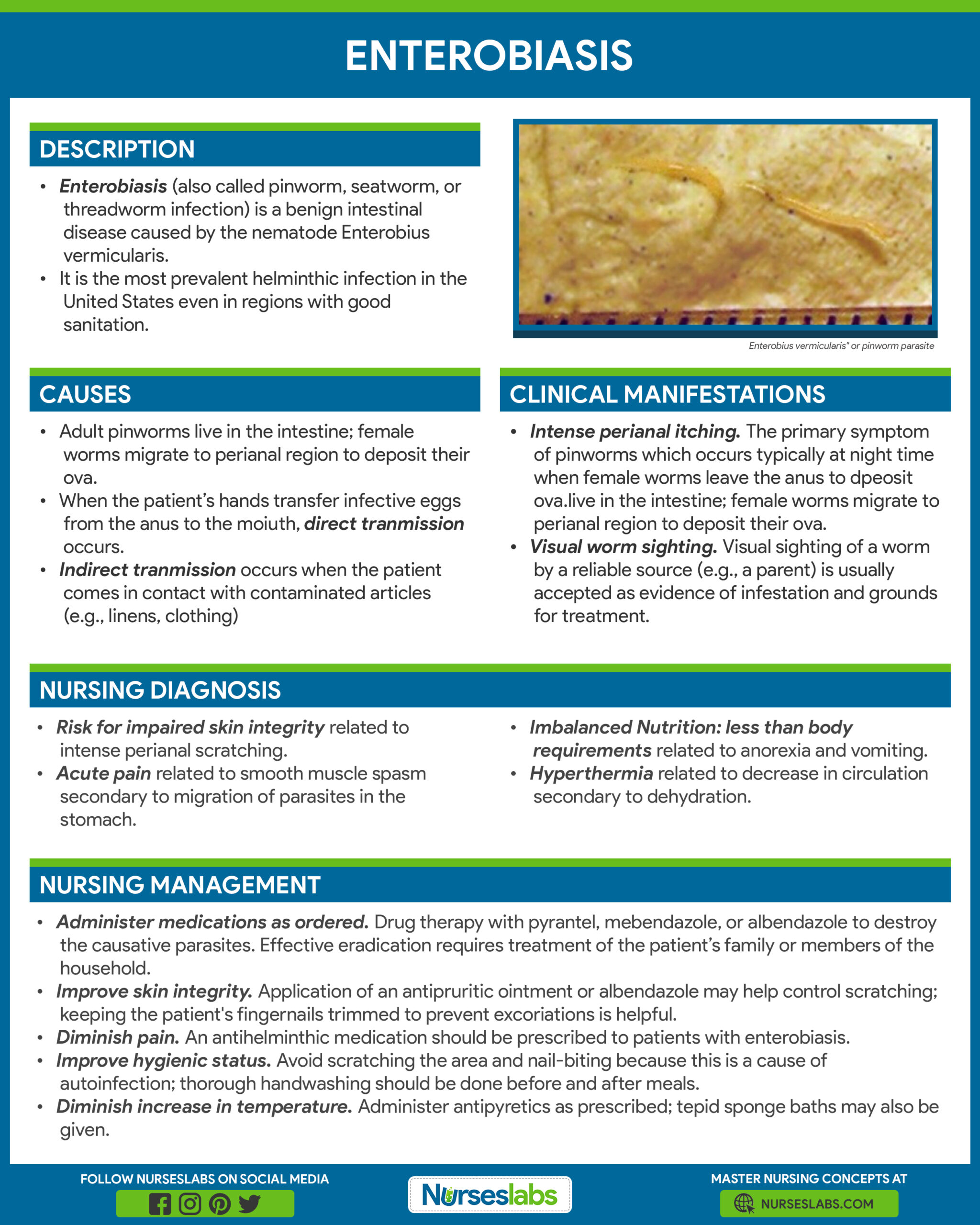
Symptoms of enterobiasis in children include:
- Perianal itching. Intense perianal itching is the primary symptom of pinworms. This occurs especially at night when the female worm leaves the anus to deposit ova.
- Erythema. Patients often have excoriation or erythema of the perineum, vulvae, or both, but infestation can occur without these signs.
- Abdominal pain. Abdominal pain may sometimes be severe and can mimic acute appendicitis.
- Visual worm sighting. Visual sighting of a worm by a reliable source (e.g., a parent) is usually accepted as evidence of infestation and grounds for treatment.
Assessment and Diagnostic Findings

The usual method of diagnosis is to use cellophane tape to capture the eggs from around the anus.
- Cellophane tape test. The cellophane tape test for identifying worms is performed in the early morning, just before or as soon as the child wakens; the tape is then examined microscopically for eggs in the laboratory.
Medical Management
Treatment of enterobiasis consists of the following:
- Handwashing. Thorough and regular handwashing is effective in preventing disease transmission.
- Personal hygiene. Changing personal habits such as thumb-sucking or nail-biting may reduce re-infection; The child should also be encouraged to observe other hygiene measures, such as regular bathing and daily change of underclothing; the nurse should teach caregivers to keep the child’s fingernails short and clean.
Pharmacologic Management
Drug therapy with pyrantel, mebendazole, or albendazole is the current standard in treating enterobiasis:
- Anthelmintics. Mebendazole is not currently available in the United States; Pyrantel pamoate or albendazole (not currently approved for this use by the US Food and Drug Administration) are recommended alternatives; a second dose given 2 weeks after the initial dose is recommended. Parasite biochemical pathways are different from the human host, thus toxicity is directed to the parasite, egg, or larvae. Mechanism of action varies within the drug class.
- Anal albendazole. Anal albendazole may help with symptoms of pruritus ani.
Nursing Management
Nursing care for a child with enterobiasis include the following:
Nursing Assessment
Assessment includes the following:
- History. Patients with enterobiasis are often asymptomatic. Worms may be incidentally discovered when they are seen in the perineal region; if patients are symptomatic, pruritus ani and pruritus vulvae are common presenting symptoms.
- Physical exam. Worms can be found in stools or on the patient’s perineum before bathing in the morning.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses are:
- Risk for impaired skin integrity related to intense perianal scratching.
- Acute pain related to smooth muscle spasm secondary to migration of parasites in the stomach.
- Imbalanced Nutrition: less than body requirements related to anorexia and vomiting.
- Hyperthermia related to decrease in circulation secondary to dehydration.
Nursing Care Planning and Goals
The major goals for a child with Enterobiasis are:
- Reduce discomfort from perianal itching.
- Diminish pain to a tolerable level.
- Regain adequate nutrition.
- Reduce or eliminate increase in temperature.
Nursing Interventions
The nursing interventions for a child with Enterobiasis are:
- Administer medications as ordered. Drug therapy with pyrantel, mebendazole, or albendazole to destroy the causative parasites. Effective eradication requires treatment of the patient’s family or members of the household.
- Inform patient of the side effects of pyrantel. Stool may be bright red and may cause vomiting. The tablet form of this drug is coated with aspirin and shouldn’t be given to aspirin-sensitive patients.
- Improve skin integrity. Application of an antipruritic ointment or albendazole may help control scratching; keeping the patient’s fingernails trimmed to prevent excoriations is helpful.
- Diminish pain. An antihelminthic medication should be prescribed to patients with enterobiasis.
- Improve hygienic status. Avoid scratching the area and nail-biting because this is a cause of autoinfection; thorough handwashing should be done before and after meals. Tell family not to shake bed linens to avoid aerosolization of eggs that may be found on linens.
- Diminish increase in temperature. Administer antipyretics as prescribed; tepid sponge baths may also be given.
- Inform patient
Evaluation
Goals are met as evidenced by:
- Reduced discomfort from perianal itching.
- Diminished pain to a tolerable level.
- Regained adequate nutrition.
- Diminished increase in temperature.
Documentation Guidelines
Documentation in a patient with enterobiasis includes:
- Individual findings include factors affecting, interactions, the nature of social exchanges, and specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.































Leave a Comment